Objectives: Circumventricular organs (CVOs) are fine, periventricular, neurotransmitter-rich structures that are devoid of a blood-brain barrier and are known for their secretory role controlling fluid and electrolyte balance, thirst and even reproduction. Common pathologies of the brain such as trauma or bleeding affect CVOs, and hence their function. However, at what stage of these disease processes are CVOs affected and the time sequence of their recovery is still not clear. The aim of this study was to detect the morphological changes in CVOs using electron microscopy after experimental subarachnoid hemorrhage (SAH).
Methods: Experimental SAH was induced by transclival puncture of the basilar artery. Both scanning and transmission electron microscopic examination of the representive sections from each CVO was undertaken.
Results: Electron microscopy has shown that after SAH, the cells that form the CVOs exhibit signs of cellular necrosis with margination of the nucleus as well as cytoplasmic, mitochondrial and axonal edema. The subfornicial organ and organum vasculosum lamina terminalis appear to be more vulnerable to the effects of SAH than the median eminence or area postrema.
Discussion: Considering the fact that the experimental SAH model we have used is very similar to the momentary rupture of an aneurysm with secondary reflex spasm to seal the hole, it will not be unrealistic to consider that similar effects may also take place in the clinical setting. [Neurol Res 2005; 27: 580-585]
Keywords: Circumventricular organ; subarachnoid hemorrhage; necrosis
INTRODUCTION
Circumventricular organs (CVOs), located around the brain ventricles, are fine structures subserving important physiological events such as fluid and electrolyte balance, the feeling of thirst and other neuroendocrine functions like libido and reproduction. Originally based on post-mortem findings and/or personal observations, the role of the brain in the regulation of other hormone systems, such as the pituitary, has been known since the end of 19th century. The first to conduct experiments concerning this were Hume from the US1 and Harris from the UK2. Both groups of researchers found that the hypothalamus had a regulatory role over the anterior pituitary. Around the same time Scharrer (1954)3 had shown that numerous differentiated neuronal cell groups capable of hormone or transmitter secretion other than those in the anterior hypothalamus existed. One of the most exciting findings in neuroendocrinology has been the intrinsic or brain angiotensin system exerting a central control over fluid and electrolyte balance, which was long believed to be controlled only by renal-suprarenal gland interaction. These specific cellular groups that form the brain angiotensin system are located at CVOs. These tiny organs do not have a blood-brain barrier (BBB). The capillary endothelial cell membranes and junctions are ready for the secretory function4,5. The brain angiotensin system not only directs the lower systems subserving fluid and electrolyte balance, but also contributes to the regulation of blood pressure and reproductive functions. The area postrema (AP), median eminence (ME), organum vasculosum lamina terminalis (OVLT), subfornicial organ (SFO), pineal gland, posterior pituitary and the subcomissural organs (SCO) are all located around the ventricular system, particularly the third ventricle, and have a common function that is mediated by means of neurotransmitters. Although scattered anatomically, thes organs are grouped as the CVOs.
After subarachnoid hemorrhage (SAH), significant changes occur in blood pressure, cardiac rhythm, extracellular electrolyte concentrations and the permeability of the kidneys. Brain ischemia and/or damage occurs both due to a direct irritative effect of blood breakdown products on the blood vessel wall leading to spasm or vasculopathy and also due to the activation of central and peripheral adrenergic systems in an effort to maintain perfusion. Spasm of the small perforating hypothalamic branches often leads to hypoperfusion of the anterior hypothalamic area, which in turn leads to temporary or permanent hypothalamic damage. Hypoperfusion of the posterior hypothalamus releases the central control over the brain angiotensin system and this stimulates the peripheral angiotensin system, triggering further vasoconstriction. This must be why patients with a high plasma renin activity and/or high urinary cathecolamine levels after SAH have been found to have poor prognosis6. We have previously shown that SAH7 and hydrocephalus8 caused increases in the receptor content at CVOs in rats. In light of our previous findings pointing to an up-regulation of angiotensin receptors in the CVOs after SAH, we wished to know what kind of ultrastructural changes occurred in the CVOs after SAH.
MATERIALS AND METHODS
Experiments were carried out at the microsurgery laboratory of the Medical and Surgical Research Center of Zonguldak Karaelmas University. Electron microscopic analysis was carried out at the Anatomy Department of Hacettepe University, Ankara.
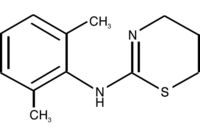
Twenty white albino male rats weighing 250-300 g were anesthetized by an intramuscular (i.m.) injection of 5 mg/kg ketamine HCl (Ketalar, Parke-Davis/ Eczacibasi, Istanbul) and 10 mg/kg xylazine (Rompun, Bayer, Istanbul). The surgical procedure was performed using an operating microscope (Opmi-1, Zeiss, Germany). SAH was created with a technique similar to that described by Barry et al.8,9. Briefly, through a midline cervical incision in the supine position, the clivus was exposed using the anterior parapharyngeal approach. A bony window in front of the basilar artery was created using large bore needles with immaculate care not to open the prepontine cistern. A suture needle with an outer diameter of 75 µm (Ethicon, Scotland, UK) was inserted into the basilar artery. The withdrawal of the needle caused an extensive hemorrhage into the subarachnoid space with an even distribution up to the olfactory area (Figure 1).
For electron microscopy, one animal was considered to represent the normal morphology for scanning electron microscopic (SEM) examination. The animals with SAH in the SEM group were not perfused and were only decapitated. The animals in the transmission electron microscopy (TEM) group were anesthetized by an intraperitoneal (i.p.) injection of 100 mg sodium thiopentone (Pentothal, Abbott, Istanbul). After thoracotomy, the left ventricle was cannulated, the descending aorta clamped and the blood washed from the head and cervical regions with Ringer lactate solution after section of the vena cava. The bloodstream was then perfused with a fixation fluid (3% paraformaldehyde and 1% glutaraldehyde in PFS) until the heart stopped. After fixation in situ for 1 hour, the objects were decapitated and accurate representative specimens, each ~2 mm^sup 3^ in volume, were obtained from the SFO, ME, OVLT and AP using a rat sterotaxic atlas. The tissues for TEM were fixed in 2.5% glutaraldehyde solution in phosphate buffer at 4°C for 24 hours and then post-fixed for 1 hour in 2% osmium tetroxide in buffer at 4°C. The samples were dehydrated in ascending solutions of alcohol, pre-treated with propylene oxide and araldite mixture, embedded in araldite resin, cut with an LKB ultramicrotome, mounted on copper grids, stained with uranyl acetate and Reynold's lead citrate, and examined with a JEM 1200 (JEOL, Japan) transmission electron microscope. For SEM, the brains were removed without perfusion and 2 cm^sup 3^ specimens from the CVOs were obtained fresh using a rat stereotaxic atlas. The specimens were immediately inserted into phosphate-buffered 2.5% glutaraldehyde solution at 4°C. After an initial 24-hour fixation, the tissue specimens were washed 3-4 times with Sorenson's buffer solution (20% 1/15 M Na^sub 2^HPO^sub 4^ and 80% 1/15 M KH^sub 2^PO4, pH 7.38). After cleansing, the tissues were post-fixed for 1 hour in 2% osmium tetroxide. The tissues were again washed with Sorenson's solution for 15 minutes before being critical-point dried and gold-coated. The tissues were examined with a JEM 1200 (JEOL, Japan) scanning electron microscope.
RESULTS
Macroscopic examination of each experimental animal showed blood within all basal cisterns. In the specimens without SAH, fine endothelial structures, normal nuclei and axonal structures were documented in the CVOs using TEM. Few edematous vacuoles were detected in the SFO and AP of normal objects (Figure 2). In control specimens, the SEM showned no red blood cells (RBCs) and very few edematous vacuoles in the perivascular area. In SAH specimens stained for SEM, there were perivascular RBCs (Figure 3a-d). In SAH specimens stained for TEM, there were perivascular RBCs as well as necrosis. The neuronal morphology was preserved especially in the ME. In neurons from the SFO, OVLT and the AP, the nuclear chromatin was displaced paracentrally with necrotic vacuoles in their cytoplasm. The axons were also severely affected. The axonal organelles became edematous. Vascular endothelial lining also became edematous with swollen mitochondria (Figure 4a-d).
DISCUSSION
CVOs are special and separate cell groups that function as an endocrine unit. The capillary structure of CVOs is quite different from that of any other part of the brain. The capillary surface area of CVOs is much less and the capillary endothelial lining more permeable. The endothelial cells of CVOs have 3-7 times more cytoplasmic vacuoles. The number of intercellular junctions is 44% more and wider than an ordinary brain capillary and the cell membrane is thinner. There is 66% less mitochondria in the endothelial cell at CVOs4,10. Their junctions make these cells more permeable to solutes in the plasma.
Ependymal cells at CVOs have a wider range of function as compared with other ependymal cells. The ependymal cells at the subcomissural organ are known to stimulate secretion, whereas the ependymal cells at SFO and OVLT are more involved with transport.
Both the dentrites and the axons of these specialized neurons at CVOs have direct contact with both capillary endothelium and the cerebrospinal fluid (CSF). To connect with the CSF, the dentrites and the axons penetrate the ependyma. In contrast to general ciliated and cuboidal morphology of an ependymal cell, ependymal cells of the CVOs are flat and non-ciliated cells; however, on the other hand, they do have special microvilli to increase the surface area in contact with the CSF. These ependymal cells that neighbor the CVOs and have direct contact with the third ventricle are called tanycytes. Tanycytes, intraventricular projections of the axon terminals, special capillary networks of CVOs all contribute to the final function of the ependyma11,12. In the AP and SFO, the ependymal lining has a rich capillary network in addition to its close contact with the axons and the CSF.
The main problem with analysing the ultrastructural morphology of CVOs is that the capillary structure is not uniform4. Three different capillary structures have been shown at the SFO13. Under pathological conditions it becomes even more difficult to ascertain what has happened to each of these different types. After SAH, changes at the cellular level occur either due to the direct effect of the blood constituents or due to ischemia secondary to the organism's effort for homoestasis. The blood breakdown products in the the subarachnoid space may act either like a neurotoxin and cause diffuse encephalopathy directly14 or encephalopathy arises from diffuse hypoperfusion and/or arterial vasospasm related to spasmogens15-19. Because of the fact that the CVOs are devoid of BBB and also due to their immediate relationship with the CSF, CVOs are highly vulnerable after SAH. Besides the early effects of spasmogens, SAH also has a late detrimental effect through mitogens, which promote proliferation and migration of cellular elements into the subintimal zones of cerebral arteries, i.e. proliferative angiopathy20. Late hypothalamic damage after SAH is often attributed to this latter effect of the SAH.
Several hormones and neurotransmitters including serotonin, catecholamines, prostaglandins and histamine have been held responsible for the delayed ischemic deficits seen after SAH. These spasmogens have been shown to have an effect on the cerebrovascular bed and to decrease the local blood flow and eventually cause a decrease in neural function. Brain angiotensin, an octapeptide, produced at and discharged from the CVOs is another potent vasoconstrictor and acts in a similar way to the above-mentioned spasmogens in the SAH setting. Besides its central direct effect on the local arterial bed, brain angiotensin Il also causes the discharge of norepinephrine from the peripheral adrenergic system and the vascular smooth muscle layer, already made sensitive to the effects of norepineprine by angiotensin II, then constricts and eventually proliferates with necrosis between proliferating layers20. After this initial ischemia, a rapid increase in the intraneuronal Ca^sup 2+^ concentration occurs, with a concomittant decrease in the extracellular Ca^sup 2+^ concentration. Rising intracellular Ca^sup 2+^ activates lipase, protease and endonuclease, and activation of these isoenzymes triggers self-digestion21,22. Free radical formation prevents emergency Ca^sup 2+^ tamponade systems from causing a vicious cycle and accumulation of more intracellular Ca^sup 2+^ inside an already energydepleted mitochondria. The result is cellular death. Our study has shown these ultrastructural changes in CVOs after SAH. The examination of the neuronal structure after SAH has shown both deterioration of cellular organelles and changes in the cytoplasm. The main changes occurred in the endothelial lining and in the perivascular space, with cytoplasmic edema and swelling of all organeiles eventually leading to cellular necrosis23. Damage to the normal neuronal structure was documented in the SFO, AP, OVLT but not in the ME. Previously, we have shown that angiotensin receptor content increased in the SFO and OVLT8 and our present findings coincide with our previous findings. Whether receptor content increase is secondary to the damage of energy mechanisms that hyperpolarize the cell membrane where the receptors are located is not clear. It is also possible that the bulk release of neurotransmitter content into the extracellular space bypassing the normal network between brain and peripheral angiotensin systems, causes a positive feedback. Whatever the mechanisms are, SFO and OVLT appear to be more vulnerable to the effects of SAH than ME or AP. Considering the fact that the experimental SAH model we have used is very similar to the momentary rupture of an aneurysm with secondary reflex spasm to seal the hole, it will not be unrealistic to think that similar effects may also take place in the clinical setting.
ACKNOWLEDGEMENTS
This study was supported by The Scientific and Technical Research Council of Turkey-Health Sciences Research Committee (grant no: SBAC-AYD-373).
REFERENCES
1 Hume DM. The neuro-endocrine response to injury: Present status of the problem Ann Surg 1953; 138: 548-557
2 Harris GW. Pituitary-hypothalamic mehanisms. AMA Arch Neurol Psychiatry 1955; 73: 124-126
3 Scharrer E. Neurosecretion and anterior pituitary in the dog. Experientio 1954; 15: 264-266
4 Gross PM, Sposito NM, Pettersen SE, et al. Differences in function and structure of the capillary endothelium in gray matter, white matter and circumventricular organ of rat brain. Blood Vessels 1986; 23: 261-270
5 Gross PM, Weindl A. Peering through the windows of the brain. J Cereb Blood Flow Metab 1987; 7: 663-672
6 Neil-Dwyer G, Cruickshank JM, Doshi R. The stress response in subarachnoid hemorrhage. Acta Neurochir (Wien) 1990; 47 (Supple.): 102-110
7 Açikgöz B, Akpmar G, Bingöl N, et al. Angiotensin II receptor content within the circumventricular organs increases after experimental hydrocephalus in rats. Acta Neurochir (Wien) 1999; 141: 1095-1099
8 Acikgöz B, Özgen T, Özdogan F, et al. Angiotensin II receptor-content within the subfornical organ and organum vasculosum lamina terminalis increases after experimental subarachnoid hemorrhage in rats. Acta Neurochir (Wien) 1996; 138: 460-465
9 Barry KJ, Gogjian MA, Stein BM. Small animal model for investigation of subarachnoid hemorrhage and cerebral vasospasm. Stroke 1979; 10: 538-541
10 Coomber BL, Stewart PA. Morphometric analysis of CNS microvascular endothelium. Microvasc Res 1985; 30: 99-115
11 Krisch B. lmmunocytochemistry of neuroendocrine systems. Prog Histochem Cytochem 1980; 13: 1-163
12 Weindl A, Joynt RJ. Barrier proporties of the organ. Arch Neurol 1972; 26: 420-426
13 Shaver SW, Sposito NM, Gross PM. Quantitave fine structure of capillaries in subregions of the rat subfornicial organ. J Comp Neurol 1990; 294: 145-152
14 Marzatico F, Gaetani P, Silvani V, et al. Experimental isobaric subarachnoid hemorrhage: Regional mitochondrial function during the acute and late phase. Surg Neurol 1990; 34: 294-300
15 Grubb RL Jr, Raichle ME, Eichling JO, et al. Effects of subarachnoid hemorrhage on cerebral blood volume, blood flow and oxygen utilization in humans. J Neurosurg 1977; 46: 446-453
16 Ishii R. Regional cerebral blood flow in patients with ruptured intracranial aneurysms. J Neurosurg 1979; 50: 587-594
17 Ropper AH, Zervas NT. Outcome 1 year after subarachnoid hemorrhage from cerebral aneurysm. Management morbidity, mortality, and functional status in 112 consecutive good-risk patients. J Neurosurg 1984; 60: 909-915
18 Voldby B, Enevoldsen EM, Jensen FT. Regional CBF, intraventricular pressure, and cerebral metabolism in patients with ruptured intracranial aneurysm. J Neurosurg 1985; 62: 48-58
19 Weir B, Aronyk K. Management, mortality and the timing of surgery for supratentorial aneurysms. J Neurosurg 1981; 54: 146-50
20 Tekkok IH, Tekkok S, Özcan OE, et al. Preventive effect of intracisternal heparin for proliferative angiopathy after experimental subarachnoid haemorrhage in rats. Acta Neurchir (Wien) 1994; 127: 112-117
21 Beal MF. Mitochondria, free radicals, and neurodegeneration. Curr Opin Neurobiol 1996; 6: 661-666
22 Siesjo BK, Siesjo P. Mechanisms of secondary brain injury, Eur J Anaesthesiol 1996; 13: 247-268
23 Martin LJ, Al Abdulla NA, Brambrink AM, et al. Neurodegeneration in excitotoxicity, global cerebral ischemia, and target deprivation: A perspective on the contrbutions of apoptosis and necrosis. Brain Res Bull 1998; 46: 281-309
Gökhan Akpinar*, Bektas Acikgöz[dagger] Selçuk Sürücü[double dagger], H. Hamdi Çelik[double dagger] and Ferda Çagavi[dagger]
* Baymdir Hospital, Department of Neurosurgery, Ankara, Turkey
[dagger] Karaelmas University SoM, Department of Neurosurgery, Zonguldak, Turkey
[double dagger] Hacettepe University SoM, Department of Anatomy, Ankara, Turkey
Correspondence and reprint requests to: Dr Gökhan Akpmar, Bayindir Hastanesi, Beyin ve Sinir Cerrahi Bölümü Sögütözü, Ankara, 06520, Turkey. [gokhanakpinar@superonline.com] Accepted for publication April 2005.
Copyright Maney Publishing Sep 2005
Provided by ProQuest Information and Learning Company. All rights Reserved