Study objectives: The intrapleural injection of transforming growth factor (TGF)-[[beta].sub.2] produces pleurodesis in rabbits associated with large pleural effusions. This study investigated whether anti-vascular endothelial growth factor (VEGF) antibody has any effect on the fluid production or the pleurodesis induced by TGF-[[beta].sub.2].
Interventions and measurements: Three groups of seven New Zealand white rabbits were administered TGF-[[beta].sub.2] 5.0 [micro]g intrapleurally. Two groups received anti-VEGF antibody (10 mg/kg and 25 mg/kg) IV 24 h before TGF-[[beta].sub.2] injection, and the third group received no antibody. The rabbits were killed at 2 weeks, and the macroscopic pleurodesis score was determined. The degree of pleural angiogenesis was assessed by immunohistochemical staining for factor VIII.
Results: The administration of anti-VEGF antibodies had no significant effect on the pleural fluid volume or the characteristics of the fluid. The mean pleurodesis score of the seven rabbits in the control group (7.71 [+ or -] 0.76) was significantly (p < 0.05) higher than that for seven rabbits in the low-dose treatment group (4.43 [+ or -] 2.37) and the seven rabbits in the high-dose treatment group (4.57 [+ or -] 2.36) [[+ or -] ]. The percentage of pleural tissue demonstrating angiogenesis in the control group (4.87 [+ or -] 0.43%) was significantly (p < 0.05) higher than that for the low-dose (2.94 [+ or -] 0.68%) or high-dose (2.67 [+ or -] 0.64%) antibody groups. When all rabbits were considered, there was a highly significant correlation between the pleural vascular density scores and the pleurodesis scores (r = 0.84, p < 0.01).
Conclusion: VEGF and angiogenesis appear to play a pivotal role in the production of a pleurodesis.
Key words: angiogenesis; pleura; pleurodesis; transforming growth factor-[[beta].sub.2]; vascular endothelial growth factor
Abbreviations: LDH = lactate dehydrogenase; TGF = transforming growth factor; VEGF = anti-vascular endothelial growth factor
**********
Chemical pleurodesis is an important method for managing recurrent pleural effusions and pneumothoraces, (1,2) Pleurodesis occurs when pleural fibrosis is induced, and symphysis develops between the visceral and parietal pleurae to obliterate the pleural space. The intrapleural administration of transforming growth factor (TGF)-[[beta].sub.2], a profibrotic cytokine, produces an excellent pleurodesis in animals. (3-5) Although TGF-[[beta].sub.2] induced a pleurodesis at least as effectively as did talc and doxycycline, the intrapleural administration of TGF-[[beta].sub.2] induced a much larger volume of pleural fluid in the first few days. The fluid was characterized by low protein and lactate dehydrogenase (LDH) levels, and low WBC counts. (3) The increased fluid production may be due to increased levels of vascular endothelial growth factor (VEGF) in the pleural fluid. We previously demonstrated that the intrapleural injection of TGF-[[beta].sub.2] induced a dose-dependent increase in the pleura] fluid VEGF levels in rabbits. (6) In addition, the level of VEGF in the pleura] fluid correlated significantly with the volume of the pleura] effusion. (6) In vitro, the addition of TGF-[[beta].sub.2] to cultured pleural mesothelial cells induced a dose-dependent increase in VEGF production. (6) Given these in vivo and in vitro experimental data, we postulated that VEGF is responsible for the increased pleural fluid production after the intrapleural administration of TGF-[[beta].sub.2].
VEGF, also known as the vascular permeability factor, is all important angiogenic cytokine. VEGF also increases vascular permeability. (7,8) It is likely that VEGF plays an important role in pleural fluid formation. (9,10) In humans, pleura] fluid VEGF levels were significantly higher in exudates than in transudates. (9) Moreover, VEGF receptors are present at high density in both the normal and diseased pleura. (10) Further evidence of the role of VEGF in pleural diseases comes from studies on VEGF antagonists. VEGF receptor phosphorylation blockade inhibits the formation of malignant effusions in mice with lung adenocarcinomas. (11) An in vitro study (12) reported that anti-VEGF antibodies negate the Staphylococcus aureus-induced increased VEGF production in mesothelial cells and the subsequent increase in mesothelial permeability.
The aim of the present study was to evaluate the effect of anti-VEGF antibody on the volume and characteristics of pleura] fluid and the degree of pleurodesis after intrapleural administration of TGF-[[beta].sub.2]. We hypothesized that the systemic administration of anti-VEGF antibody would result in a reduction in the amount of pleural fluid production and would have no effect on the degree of pleurodesis.
MATERIALS AND METHODS
TGF-[[beta].sub.2] and Anti-VEGF Antibody
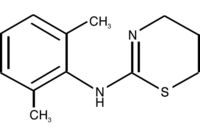
Recombinant human TGF-[[beta].sub.2] produced in Chinese hamster ovary cells was obtained from Genzyme Corporation (Framingham, MA), as we previously described. (3-6) TGF-[[beta].sub.2] was formulated in a vehicle consisting of 20 mmol/L sodium phosphate, 130 mmol/L sodium chloride, 15% (weight/weight) propylene glycol, and 20% (weight/weight) polyethylene glycol 400 at a pH of 7.2. Recombinant human monoclonal anti-VEGF antibody was provided by Genentech (San Francisco, CA) in a 4-mL vial containing 25 mg/mL anti-VEGF antibody (25 mg/mL, 4 mL per vial).
Animal Experiment
The study protocol was approved by the Vanderbilt University Institutional Animal Care and Use Committee. The method used was similar to that described in our previous studies, (3,4,6) New Zealand white rabbits weighing 1.5 to 2.0 kg were anesthetized with an IM injection of 35 mg/kg of ketamine hydrochloride (Fort Dodge Animal Health Laboratories; Fort Dodge, IA) and 5 mg/kg of xylazine hydrochloride (Fermenta; Kansas City, MO). The chest was shaved, and the skin was sterilized with 10% povidone iodine (Baxter; Deerfield, IL). The rabbit was placed in the left lateral decubitus position, and a small (< 3 cm) skin incision was made midway between the tip of the scapula and the sternum approximately 2 cm above the right costal margin. A chest tube (silicone tube, 0.062-inch internal diameter and 0.125-inch outer diameter; Braintree Scientific; Braintree, MA) with three extra openings near its distal end to enhance drainage was inserted by blunt dissection into the right pleural cavity. The chest tube was secured at the muscle layers with a purse-string suture. The proximal end of the chest tube was then tunneled underneath the skin and drawn out through the skin posteriorly and superiorly between the two scapulae. A three-way stopcock was attached to the end of the chest tube via an adapter through which any pleural air was evacuated. With the tube clamped, the three-way stopcock was then removed from the chest tube and replaced by a capped one-way valve (Medexinc; Hilliard, OH). The chest tube, cap, and one-way valve were sutured to the skin. Any pleural fluid that accumulated during the experiment could be aspirated via the one-way valve. The left pleural cavity was used for control.
Twenty-one rabbits were placed into three groups of 7 rabbits each. All the rabbits received TGF-[[beta].sub.2] 5.0 [micro]g in 2.5 mL intrapleurally 24 h after chest tube placement. Injection of the TGF-[[beta].sub.2] was followed immediately by an injection of 1.0 mL of 0.9% sodium chloride solution to clear the dead space of the chest tube. Rabbits in the high-dose antibody group received 25 mg/kg anti-VEGF antibody IV 24 h before the intrapleural administration of TGF-[[beta].sub.2]. Rabbits in the low-dose antibody group received 10 mg/kg anti-VEGF antibody IV 24 h before the intrapleural TGF-[[beta].sub.2]. Rabbits in the third group received no anti-VEGF antibody. The dose of TGF-[[beta].sub.2] used was based on the results of our studies (3,4,6) on TGF-[[beta].sub.2]-induced pleurodesis.
After the intrapleural injection, the chest tube was aspirated at 24-h intervals. The volume of the pleural fluid collected was recorded. The protein and LDH levels in the fluid collected after 24 h were determined with an automated analyzer (Johnson & Johnson; Rochester, NY). The upper limit of normal for human serum LDH by this method is 630 U/L. Total leukocyte count was measured using an automated counter (Coulter Electronics; Luton, UK) that was calibrated daily. The first reading was ignored because it frequently varied substantially from the subsequent readings, and the mean of the next three readings was recorded. The chest tube was removed under light sedation when the pleural fluid drainage was < 5 mL over the preceding 24 h.
Fourteen days after the injection of the TGF-[[beta].sub.2], the rabbits were sedated and then killed with carbon dioxide inhalation. The thorax was removed en bloc. The lungs were expanded by the injection of 50 mL of 10% neutral-buffered formalin into the exposed trachea via a plastic catheter (6 mm in diameter). The trachea was then lighted and the entire thorax submerged into 10% neutral-buffered formalin solution for at least 48 h before the pleurodesis was graded.
Pleurodesis Scoring Scheme
The pleural cavity was carefully exposed using methodology previously described. (3,4,6) A consensus grading of the macroscopic pleurodesis was reached by two investigators (K.B.L. and R.W.L.), who were blinded with respect to the treatment group using the semiquantitative scheme described below. Both graders were present when the thorax was opened, and alter discussion a consensus grade was agreed on. Any evidence of hemothorax, infection, or empyema was recorded.
Grading of Pleurodesis Score
The degree of pleurodesis was graded on a scale of 1 to 8 as described in our previous studies. (4,13-15) Adhesions were defined as fibrous connections between the visceral and parietal pleura. Symphysis was present if the visceral and parietal pleura were difficult to separate as a result of adhesions. The degree of pleurodesis was graded as follows: 1 = no adhesions between the visceral and parietal pleura; 2 = rare adhesions between the visceral and parietal pleura with no symphysis; 3 = a few scattered adhesions between the visceral and parietal pleura with no symphysis; 4 = many adhesions between the visceral and parietal pleura with no symphysis; 5 = many adhesions between the visceral and parietal pleura with symphysis involving < 5% of the hemithorax; 6 = many adhesions between the visceral and parietal pleura with symphysis involving 5 to 25% of the hemithorax; 7 = many adhesions between the visceral and parietal pleura with symphysis involving 25 to 50% of the hemithorax; and 8 = many adhesions between the visceral and parietal pleura with symphysis involving > 50% of the hemithorax.
Microscopic Examination of the Pleura
Histologic and Immunohistologic Staining Preparation: At the time, the pleura was evaluated grossly, samples of the parietal pleura, and lung from each hemithorax were obtained and fixed in 10% neutral buffered formalin at room temperature. After a minimum of 48 h, tissues were embedded in paraffin blocks. Representative sections (6 [micro]m) were stained with hematoxylineosin for histologic examination. For immunohistochemical staining, sections were deparaffinized and rehydrated through a graded alcohol series to phosphate-buffered saline solution. Endogenous peroxidase activity was inactivated by treating with 3% hydrogen peroxide in aqueous methanol for 20 min at room temperature followed by Tris-buffered saline solution with 0.1% Tween rinses.
Immunohistochemical Analysis for Factor VIII: The degree of pleural angiogenesis (vascular density) was evaluated by immunohistochemical staining. (16) To selectively highlight all endothelial cells within pleural areas for the purpose of automated morphometric analysis, sections were immunostained for factor VIII antigen (von Willebrand factor). The sections were incubated with anti-factor VIII (Dako Cytomation; Carpinteria, CA) at a dilution of 1:900 for 30 min. The Dako [Envision.sup.+] System, DAB +/Peroxidase (Dako Cytomation, Carpinteria, CA) was used to produce localized, visible staining. Slides were lightly counter-stained with Mayer hematoxylin, dehydrated, and cover slipped.
Morphometric Analysis Techniques: Image ProPlus software (Media Cybernetics; Silver Springs, MD) was used to analyze tissue sections viewed on the stage of a Vanox light microscopy interfaced via a Progressive Research Digital Camera (Konatron Electronik; Munich, Germany). Two sections randomly selected from each visceral pleural sample were analyzed. Within each section, measurements of 10 random fields were performed, and the mean result was reported. The degree of pleural angiogenesis was semiquantitated by measuring the percent of the area occupied by endothelial cells. Since factor VIII immunostaining selectively highlights only the endothelial components of the pleural tissues, the percentage of the area occupied by microvessels can be assessed via computer-assisted digital analysis. The Image ProPlus color scale was adjusted to recognize brown staining in areas representing immunostained microvessels. (17) The analysis was performed by an observer (Y.B.G.) blinded to the treatment of the rabbit.
Statistical Analysis
All data are presented as mean [+ or -] SD unless otherwise stated. The pleural fluid volume, pleurodesis scores, and pleural vascular density, in three different groups were compared with one-way analysis of variance. Since the pleural fluid WBCs and LDH were not normally distributed, the median values among the treatment groups for these measurements were compared using the Kruskal-Wallis one-way analysis of variance on ranks. The Pearson correlation was used for linear regression analysis. All data were analyzed using statistical software (Sigma Star V2.03; San Rafael, CA). A p value < 0.05 was considered significant.
RESULTS
Pleural Fluid Analysis
The administration of anti-VEGF antibody prior to the injection of TGF-[[beta].sub.2] did not significantly affect the volume of pleural fluid produced (Table 1). Although the mean total amount of fluid produced in the seven rabbits in the control group (35 [+ or -] 31 mL) tended to be greater than that in the seven rabbits in the low-dose antibody group (23 [+ or -] 15 mL) and in the seven rabbits in the high-dose antibody group (18 [+ or -] 15), the differences were not significant (p = 0.28) Moreover, there was no significant difference in the WBC, protein, or LDH levels in the three different groups (Table 1).
Pleurodesis Scores
Administration of anti-VEGF antibodies 24 h prior to the intrapleural instillation of TGF-[[beta].sub.2] resulted in a less effective pleurodesis (Fig 1). The mean pleurodesis score of the control group (7.71 [+ or -] 0.76) was significantly (p < 0.05) higher than that for the low-dose antibody group (4.43 [+ or -] 2.37) and the highdose antibody group (4.,57 [+ or -] 2.36) [Table 2].
[FIGURE 1 OMITTED]
No rabbits died before the time they were to be killed, and there was no evidence of empyema in any rabbit. Two rabbits in the control group had a moderate hemothorax (< 50% of the hemithorax) at necropsy.
Pleural Histology Vascular Density
The vascular density in the visceral pleura of the rabbits that received the anti-VEGF antibodies was noticeably diminished on both the hematoxylin-eosin-stained sections and the sections selectively immunostained with the endothelial marker (factor VIII). By contrast, pleural tissues from control rabbits showed numerous dilated microvessels. Semiquantitation by computer-assisted digital analysis of the percentage of visceral pleural occupied by tissues immunostained with factor VIII showed that the groups pretreated with anti-VEGF antibody had a significantly (p < 0.05) lower percentage of their pleural tissues staining positive for factor VIII (Fig 2). The pleural vascular density of the control group (4.87 [+ or -] 0.43%) was significantly (p < 0.05) higher than that for the low-dose antibody treatment group (2.94 [+ or -] 0.68%) and the high-dose antibody treatment group (2.67 [+ or -] 0.64%). When all 21 rabbits were considered, there was a highly significant correlation between the visceral pleural vascular density scores and the pleurodesis scores (r = 0.835, p < 0.01) [Fig 3].
[FIGURES 2-3 OMITTED]
DISCUSSION
The intrapleural injection of TGF-[[beta].sub.2] induced a large volume of pleural fluid formation in the first 24 h. The administration of anti-VEGF antibodies 24 h prior to the TGF-[[beta].sub.2] administration did not significantly affect the amount of fluid. However, the administration of the anti-VEGF antibody significantly inhibited the pleurodesis induced by the TGF-[[beta].sub.2]. Moreover, the administration of the anti-VEGF antibodies significantly reduced the amount of angiogenesis in the pleura. When all rabbits were considered together, the amount of angiogenesis was closely correlated with the pleurodesis score. These findings suggest that angiogenesis is important for the production of a pleurodesis induced by intrapleural TGF-[[beta].sub.2].
We have previously shown that the intrapleural injection of TGF-[[beta].sub.2] results in an effective pleurodesis that is often associated with the production of large amounts of pleural fluid in the first few days after injection. (3,4) We have also demonstrated that TGF-[[beta].sub.2] induces a dose-dependent VEGF release from cultured pleural mesothelial cells. (6) The basal mesothelial production of VEGF is reduced in the presence of anti-TGF-[beta] antibodies, implying that basal VEGF elaboration from mesothelial cells is in part due to endogenous TGF-[beta]. (6) TGF-[beta] also induces VEGF in vivo. The intrapleural injection of TGF-[beta].sub.2] in rabbits stimulates VEGF production in a dose-dependent manner. (6) The pleural fluid VEGF concentration correlates significantly with the volume of effusion induced. (6) The pleural fluid VEGF level is 70-fold higher than the corresponding plasma levels, supporting the contention that VEGF is produced by cells within the pleural cavity. (6) In human pleural effusions, the levels of TGF-[[beta].sub.1] and TGF-[[beta].sub.2] both correlate significantly with the levels of VEGF. (18) Given the in vivo and in vitro experimental data, it is reasonable to suggest that TGF-[beta] contributes to the VEGF aceulnulation in pleural effusions.
A role of VEGF in pleural fluid formation is supported by data from clinical studies and from animal models. (19-21) VEGF is the most potent cytokine known for increasing vascular permeability. (8) In addition, VEGF is a potent stimulator of angiogenesis. These two functions of VEGF probably result in a large flux of water and macromolecules from the vasculature to the pleural space when there are elevated levels of VEGF in the pleural space. In humans, pleural fluid VEGF levels were significantly higher in exudates than in transduates. (9) Kraft et al (22) showed that the VEGF levels in malignant pleural and peritoneal effusions were up to 10-fold higher than those in the corresponding serum, indicating that local production, rather than diffusion from serum, is the main source of VEGF in these effusions. Fms-like tyrosine kinase-1 receptors for VEGF are present at high density in both healthy and inflammatory pleural tissues. (10) Further evidence of the role of VEGF in pleural fluid formation comes from studies on VEGF antagonists. VEGF receptor phosphorylation blockade inhibits the formation of malignant effusion in mice with lung adenoeareinomas. (11) Anti-VEGF antibodies negate the S aureus-induced production of VEGF by mesothelial cells and the subsequent increase in mesothelial permeability in vitro. (12) All of the above evidence suggests that VEGF is an important factor in pleural fluid formation.
Since our group had observed that the intrapleural administration of TGF-[[beta].sub.2] causes pleural effusions and it is known that TGF-[[beta].sub.2] stimulates VEGF production from pleural mesothelial cells, (6) we expected that the administration of anti-VEGF antibodies would reduce the amount of pleural fluid formed after TGF-[[beta].sub.2] was administered intrapleurally. However, in the present study, the administration of anti-VEGF antibodies did not have a significant effect on the amount of pleural fluid formed. A clinical trial (23) of recombinant human monoclonal anti-VEGF antibody as adjunct therapy for inoperable non-small cell lung cancer also showed no definite benefit on the evolution of pleural effusions.
Why didn't anti-VEGF antibody significantly decrease the pleural fluid formation after TGF-[[beta].sub.2] injection? There are four possible explanations. First, the anti-VEGF antibody used in the present study is a human antibody, and it might not neutralize the rabbit VEGF. We feel that this explanation is unlikely because there was a definite effect of the anti-VEGF antibody on pleurodesis and angiogenesis. Moreover, Yoshida et al (24) reported that administration of the same anti-VEGF antibody blocked tumor necrosis factor-[alpha]-induced angiogenesis in the rabbit cornea in vivo. Second, it is possible that the anti-VEGF antibodies did not enter the pleural space. This explanation is again unlikely because the anti-VEGF antibodies did affect the pleurodesis. However, it is possible that when the TGF-[[beta].sub.2] was injected and the pleura was normal, a significant amount of anti-VEGF antibody did not enter the pleural space. Third, there was a definite tendency for there to be less fluid production in the groups that received the anti-VEGF antibodies (Table 1). The power of the test in this experiment was < 0.50. If we had tripled the number of animals, the power of the test with the numbers we observed in the first set of animals would have given us a power of approximately 0.80 to detect a significant difference. Fourth, other factors with fimctions similar to those of VEGF might be responsible for the increase in pleural fluid formation.
Normal angiogenesis, which is self-limiting and strictly regulated, is important during wound healing as well as during the formation of the endometrium, corpus luteum, and placenta. Angiogenesis is also involved in various pathologic inflammatory and angiogenie diseases, including psoriasis, rheumatoid arthritis, diabetic retinopathy, arteriosclerosis, and solid tumors. (25,26) The development of new blood vessels depends on angiogenie factors, such as VEGF, acidic fibroblast growth factor, basic fibroblast growth factor, angiogenin, placenta growth factor, epidermal growth factor/transforming growth factor-[alpha], hepatocyte growth factor, and plasminogen activators. (26)
The exact mechanism responsible for pleurodesis remains unknown. Previous reviews (2,27,28) have not emphasized the role of angiogenesis in pleurodesis. It is thought that when sclerosing agents are injected into the pleural space, they injure the mesothelial cells lining the pleural space. As a result of the injury, pleural inflammation develops usually in association with a transient pleural effusion. If the injury is sufficiently severe, intrapleural fibrosis will develop and the visceral and parietal pleurae will tuse producing a pleurodesis. (2,29,30) A previous study by Hurewitz and coworkers (31) noted that as the pleural inflammation continued, neovascularization developed and was prominent on the surfaces of the visceral and parietal pleurae. We have found that when doxycycline is administered intrapleurally in rabbits without chest tube placement, there is a high incidence of hemothorax that is fatal in a significant proportion of the animals. (32) In the past, we hypothesized that the hemothoraees were due to rupture of fragile capillaries associated with neovascularization. (32) In the present study, only animals in the control group had a hemothorax. This observation provides support for the hypothesis that the hemothoraces are associated with angiogenesis. Both rabbits with hemothoraees had a pleurodesis score of 8. If these two animals were eliminated from the statistical analysis, the conclusions did not change.
It is well known that VEGF is a potent angiogenic agent. (33,34) The present study demonstrated that anti-VEGF antibody decreased pleural angiogenesis. In addition, the present study demonstrated that anti-VEGF antibodies decreased the effectiveness of pleurodesis following TGF-[[beta].sub.2]. Moreover, when all rabbits were considered, there was a high correlation (r = 0.84) between the pleurodesis score and the percent of the pleura occupied by new vessels. These observations suggest that angiogenesis is important in the production of pleurodesis at least after the intrapleural administration of TGF-[[beta].sub.2]. It remains to be seen whether anti-VEGF antibodies will inhibit the pleurodesis resulting from the intrapleural administration of other agents.
What are the clinical implications of the present study? It is believed that angiogenesis is crucial for the growth of malignancies. (25) Indeed, agents that act as anti-VEGF agents are now being used in the treatment of several different tumors. (11,35,36) It is likely that in the future additional agents that inhibit angiogenesis will be used for chemotherapy of tumors. The present study suggests that one should probably not attempt to create a pleurodesis when the patient is receiving an agent that inhibits angiogenesis.
In conclusion, the present study demonstrates that the IV administration of anti-VEGF antibodies prior to the intrapleural instillation of TGF-[[beta].sub.2] significantly inhibits the resulting pleurodesis and decreases the amount of angiogenesis in the pleural tissues. The degree of pleurodesis is highly correlated with the angiogenesis score. These observations suggest that angiogenesis is important for the production of a pleurodesis.
ACKNOWLEDGMENT: We thank Genenteeh Inc., San Francisco, CA, for providing the antibody; and Lillian B. Nanney, PhD, and Ms. Nancy L. Cardwell for their technical support in using the ilnaging software.
REFERENCES
(1) Light RW, Vargas FS. Pleural sclerosis for the treatment of pneumothorax and pleural effusion. Lnng 1997; 175:213-223
(2) Light RW. Pleural diseases. 4th ed. Philadelphia, PA: Lippincott Williams & Willdns, 2001
(3) Light RW, Cheng DS, Lee YCG, et al. A single intrapleural injection of transforming growth factor [beta]-2 produces an excellent pleurodesis in rabbits. Ann J Respir Crit Care Med 2000; 162:98-104
(4) Lee YCC, Teixeira LR, Devin CJ, et al. Transforming growth factor-[[beta].sub.2] induces pleurodesis significantly faster than talc. Am J Respir Crit Care Med 2000; 163:640-644
(5) Lee YCG, Lane KB, Parker RE, et al. Transforming growth factor [beta]-2 (TGF[[beta].sub.2]) produces effective pleurodesis in sheep with no systemic colnplications. Thorax 2000; 55:1058-1062
(6) Lee YCG, Melkerneker D, Thompson PJ, et al. Transforming growth factor [beta] induces vascular endothelial growth factor elaboration from pleural mesothelial cells in vivo and in in vitro. Am J Respir Crit Care Med 2002; 165:88-94
(7) Breier G, Albrecht U, Sterrer S, et al. Expression of vascular endotbelial growth factor during angiogenesis and endothelial cell differentiation. Development 1992; 114:521-532
(8) Ferrara N. Molecular and biological properties of vascular endothelial growth factor. J Mol Med 1999; 77:527-543
(9) Cheng DS, Rodriguez RM, Perkett EA, et al. Vascular endothelial growth factor in pleural fluid. Chest 1999; 116: 760-765
(10) Thickett DR, Armstrong L, Millar AB. Vascular endothelial grow factor (VEGF) in inflammatory and malignant pleural effusion. Thorax 1999; 54:707-710
(11) Yano S, Herbst RS, Shinohara H, et al. Treatment for malignant pleural effusion of human lung adenocarcinoma by inhibition of vascular endothelial growth factor receptor tyrosine kinase phosphorylation. Clin Cancer Res 2000; 6:957-965
(12) Mohammed KA, Nasreen N, Hardwiek J, et al. Bacterial induction of pleural mesothelial monolayer barrier dysfunction. Am J Physiol Lung Cell Mol Physiol 2001; 281:L119-L125
(13) Lee YC, Yasay JR, Johnson JE, et al. Comparing transforming growth factor-[[beta]2], talc and bleomyein as pleurodesing agents in sheep. Respirology 2002; 7:209-216
(14) Lee YC, Malkemeker D, Devin CJ, et al. Comparing transforming growth factor [beta]-2 and fibronectin as pleurodesing agents. Respirology 2001; 6:281-286
(15) Lee YC, Devin CJ, Teixeira LR, et al. Transforming growth factor [beta]2 induced pleurodesis is not inhibited by corticosteroids. Thorax 2001; 56:643-648
(16) Detmar M, Crown LF, Schon MP, et al. Increased microvascular density and enhanced leukocyte rolling and adhesion in the skin ofVEGF transgenesis mice. J Invest Dermatol 1998; 111:1-6
(17) Nanney LB, Wamil BD, Whitsitt J, et al. CM101 stimulates cutaneous wound healing through an anti-angiogenic mechanism. Angiogenesis 2001; 4:61-70
(18) Cheng D, Lee YC, Rogers JT, et al. Vascular endothelial growth factor level correlates with transforming growth factor-[beta] isoform levels in pleural effusions. Chest 2000; 118: 1747-1753
(19) Yeo K-T, Wang HH, Nagy JA, et al. Vascular permeability factor (vascular endothelial growth factor) in guinea pig and human tumor and inflammatory effusions. Cancer Res 1993; 53:2912-2918
(20) Yano S, Shinohara H, Herbst RS, et al. Production of experimental malignant pleural effusions is dependent on invasion of the pleura and expression of vascular endothelial growth factor/vascular permeability factor by human lung cancer cells. Am J Pathol 2000; 157:1893-1903
(21) Grove CS, Lee YC. Vascular endothelial growth factor: the key mediator in pleural effusion formation. Curr Opin Pulm Med 2002; 8:294-301
(22) Kraft A, Weindel K, Ochs A. Vascular endothelial growth factor in the sera and effusions of patients with malignant and nonmalignant disease. Cancer 1999; 85:178-187
(23) Lee YCG, Devote R, Novotny W, et al. The effects of recombinant human monoclonal antibodies against vascular endothelial growth factor on maliguant pleural effusions in patients with non-small cell lung carcinoma [abstract]. Chest 2001; 120(suppl):193S
(24) Yoshida S, Ono M, Shono T. Involvement of interleukin-8, vascular endothelial growth factor, and basic fibroblast growth factor in tumor necrosis factor a-dependent angiogenesis. Mol Cell Biol 1997; 17:4015-4023
(25) Folkman J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat Med 1995; 1:27-31
(26) Folkman J, Klagsbrun M. Angiogenic factors. Science 1987; 235:442-447
(27) Hurewitz AN, Wu CL, Mancuso P. Tetracycline and doxycycline inhibit pleural fluid metalloproteinases: a possible mechanism for chemical pleurodesis. Chest 1993; 103:1113-1117
(28) Light RW, Vargas FS. Pleural sclerosis for the treatment of pnemnothorax and pleural effusion. Lung 1997; 175:213-223
(29) Sahn SA, Good JT. The effect of common sclerosing agents on tbe rabbit pleural space. Am Rev Respir Dis 1981; 124:65-67
(30) Miller EJ, Kajikawa O, Pueblitz S, et al. Chemokine involvement in tetracycline-induced pleuritis. Eur Respir J 1999; 14:1387-1393
(31) Hurewitz AN, Lidonicci K, Wu CL. Histologic changes of doxycycline pleurodesis in rabbits: effect of concentration and pH. Chest 1994; 106:1241-1245
(32) Wu W, Teixeira LR, Light RW. Doxycycline pleurodesis in rabbits: comparison of results with and without chest tube. Chest 1998; 114:563-568
(33) Ferrara N. Role of vascular endothelial growth factor in regulation of physiological angiogenesis. Am J Physiol Cell Physiol 2001; 280:C1358-C1366
(34) Ferrara N. VEGF: an update on biological and therapeutic aspects. Curr Opin Biotechnol 2000; 11:617-624
(35) Schlaeppi JM, Wood JM. Targeting vascular endothelial growth fhctor (VEGF) for anti-tumor therapy, by anti-VEGF neutralizing monoclonal antibodies or by VEGF receptor tyxosine-kinase inhibitors. Cancer Metast Rev 1999; 18:473-481
(36) Yang JC, Haworth L, Sherry RM, et al. A randomized trial of bevacizumab, an anti-vascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med 2003; 349:427-434
* From the Department of Respiratory and Critical Care Medicine (Dr. Guo), the First Affiliated Hospital of Sun Yat-sen University, Guangzhou, ROC; Department of Critical Care and Pulmonary Services (Dr. Kalomenidis), Athens Medical School, Evangelismos Hospital, Athens, Greece; Mouse Pathology and Immunostaining Core Facility (Ms. Parman), Vanderbilt University Medical Center, Nashville TN. and Department of Pulmonary Medicine (Drs. Hawthorne, Lane, and Light), St. Thomas Hospital and Vanderbilt University, Nashville, TN. This work was presented in part at the American College of Chest Physicians annual meeting, Orlando, FL, October 2003. Supported in part by the Saint Thomas Foundation, Nashville, TN.
Manuscript received November 22, 2004; revision accepted February 4, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Richard W. Light, MD, FCCP, Department of Pulmonary Medicine, St. Thomas Hospital, 4220 Harding Rd, Nashville, TN 37205; e-mail: rlight98@yahoo.com
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group