Study objectives: Several systemic effects have been described after talc pleurodesis. The aim of this study was to assess the systemic response induced by low, nonpleurodesis-inducing doses of tale and silver nitrate in an experimental model in rabbits.
Design: Groups of six rabbits were injected intrapleurally with tale, 100 mg/kg or 400 mg/kg, and silver nitrate, 0.1% or 0.5%. After 6, 24, or 48 h, samples of blood and pleural fluid were collected and assayed for leukocytes, percentage of neutrophils, lactate dehydrogenase, interleukin-8, and vascular endothelial growth factor (VEGF) levels. Preinjection blood samples were used as normal blood controls.
Measurements and results: Silver nitrate 0.1% induced a more intense pleural inflammation than that produced by talc 100 mg/kg. In contrast, talc 100 mg/kg induced a more pronounced acute systemic response with higher values of WBCs and neutrophils, whereas silver nitrate 0.1% produced no significant increases in leukocytes or neutrophils. The serum interleukin-8 and VEGF levels increased in all groups, and decreased with time only in the silver nitrate 0.1% group. The highest serum VEGF levels were observed in the talc 100 mg/kg group.
Conclusions: In conclusion, 0.1% silver nitrate produced an intense pleural inflammatory response with a less evident systemic response in comparison to 0.5% silver nitrate and talc 100 mg/kg or 400 mg/kg.
Key words: inflammation; pleura; pleural effusion; pleurodesis; silver nitrate; systemic inflammatory response; talc
Abbreviations: IL = interleukin; LDH = lactate dehydrogenase; VEGF = vascular endothelial growth factor
**********
Talc is the agent most commonly used to induce pleurodesis in clinical practice. (1-3) It has been postulated that talc injected into the pleural space may be absorbed and induce systemic inflammatory effects, including fever, arrhythmias, and ARDS. (4) Fever has also been described after intrapleural injection of other pleurodesis agents. (5-21) However, the major concern with talc relates to ARDS. The incidence of ARDS after talc is administered intrapleurally varies from 1.2 to 9%, with a mortality rate as high as 50% in these patients. (22,23)
The mechanism by which talc induces acute systemic effects is poorly understood. Talc particles have been demonstrated in several organs of animals that received doses of talc sufficient to produce a pleurodesis. (24,25) There is also evidence that the risk of adverse effects after talc pleurodesis may be dose related. In fact, when a small dose of talc was injected in rabbits, talc particles were shown only in the ipsilateral lung and mediastinum. (26) Other factors, such as re-expansion pulmonary edema, the absorption of talc particles of small size (< 10 [micro]m), and bacterial contamination may contribute to the development of the systemic inflammatory response. (27) As the adverse side effects related to pleurodesis occur mainly within the first 48 h of the intrapleural injection, studies in this period are most important for understanding the possible role of various mediators in the development and regulation of the inflammatory response.
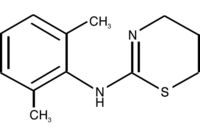
In an attempt to overcome the side effects associated with talc, other pleurodesis agents have been studied. We have focused on silver nitrate, a potent caustic agent. Silver nitrate in the past was used to induce pleurodesis for recurrent pneumothorax with a success rate of 75 to 90% in concentrations varying from 1.0 to 10%. (28-30) We have demonstrated that a lower dose (0.5%) produced pleural fibrosis and pleurodesis similar to that produced by 35 mg/kg of tetracycline (31) and superior to that induced by 400 mg/kg of talc slurry (32) in rabbits, with only minimal microscopic lung damage after long-term observation. (33) In addition, we established that 0.3% silver nitrate was able to induce experimental pleurodesis with minimum damage to the pulmonary parenchyma. (34)
Concerned with the potential side effects produced by the pleurodesis agents injected into the pleural space, we also reported experimentally that both talc and silver nitrate in doses considered effective in inducing pleurodesis (400 mg/kg and 0.5%, respectively) produced a systemic acute inflammatory response with increased levels of WBCs, neutrophils, interleukin (IL)-8, and vascular endothelial growth factor (VEGF). (35) Based on these previous findings, we hypothesized that an intrapleural injection of a low dose of these agents would produce a less intense systemic response than that produced by the higher doses. If this were the case, then one could possibly produce a pleurodesis without the risk of ARD S by injecting low doses of talc or silver nitrate repeatedly.
MATERIALS AND METHODS
Pleural Injection
Seventy-eight white New Zealand male rabbits (13 groups of 6 rabbits) weighing 2.0 to 2.5 kg received intrapleural injections with 3 mL saline solution containing talc, 100 mg/kg or 400 mg/kg (USP Pharmacy; Sao Paulo, Brazil) or silver nitrate, 0.1% or 0.5% (Merck; Darmstadt, Germany). The higher doses of both agents were selected because they have been shown to induce pleurodesis in rabbits, whereas the lower doses induced no pleurodesis. (31,32) The method of pleural injection was described in our previous studies. (31-35) Briefly, the rabbits were anesthetized with ketamine 35 mg/kg (Cristalia; Sao Paulo, Brazil) plus xylazine 5 mg/kg (Bayer; Sao Paulo, Brazil). Then a parasternal, 2-tin chest incision was performed, a 21-gauge needle was inserted through the intercostal muscle for the injection of the solution into the pleural space, and the muscles and skin were sutured with nylon 5-0. Alter 6, 24, or 48 h, the animals received a lethal injection of pentobarbital; immediately before each injection, a blood sample from each animal was collected for comparison with the group of normal, noninjected control animals.
After death, a midline abdominal incision was performed and a 21-gauge needle was inserted through the diaphragm to aspirate the pleural fluid. Blood samples were collected from a group of six noninjected rabbits for controls. The study was approved by the Ethics Committee of the Heart Institute (InCor), University of Sao Paulo Medical School, which oversees research involving both animals and humans.
Reagents
Talc, a magnesium silicate asbestos-free particle with a mean length of 25.4 [micro]m (range, 6.4 to 50.5 [micro]m), was suspended under sterile conditions in endotoxin-free saline solution to provide doses of 100 mg/kg or 400 mg/kg. Silver nitrate was diluted with endotoxin-free water to yield concentrations of 0.1% or 0.5% for intrapleural injection.
Cytologic and Biochemical Analysis
Blood and pleural fluid were collected in ethylenediamine tetra-acetic acid for cytologic and cytokine analysis, and in dry tubes for lactate dehydrogenase (LDH). For the blood cytologic evaluation, samples were processed in an automated hematologic analyzer carrying a specific module for rabbit blood analysis (ADVIA; Bayer, Germany). Pleural fluid samples were placed in a hemocytometer for determination of total leukocytes and onto slides for Leishman preparation and determination of neutrophil percentage. Other samples were centrifuged at 1,000 revolutions per minute for 10 min at 4[degrees]C, withdrawn immediately for LDH analysis and stored at - 80[degrees]C for cytokine determination.
Cytokines Analysis
IL-8 (OptEIA, rabbit IL-8 set; Pharmingen; San Diego, CA) and VEGF (R&D Systems; Minneapolis, MN) were measured by enzyme-linked immunosorbent assay according to the directions of the manufacturer. Quantification of IL-8 and VEGF was done by comparison of the optical density in the enzyme-linked immunosorbent assay reader (PowerWave; Bio-Tek Instruments; Winooski, VT) using a 450-nm filter with the optical density of controls.
Statistical Analysis
Data sets that were not normally distributed were subjected to log transformation. One-way analysis of variance was used to compare the blood and pleural fluid values, and if the log-transformed data did not satisfy normality tests, Kruskal-Wallis one-way analysis of variance on ranks was used. t tests were used to compare the values among subgroups at each time point (tale 100 mg/kg vs silver nitrate 0.1%, talc 100 vs talc 400 mg/kg, and silver nitrate 0.1 vs silver nitrate 0.5%). Statistical analysis was performed using statistical software (SigmaStat; SPSS; San Rafael, CA); p < 0.05 was accepted as significant.
RESULTS
Blood
Leukocytes: Intrapleural injection of both doses of talc and 0.5% silver nitrate led to a significant increase in the peripheral WBC count. The peripheral WBC count after injection of 0.1% silver nitrate at 6 h was nearly identical to the control value. However, only the WBC count at 6 h after injection of talc 400 and 0.5% silver nitrate was significantly higher than control. The WBC count tended to be higher after the higher doses of both agents, but only the higher dose of silver nitrate was significantly higher than the lower dose, with no difference between the doses of talc (Table 1).
Neutrophils: The percentage of blood neutrophils was also increased 6 h after the injection of both doses of talc in comparison to control (Table 1). The neutrophil response decreased along time for both doses of talc. Of note, talc 100 mg/kg had a slower decrease in the neutrophil response in comparison to talc 400 mg/kg. In contrast, injection of silver nitrate 0.1% or 0.5% did not produce a significant neutrophil systemic response. In the comparison among groups, talc 100 mg/kg had a significantly higher neutrophil percentage at all time points than did silver nitrate 0.1%.
LDH: Serum LDH was significantly higher 6 h after injection of talc 100 mg/kg (499 [+ or -] 172 IU/L) and 0.5% silver nitrate (540 [+ or -] 215 IU/L) than after the control (217 [+ or -] 84 IU/L). The increase in serum LDH after all agents had disappeared by 24 h. There was no significant difference in serum LDH between the lower dose of talc and 0.1% silver nitrate (499 [+ or -] 172 IU/L vs 451 [+ or -] 186 IU/L) [data not shown].
IL-8: Serum IL-8 increased after intrapleural injection of all doses of talc and silver nitrate in comparison to control. Serum levels of IL-8 were significantly higher after 0.1% silver nitrate than after talc 100 mg/kg only at 6 h. Serum IL-8 was also greater for silver nitrate 0.5% than after silver nitrate 0.1% at 48 h and talc 400 mg/kg at 6 h and 24 h (Table 2).
VEGF: The findings with VEGF were similar to those with IL-8. Intrapleural injection of different doses of talc and silver nitrate led to significant increases in serum VEGF levels in comparison to control injected animals (< 15 pg/mL). However, the lower dose of talc (100 mg/kg) had a significant higher level of serum VEGF after 48 h than the lower dose of 0.1% silver nitrate (121 [+ or -] 46 pg/mL vs 45 [+ or -] 15 pg/mL; p < 0.05). There was no statistically significant difference between the mean levels of VECF in the higher doses of the talc and silver nitrate groups or between the 0.1% and 0.5% silver nitrate groups (Table 3).
Pleural Fluid
Leukocytes: Mean pleural fluid WBC count was > 20,000/[micro]L in all groups at 6 h and tended to decrease with time. No significant difference was found when the lower and the higher dose of talc were compared. Silver nitrate 0.1% produced a similar response as that of silver nitrate 0.5% only in the first 24 h. After 48 h, the pleural fluid WBC count was higher in the 0.5% silver nitrate group than in all other groups (Table 4).
Neutrophils: Most of the nucleated pleural fluid cells were neutrophils in all treatment groups. With time, the percentage of neutrophils tended to decrease in all groups except silver nitrate 0.5%. There were no significant differences in the mean WBC counts in the two talc groups. The mean percentage of pleural neutrophils in the 0.5% silver nitrate group at 48 h was significantly higher than in all the other groups.
IL-8: Pleural fluid IL-8 levels tended to be higher with the higher doses of both compounds (Table 2). Mean pleural fluid IL-8 tended to be higher after silver nitrate than after talc. Talc 400 mg/kg induced a significantly higher pleural fluid level of IL-8 than talc 100 mg/kg at 6 h and 48 h. Mean pleural fluid IL-8 was significantly higher after the higher dose of silver nitrate at 6 h and 24 h than in all the other groups, and was significantly higher for the 0.1% silver nitrate group than the 100 mg/kg talc group at all time points (p < 0.001).
VEGF: Pleural fluid VEGF levels were greater for the higher doses of both agents in comparison to the lower doses (Table 3). In the talc groups, the difference was significant at 24 h and 48 h and in the silver nitrate groups at all time points. In the comparison between the lower doses of both agents, pleural fluid VEGF was significantly higher for silver nitrate than for talc only at 6 h.
LDH: In general, pleural fluid LDH tended to be higher after silver nitrate than after talc (Table 5). The higher talc dose (400 mg/kg) induced a significantly higher pleural fluid LDH levels at 6 h and 24 h than did the lower dose of talc. Similar to the findings with the cell counts, LDH levels decreased with time in both talc groups and in the 0.1% silver nitrate group. In contrast, LDH levels in the 0.5% silver nitrate group increased with time and after 48 h were significantly higher than the 0.1% silver nitrate group.
Pleural Fluid Volume: Pleural fluid volume tended to be higher in the silver nitrate groups than in the talc groups (Table 5). Even with the lower dose of silver nitrate, the pleural fluid amount was significantly greater than that with either talc dose at 24 h and 48 h. Mean pleural fluid volume was significantly greater for the higher dose of talc at 9.4 h and 48 h in comparison to the lower dose. There was no significant difference between the mean volumes of fluid induced by the two doses of silver nitrate.
DISCUSSION
We have previously shown that the intrapleural injection of both talc and silver nitrate in doses sufficient to produce a pleurodesis in rabbits induced an acute systemic inflammatory response. (35) In the present study, we assessed the blood and pleural response of lower doses of both agents to determine if a lower dose would produce pleural inflammation with a lower systemic response. Talc induced a more pronounced systemic leukocyte response than silver nitrate. In comparison to control, the WBC count was increased significantly only for talc 400 mg/kg at 6 h, whereas the neutrophil percentage was higher for both doses of talc at 6 h. After 24 h, the neutrophil percentage was still elevated in the group of talc 100 mg/kg. Silver nitrate 0.1% induced a less intense leukocyte systemic response, with no significant increase in the WBC count or neutrophil percentage.
The comparison of the noncellular systemic response showed a more intense increase in the LDH levels for talc 100 mg/kg than for talc 400 mg/kg, at levels similar to those produced by the higher dose of silver nitrate. Although 0.1% silver nitrate 'also led to an increase in serum LDH level, it did not differ significantly from control values. The serum IL-8 levels increased in all groups, even with the lower doses of both agents. However, for both doses of talc, the serum IL-8 levels tended to increase with time, in contrast to 0.1% silver nitrate, which had an intense IL-8 response at 6 h that tended to decrease with time. VEGF serum levels were 'also increased in all groups, although the higher serum levels were observed in the talc groups. After 48 h, the talc 100 mg/kg group had significant greater serum VEGF levels than the 0.1% silver nitrate group, whereas there was no significant difference between the levels in the high-dose groups.
The pleural fluid analysis showed an acute WBC and neutrophil response that was similar for both agents. The leukocyte response decreased with time for both doses of talc and for 0.1% silver nitrate. In contrast, 0.5% silver nitrate produced an intense and persistent pleural leukocyte inflammatory response in comparison to all other groups. The pleural fluid levels of LDH, IL-8, and VEGF were greater for the higher doses of both agents in comparison to the lower doses. Of note, 0.1% silver nitrate led to significant higher pleural fluid LDH and IL-8 levels than those produced by talc 100 mg/kg at all time points and of VEGF at 6 h.
Only a few studies have addressed the systemic response to pleurodesis agents. An increase in the serum angiotensin-converting enzyme after intrapleural talc injection was reported in an experimental model in rabbits. (36) In a clinical study (37) comparing talc and tetracycline, talc induced greater hypoxemia and an acute increase in serum levels of C-reactive protein than did tetracycline.
The mechanisms by which talc induces a systemic inflammatory response remain unknown. Although it has been postulated that the systemic side effects associated with talc pleurodesis may be dose related, (26) there is not a great amount of evidence to support this affirmation. Since talc particles were found in other tissues in experimental studies (26) even with doses insufficient to produce a pleurodesis, there is strong evidence that this agent is potentially harmful regardless of the dose. (24-26) The migration of talc particles to the systemic circulation is hypothesized to be one of the likely mechanisms. Indeed, extra pleural talc in several organs has been demonstrated in experimental (24,25) and in clinical studies (38) after intrapleural administration. As the talc used for pleurodesis throughout the world has different sources and different sized particles, (39,40) it has been hypothesized that the small particles are more likely to gain access to the systemic circulation through the lymphatic route. (25,37) Other possible mechanisms have been advocated, including absorption of inflammatory mediators from the inflamed pleural space and the absorption of talc contaminants. (27) Another possible factor influencing the systemic effects of the pleurodesis agents is the condition of the pleural cavity. In benign pleural effusions or pneumothorax, the large surface of the normal mesothelial lining and the normal physiology of the pleural lymphatics may result in a higher rate of absorption of the agents instilled into the pleural space. However, with malignant involvement of the pleural cavity, there may be a lower rate of absorption and a subsequent lower risk of systemic effects.
Silver nitrate 0.5% has proved to be an efficient alternative to tetracycline derivatives and talc for inducing pleurodesis in experimental studies. (31,32) Its efficacy has also been proved in clinical studies. (30,41) In patients with malignant pleural effusions who received 0.5% silver nitrate or 5 g of talc "slurry," silver nitrate was more effective in inducing pleurodesis after a 1-month evaluation (95.6% vs 87.5%) and had no significant adverse systemic effects. (41)
Our findings indicate that the low dose of 0.1% silver nitrate produces an acute pleural inflammatory response that is more intense than that observed with talc 100 mg/kg or 400 mg/kg. In addition, 0.1% silver nitrate produces a less intense blood systemic inflammatory response in comparison to 0.5% silver nitrate and talc 100 mg/kg or 400 mg/kg.
Although 0.1% silver nitrate did not produce an effective pleurodesis in our rabbit model, (34) the observations of the present study may lead to new alternatives to produce pleurodesis. One possible approach is the repeated injection of low doses of silver nitrate, since the 0.1% dose produces an intense pleural inflammation with less systemic effects than the higher 0.5% dose. This approach could be particularly attractive in recurrent benign pleural effusions and pneumothorax, in which a long-term survival is predicted in contrast to malignancy.
In conclusion, talc in doses considered insufficient to induce a pleurodesis in our experimental model in rabbits produced adverse systemic effects comparable to those observed with the dose used to produce efficient pleurodesis. In contrast, 0.1% silver nitrate produced intense pleural inflammation with considerably fewer systemic effects than that observed with both doses of talc or 0.5% silver nitrate. In order to reduce the risk of the adverse systemic effects related to pleurodesis, intrapleural injection of repeated low doses of silver nitrate may be considered in future studies.
ACKNOWLEDGMENT: The authors thank Luis C. Moreira, Tania Cabral, Antonieta Lamanna, Geni Pedrosa, Luciana P. Almeida, Gabriela G. Carnevale, and Carlos S. R. Silva for their valuable collaboration.
REFERENCES
(1) Walker-Renard PB, Vaughan LM, Sahn SA. Chemical pleurodesis for malignant pleural effusions. Ann Intern Med 1994; 120:56-64
(2) Light RW. Pleural Diseases. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2001
(3) Marchi E, Teixeira LR, Vargas FS. Management of malignancy-associated pleural effusion: current and future treatment strategies. Am I Respir Med 2003; 2:261-273
(4) Marchi E, Teixeira LR, Vargas FS. Talc for pleurodesis: hero or villain [editorial]? Chest 2003; 124:416
(5) Agrenius V, Chmielewska J, Widstrom O, et al. Increased coagulation activity of the pleura after tube drainage and quinacrine instillation in malignant pleural effusion. Eur Respir J 1991; 4:1135-1139
(6) Koldsland S, Svennevig JL, Lehne G, et al. Chemical pleurodesis in malignant pleural effusions: a randomized prospective study of mepacrine versus bleomycin. Thorax 1993; 48:790-793
(7) Wallach HW. Intrapleural tetracycline for malignant pleural effusions. Chest 1975; 68:510-512
(8) Gravelyn TR, Michelson MK, Gross BH, et al. Tetracycline pleurodesis for malignant pleural effusions: a 10-year retrospective study. Cancer 1987; 59:1973-1977
(9) Landvater L, Hix WR, Mills M, et al. Malignant pleural effusion treated by tetracycline therapy. Chest 1988; 93: 1196-1198
(10) Light RW, O'Hara VS, Moritz TE, et al. Intrapleural tetracycline for the prevention of recurrent spontaneous pneumothorax: results of a Department of Veterans' Affairs cooperative study. JAMA 1990; 264:2224-2230
(11) Kitamura S, Sugiyama Y, Izumi T, et al. Intrapleural doxycycline for control of malignant pleural effusion. Curr Ther Res 1981; 30:515-521
(12) Muir JF, Deffouilloy C, Ndarurinze S, et al. The use of intrapleural doxycycline by lavage and drainage in recurrent malignant pleural effusions. Rev Mid Respir 1987; 4:29-33
(13) Mansson T. Treatment of malignant pleural effusion with doxycycline. Stand J Infect Dis 1988; 53:29-34
(14) Paladine W, Cunningham TJ, Sponzo R, et al. Intracavitary bleomycin in the management of malignant effusions. Cancer 1976; 38:1903-1908
(15) Bitran JD, Brown C, Desser RK, et al. Intracavitary bleomytin for the control of malignant effusions. J Surg Oncol 1981; 16:272-277
(16) Ostrowski MJ. An assessment of long-term results of controlling the reaccumulation of malignant effusions using intracavitary bleomycin. Cancer 1986; 57:721-727
(17) Ruckdeschel JC, Moores D, Lee JY, et al. Intrapleural therapy |or malignant pleural effusions: a randomized comparison of bleomycin and tetracycline. Chest 1991; 100:1528-1535
(18) Kessinger A, Wigton RS. Intracavitary bleomycin and tetracycline in the management of malignant pleural effusions: a randomized study. J Surg Oncol 1987; 36:81-83
(19) Vargas FS, Wang NS, Lee HM, et al. Effectiveness of bleomycin in comparison to tetracycline as pleural sclerosing agent in rabbits. Chest 1993; 104:1582-1584
(20) Hillerdal G, Kiviloog J, Nou E, et al. Corynebacterium parvum in malignant effusion: a randomized prospective study. Eur J Respir Dis 1986; 69:204-206
(21) Ross GA, Felletti R, Balbi B, et al. Symptomatic treatment of recurrent malignant pleural effusions with intrapleurally administered Corynebacterium parium: clinical response is not associated with evidence of enhancement of local cellular-mediated immunity. Am Rev Respir Dis 1987; 135:885-890
(22) de Campos JR, Vargas FS, Werebe EC, et al. Thoracoscopy tale poudrage: a 15-year experience. Chest 2001; 119:801-806
(23) Rehse DH, Aye RW, Florence MG. Respiratory failure after talc pleurodesis. Am J Surg 1999; 177:437-440
(24) Werebe EC, Pazetti R, Milanez de Campos JR, et al. Systemic distribution of talc after intrapleural administration in rats. Chest 1999; 115:190-193
(25) Ferrer J, Montes JF, Viillarino MA, et al. Influence of particle size on extrapleural talc dissemination after talc slurry pleurodesis. Chest 2002; 122:1018-1027
(26) Montes JF, Ferrer J, Villarino MA, et al. Influence of tale dose on extrapleural talc dissemination after talc pleurodesis. Am J Respir Crit Care Med 2003; 168::348-355
(27) Fraticelli A, Robaglia-Schlupp A, Riera H, et al. Distribution of calibrated talc after intrapleural administration: an experimental study in rats. Chest 2002; 122:1737-1741
(28) Brock RC. Recurrent and chronic spontaneous pneumothorax. Thorax 1948; 3:88-92
(29) Andersen I, Poulsen T. Surgical treatment of spontaneous pneumothorax. Acta Chir Stand 1959; 118:105-112
(30) Wied U, Halkier E, Hoeier-Madsen K, et al. Tetracycline versus silver nitrate pleurodesis in spontaneous pneumothorax. J Thorac Cardiovasc Surg 1983; 86:591-593
(31) Vargas FS, Teixeira LR, Silva LM, et al. Comparison of silver nitrate and tetracycline as pleural sclerosing agents in rabbits. Chest 1995; 108:1080-1083
(32) Vargas FS, Teixeira LR, Vaz MAC, et al. Silver nitrate is superior to talc slurry in producing pleurodesis in rabbits. Chest 2000; 118:808-813
(33) Vargas FS, Teixeira LR, Antonangelo L, et al. Experimental pleurodesis in rabbits induced by silver nitrate and talc: 1-year follow-up. Chest 2001; 119:1516-1520
(34) Teixeira LR, Vargas FS, Antonangelo L, et al. Low concentration silver nitrate pleurodesis in rabbits: optimal concentration for rapid and complete sclerosing effect. Lung 2003; 181:353-359
(35) Marchi E, Vargas FS, Acencio MP, et al. Talc and silver nitrate induce systemic inflammatory effects during the acute phase of experimental pleurodesis in rabbits. Chest 2004; 125:2268-2277
(36) Mitchem RE, Herndon BL, Fiorella RM, et al. Pleurodesis by autologous blood, doxycycline, and talc in a rabbit model. Ann Thorac Surg 1999; 67:917-921
(37) Maskell NA, Lee YC, Gleeson FV, et al. Randomized trials describing lung inflammation after pleurodesis with talc of varying particle size. Am J Respir Crit Care Med 2004; 170:377-382
(38) Campos JR, Werebe EC, Vargas FS, et al. Respiratory failure due to insufflated talc. Lancet 1997; 349:251-252
(39) Sanches C, Marchi E, Romero B, et al. Association of the size of talc particles with the occurrence of complications of pleurodesis [abstract]. Eur Respir J 2001; 18:5158-5168
(40) Ferrer J, Villarino MA, Tura JM, et al. Talc preparations used for pleurodesis vary markedly from one preparation to another. Chest 2001; 119:1901-1905
(41) Paschoalini MS, Pereira JR, Abdo EF, et al. Silver nitrate versus talc slurry for pleurodesis in patients with malignant pleural effusions [abstract]. Am J Respir Crit Care Med 1999; 159:A384
* From the Pleura Laboratory Pulmonary Division Heart Institute (InCor), University of Sao Paulo Medical School, Brazil; and Saint Thomas Hospital and Vanderbilt University, Nashville, TN. Supported by the Foundation to Support Research from the State of Sao Paulo (FAPESP 99/02777-3) and the National Board of Scientific and Technologic Development (CNPq) of Brazil.
Manuscript received November 13, 2004; revision accepted February 14, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Evaldo Marchi, MD, Pulmonary Division, Heart Institute (InCor), University of Sao Paulo Medical School, Brazil, Rua Lucia B. Passarin, 590, Ap.42, Jundiai, Sao Paulo, Brazil; e-mail: evmarchi@uol.com.br
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group