Cystic fibrosis (CF) is characterized by considerable oxidative stress. However, it is not known whether oxidative stress is an important feature early in this disease. We have investigated a group of infants and young children with CF to establish whether oxidants are produced in their airways. Bronchoalveolar lavage fluid (BALF) was assayed for myeloperoxidase as a measure of neutrophilic inflammation, and 3-chlorotyrosine as a biomarker of the potent oxidant hypochlorous acid, which is formed by myeloperoxidase. Protein carbonyls were also measured as a nonspecific indicator of reactive oxidant production. Myeloperoxidase and 3-chlorotyrosine levels in BALF from children with CF were 10- and fivefold higher, respectively, than in disease control subjects. There was a strong correlation between myeloperoxidase and 3-chlorotyrosine. Myeloperoxidase levels were fourfold higher in children with infections in their airways. Median protein carbonyls were elevated by only twofold compared with disease control subjects, but some children had extremely high levels of protein oxidation. We conclude that hypochlorous acid is produced early in CF and that it is a candidate for precipitating the fatal decline in lung function associated with this disease. Also, there must be other sources of oxidants because protein carbonyls were not related to either inflammation or infection.
Keywords: hypochlorous acid; neutrophil; oxidative stress; protein carbonyl
Cystic fibrosis (CF) is the most common fatal hereditary disease in populations of European ancestry (1). The disease is precipitated by defects in the CF transmembrane conductance regulator (CFTR) protein, which is an essential component of epithelial chloride transport in many organs. Death most often results from chronic progressive lung disease (1). Destruction of the airways is caused by repeated/continual bouts of infection and inflammation. A chronic neutrophilic inflammation of the airways is felt to be responsible for the majority of the tissue damage (2). Neutrophil-derived oxidants may contribute to tissue destruction in the airways (3, 4). These oxidants are generated when neutrophils ingest bacteria. Oxidants are derived from an NADPH-oxidase that reduces molecular oxygen to Superoxide. The Superoxide dismutates to hydrogen peroxide, which is used by the heme enzyme myeloperoxidase to oxidize chloride and thiocyanate to hypochlorous acid and hypthiocyanite, respectively (5). Pathways for oxidant production by neutrophils have been outlined in recent reviews (5, 6).
Hypochlorous acid is a potent cytotoxic agent and injures airway epithelial cells in vitro (7). Hypothiocyanite is much less toxic than hypochlorous acid (8). In support of the concept that neutrophil oxidants are involved in deteriorating lung function, levels of myeloperoxidase are elevated in sputum and bronochoalveolar fluid of patients with CF (9, H)). In addition, they are associated with the severity of lung disease as measured by lung function parameters and chest radiograph scores (9, 11).
Oxidative stress is a significant complication of CF (12, 13). It is manifested by elevated levels of lipid and protein oxidation products in both plasma (3, 4, 14) and airways secretions (15), as well as diminished antioxidanls (16). Although there is considerable evidence suggesting that oxidative stress exacerbates deterioration of the lungs in adults with CF, there is comparatively little information on how oxidants affect the airways in the initial stages of this disease. Early damage to the airways would be expected to compromise natural barriers to pathogens and encourage infection. Consequently, in this investigation we have focused on whether oxidants are produced in the airways of infants and young children with CF. We have measured biomarkers of oxidative stress in bronochoalveolar lavage fluid (BALF) from children less than 6 years old. In many cases the BALF obtained indicated the children were currently free of bacterial infection in their airways (17). Therefore, it was possible to assess the separate contributions that infection and inflammation made to oxidative stress.
METHODS
Study Population
Patients with CF. Twenty-three children with CF were studied (Table 1). All patients with CF were participating in research studies approved by the Human Subjects Review Committee, Denver, and informed consent was obtained from the patients' parents. For inclusion in these studies the patient had to have a stable clinical course with no respiratory exacerbations or changes in clinical care for the previous 30 days. Fifteen of the children with CF were identified by newborn screening based on serum-immunoreaclive trypsinogen determinations (18). One infant born in another state was the younger sibling of a previously identified patient with CF. All children had a sweat chloride concentration above 60 mmol/L. Only one of the children with CF had a chronic cough at the time of study. Standard clinical care for children with CF cared for at this center and diagnosed through newborn screening is to begin pancreatic enzyme treatment if they are symptomatic or if pancreatic insufficiency is found with an initial stool-fat collection. Seven CF children were receiving oral antibiotics for otitis media, upper respiratory tract infection, or chronic cough. None of the patients was receiving inhaled antibiotics.
Disease control subjects. Bronchoalvcolar lavage (BAL) was performed in seven disease control children for clinical indications such as suspected aspiration, chronic oxygen requirement, chronic cough, or stridor. None of the disease control children were acutely ill, none were on antibiotics, and none had chest radiographs indicating acute infection. The indications for flexible bronchoscopy in control children were defined independently by a different team of physicians who were performing clinical care.
BAL
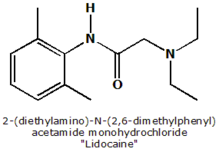
BAL was performed at the Children's Hospital in Denver. After peripheral intravenous access was established, children were sedated with midazolam 0.1-0.2 mg/kg and Fentanyl 1 to 3 µg/kg given intravenously. Children were closely monitored during and after the procedure for approximately 3 hours with continuous pulse oximetry. Viscous xylocaine was applied with cotton swabs to numb the nares. A 3.5-mm Pentax fiberoptic bronchoscope (Pentax Precision Instrument Corp., Orangeburg, NJ) was then passed through the nose to the posterior pharynx. The larynx was visualized and anesthetized with 0.1 ml/kg of 1% lidocaine. The bronochoscope was then passed into the trachea, and the carina was sprayed with an additional 0.1 to 0.2 ml/kg of the 1% lidocaine. The total airway dose of lidocaine did not exceed 5 mg/kg. The bronchoscope was advanced and wedged into the lingula or the right middle lobe bronchus, and three aliquots of 1 ml/kg of sterile normal saline were gently instilled. The fluid was aspirated by immediate gentle hand suction applied to the instilling syringe after each instillation. For each BAL, multiple aspirates were pooled into a single sample, which was used for subsequent analysis. All BAL fluid (BALF) samples were handled and processed in the same manner. Supernatants were obtained as quickly as possible and stored at -70°C for future analysis of oxidative markers (see below).
Analyses of BALF
Cytology. A 1-ml aliquot of BALF was used for total and differential cell counts. Differential counts on 100 cells were performed on Wright-Giemsa-stained cytoccntrifuge preparations made from the pooled BALF before centrifugation and resuspension. The preparations were counted in a blinded manner. The cytocentrifuge preparations were made using a Shandon Cytospin-2 (Shandon Southern Instruments, Sewickly, PA), and were ccntrifuged at 1,200 rpm for 5 minutes.
Bacterial and viral cultures. An aliquot of the pooled BALF was submitted for quantitative bacterial and viral cultures. Specific culture techniques were used to identify Staphylococcus aureus, Haempphilus influenza, and Pseudomonas aeruginosa, which are common CF-related pathogens (19). Viral cultures were performed to isolate common respiratory viruses (respiratory syncytial virus, influenza A and B, cytomegalovirus, parainfluenza 1, 2, and 3, adenovirus, and rhinovirus). Detection of fungal elements was done with the Calcofluor detection system (Polysciences, Inc., Warrington, PA).
BALF assays. The pooled BALF was centrifuged at 1,500 × g for 10 minutes. Viability of the BALF cells was determined by trypan blue dye exclusion and was always greater than 95%. The supernatant obtained was aliquoted and stored at -70°C until shipped in dry ice from Denver to Christchurch by airfreight. Samples arrived frozen and were immediately transferred to a -80°C freezer until assayed for myeloperoxidase, protein carbonyls, and chlorinated tyrosines. To determine whether shipping might promote oxidation of proteins, 17 BALF samples were split and either treated or not treated with 1 mM thiodipropionic acid to scavenge oxidizing species (20). No significant differences were found for protein carbonyls or chlorinated tyrosines between treated and untreated samples (data not shown). Thus, transport of samples did not affect the levels of oxidized proteins in the BALF.
NEUTROPHIL ELASTASE. Elastase complexed to α^sub 1^-antiprotease in BALF was determined through a commercially available heterogeneous enzyme immunoassay (Merk, Damstadt, Germany).
PEROXIDASE CONTENT. Peroxidases in BAL fluid were separated by diluting them 1:10 in a loading buffer of 100 mM phosphate pH 6.0 containing 0.03% cetrimide. CM-Sepharose CL 6B (50 mg; Pharmacia, Uppsala, Sweden) was then added to a final volume of 1 ml. The solution was mixed for 30 minutes to allow the positively charged peroxidases to bind to the cation exchanger. Subsequently, the gel was pelleted, supernatant removed, and washed once with the loading buffer containing 50 mM sodium sulfate. Myeloperoxidase was eluted using loading buffer containing 200 mM sodium sulfate and then washed twice with the same buffer. Finally the gel was washed with loading buffer containing 600 mM sodium sulfate to elute any eosinophil peroxidase. The activity of the peroxidases was measured in 200 mM sodium acetate buffer pH 5.4 containing 1.4 mM 3,3,'5,5'-tetramethylbenzidine as the reducing substrate, 200 µM hydrogen peroxide, 0.3% cetrimide, and 10% dimethylformamide (21). The change in absorbance at 630 nm was recorded after 30 minutes. Activity of myeloperoxidase was compared with that of a known amount of the purifed enzyme and expressed as micrograms of enzyme per milligram of total protein (22). Total myeloperoxidase protein was measured with commercially available radioimmunoassay kit in accordance with the manufacturer's instructions (Pharmacia). The activity assay for myeloperoxidase was calibrated against the radioimmunoassay so that results obtained in both assays could be directly compared.
CHLORINATED TYROSINES. Tyrosine (Tyr), 3-chlorotyrosine (Cl-Tyr), and 3,5-dichlorotyrosine (diCl-Tyr) in proteins from BALF were determined using stable isotope dilution gas chromatography with mass spectrometry (23, 24). Samples containing 40 µg of protein were desalted by gel filtration using Micro Bio-spin P6 chromatography columns (Biorad, Hercules, CA). [^sup 13^C]-Labeled internal standards were then added to the samples, which were dried under vacuum, and subsequently hydrolyzed for 18 hours at 110°C using methane sulfonic acid (4 N) containing 1% (vol/vol) phenol (100 µl). The hydrolysate was diluted in 0.1% trifluoroacetic acid (500 µl) and tyrosine derivatives were isolated using solid phase extraction (C18). They were eluted with 80% methanol containing 0.1% trifluoroacetic acid (1.1 ml) and dried under vacuum. Amino acids were derivatized with 3.5 M hydrobromic acid in propanol (300 µl) for 2 hours at 65°C and then with trifluoroacetic anhydride/ ethyl acetate (1:4, vol/vol) (100 µl) for 1 hour at 65°C. The derivatized samples were finally diluted in ethyl acetate and analyzed using a Hewlett Packard 6890 gas chromatograph equipped with a 30-m ZB-50 capillary column that was interfaced to a Hewlett Packard 5973 mass spectrometer (Palo Alto, CA). The initial column temperature of 65°C was maintained for 2 minutes and then increased to 150°C (30°C/min), 170°C (4°C/min), 200°C (5°C/min), and to 260°C (30°C/min). The injector, auxiliary channel, and ion source temperatures were set to 250, 280, and 150°C, respectively. Pulsed splitless injection was used with selective-ion monitoring. To check for artifactual halogenation of proteins, each batch of samples subjected to hydrolysis contained an additional sample of albumin. If Cl-Tyr levels in the albumin exceeded 50 µmol/mol of Tyr, the entire batch was rejected. The normal range of Cl-Tyr in albumin was 20 to 50 µmol/mol of tyrosine.
PROTEIN OXIDATION. Protein carbonyls were determined using a kit from Zenith Technologies (Dunedin, New Zealand). Proteins in supernatants were reacted with 2,4-dinitrophenylhydrazine, then absorbed onto wells in an ELISA plate and probed with an antibody raised against protein conjugated 2,4-dinitrophenylhydrazine. The biotin-conjugated primary antibody was then reacted with streptavidin-biotinylated horse-radish peroxidase for quantification (25). Total protein in supernatants was measured using the BioRad protein assay reagent.
Statistical Analysis
When comparing data between controls and children with CF, repeated measurements on the same individual were averaged. When investigating correlations between different markers, all values obtained for each subject were used. Data were expressed as the median with the interquartile range. The Mann Whitney U-test was used to examine differences between children with CF and disease control subjects. Spearman's correlation coefficient was used to examine relationships between the variables. A relationship was identified if r was greater than 0.4. A p value of less than 0.05 was considered significant. All statistical tests were performed using SigmaStat (Jandel Corp., San Rafael, CA).
RESULTS
Characteristics of Subjects
The characteristics of the two study populations are shown in Table 1. As outlined in Table 1, there were 7 control children in the study and 23 children with CF. Each of the control children had one BAL. Nine of the children with CF had more than one BAL before the age of 6. One subject had five bronchoscopies, two had three each, and six had two bronchoscopies. All of these bronchoscopies were performed as described in METHODS as part of studies looking at airway inflammation and therapy in children with CF, and all were done when the patient was clinically stable without any change in therapy for 30 days. The disease control subjects had fewer white blood cells in their BALF than children with CF, although this did not reach significance. Neutrophil numbers and percentages were significantly higher in the patients with CF.
Myeloperoxidase Is Elevated in BALF from Young Children with CF
Total peroxidase activity was elevated more than 10-fold in BALF from children with CF compared with control subjects (medians 3.6 versus 0.3 µg/mg protein; p = 0.002) (Figure 1A). To confirm that myeloperoxidase was responsible for total peroxidase activity, we also measured its concentration by an immunologic method. In BALF from the patients with CF, there was an excellent correlation between total peroxidase activity and myeloperoxidase protein (Figure 1B). From the slope of the plot in Figure 1B it is apparent that about 85% of the enzyme was active. To further confirm that the peroxidase activity was solely due to myeloperoxidase, we extracted peroxidases from BALF using cation-exchange chromatography. Under the conditions of our assay lactoperoxidase does not bind to the CM-Sepharose, whereas myeloperoxidase and eosinophil peroxidase bind and are eluted with 200 mM and 600 mM sodium sulfate, respectively (26). In all the samples, appreciable peroxidase activity was detected only in the salt wash that eluted purified myeloperoxidase (Figure 1C). Thus, we conclude that myeloperoxidase was markedly elevated in BALF from children with CF and that there was no detectable lactoperoxidase or eosinophil peroxidase. Using the urea method (27), we calculated that the median concentration of myeloperoxidase in epithelial lining fluid was 184 nM and ranged from
Myeloperoxidase activity was significantly correlated with the percentage of neutrophils (r = 0.53, p = 0.008, n = 24) and elastase complexed to α^sub 1^-antiprotease in BALF (r = 0.85, p
Chlorinated Tyrosines and Protein Carbonyls Are Elevated in BALF from Young Children with CF
3-Chlorotyrosine and 3,5-dichlorotyrosine are formed when hypochlorous acid reacts with proteins containing tyrosine residues. They are specific biomarkers for this neutrophil oxidant (28, 29). 3-Chlorotyrosine was markedly elevated in BALF from children with CF compared with control subjects (medians 222.5 versus 49.0 µmol/mol tyrosine; p = 0.003, n = 18 and 7) (Figure 2A). Although levels of 3,5 dichlorotyrosine were high in some samples, the difference between children with CF and control subjects did not reach statistical significance (medians 65 versus 47.9 µmol/mol tyrosine; p = 0.631, n = 18 and 7) (Figure 2B).
BALF from children with CF contained significantly greater levels of protein carbonyls than that from control subjects (medians 0.98 versus 0.40 nmol/mg protein; p
Relationships between Inflammation and Biomarkers of Oxidative Damage
There was a significant association between myeloperoxidase activity and either 3-chlorotyrosine (r = 0.87, p
Relationships between Age at Time of Sampling and Indices of Oxidative Damage
It was of interest to determine how early the lungs of children with CF were subjected to oxidative stress and whether oxidative stress increased with age. Levels of myeloperoxidase (n = 34), 3-chlorotyrosine (n = 18), or protein carbonyls (n = 25) were not associated with age at the time BALF was sampled. For some of the children these biomarkers were high at 2 to 3 months of age (data not shown). There was no sex difference for any of the oxidative biomarkers (data not shown).
Relationships between Infectious Status to Indices of Oxidative Damage
To further probe the connection between inflammation and oxidative stress in CF, we determined whether the biomarkers were influenced by infection of the airways. Samples of BALF were cultured for various organisms that colonize the lower respiratory tract in children with CF. These organisms included S. aureus, H. influenzae, P. aeruginosa, respiratory syncytial virus, influenza A and B, cytomegalovirus, parainfluenza 1, 2, and 3, adenovirus, enterovirus, and fungi. Cultures with any growth (corresponding to a lower limit of detection of bacteria of
BALF with positive cultures had significantly elevated concentrations of myeloperoxidase compared with BALF with negative cultures (medians 7.5 versus 1.7 µg/mg protein; p
DISCUSSION
In this investigation we studied a group of infants and young children with CF to ascertain the extent to which their airways were subjected to oxidative stress. There have been numerous other studies into how reactive oxidants may contribute to the pathology of CF (12, 13). However, our work is unique in that we investigated protein damage within the airways of young children. We have demonstrated that oxidative stress occurs in the airways of young children with CF. It was evident in some infants as young as 2 months old. Children with CF had elevated levels of myeloperoxidase in their BALF. The enzyme had been actively producing hypochlorous acid because substantial quantities of the specific biomarker 3-chlorotyrosine were present in airway proteins. Oxidative stress was also characterized by high levels of protein carbonyls in BALF. Thus, reactive oxidants are indeed potential candidates for initiating the progressive loss in the lung function that is characteristic of CF. Due to the limited number of subjects with repeat bronchoscopies in this study, we can only speculate whether this oxidant damage is chronically progressive or represents multiple separate events.
There has been much debate in the literature as to whether inflammation in the lungs of children with CF is a consequence of infection or whether infection follows inflammatory tissue damage (17, 32-34). In the children we studied there was a demonstrable inflammatory response to infection as judged by increases in myeloperoxidase and protein chlorination. However, in some children these markers of inflammation were high even when active infections were undetectable. This may indicate that inflammation can exist in the absence of infection. Alternatively, it could be the result of prior infection or could represent an active infection that was below the limit of detection (35, 36).
We found corroborative evidence that neutrophils are stimulated to degranulate and produce reactive oxidants in the airways of children with CF. We measured substantial levels of myeloperoxidase in BALF, which was predominantly active. The good correlations of myeloperoxidase with percent neutrophils and complexed elastase testify to the fact that the peroxidase activity originated from neutrophils when they had degranulated. Also, the strong association between myeloperoxidase and 3-chlorotyrosine suggest that the neutrophils had undergone a respiratory burst to produce superoxide and hydrogen peroxide, which were ultimately converted to hypochlorous acid. The concentrations of myeloperoxidase we measured in BALF translate to concentrations of the enzyme in epithelial lining fluid of up to 2 µM. At these concentrations, myeloperoxidase would be expected to scavenge all the hydrogen peroxide formed in its vicinity, and produce hypochlorous acid as well as other oxidants such as hypothiocyanite, nitrogen dioxide, and tyrosyl radical (5).
The relative amounts of the different oxidants formed by myeloperoxidase in the airways will depend on the concentrations of each of its substrates. Recently it was found that the concentration of thiocyanate in undiluted airway secretions is as high as 0.5 mM (37), which is the K^sub m^ for myeloperoxidase. At this concentration with 100 mM chloride, myeloperoxidase would use approximately 80% of the hydrogen peroxide its encounters to produce hypothiocyanite and 20% to produce hypochlorous acid (38). Nitrogen dioxide, tyrosyl radical, and hypobromous acid would be expected to be minor products. Thus, in normal airways the weak oxidant hypothiocyanite should be the major product of myeloperoxidase, not hypochlorous acid. This state may not hold in CF. The CFTR is an anion channel that is capable of transporting thiocyanate as well as chloride and other halides (39). Bromide has significantly decreased reabsorption in individuals with CF (40). Thiocyanate is likely to behave similarly. A disproportionate decrease in thiocyanate concentration relative to chloride would result in abnormally high production of hypochlorous acid. Thus, it is plausible that in CF there could be a major shift in the product profile of myeloperoxidase from a weak to a strong oxidant. This would compound the oxidative stress associated with inflammation in the lungs of patients with CF. Exactly how thiocyanate impacts on the activity of myeloperoxidase in CF needs further investigation.
The levels of 3-chlorotyrosine we measured in BALF from children with CF were substantially higher than in the disease control subjects. They were also high compared with those measured in lavage fluid from very low birth weight children (41) and comparable to those values reported in sputum from patients with asthma (23, 26), and in atherosclerosis lesions (42, 43). However, levels of 3-chlorotyrosine were 20-fold lower than reported in sputum from adults with CF (15). This difference may simply reflect the greater degree of infection in older patients. However, the high levels of 3-chlorotyrosine that were measured in control sputa suggest that chlorinated proteins may accumulate in sputum or that myeloperoxidase trapped in sputum may continue to chlorinate associated proteins.
Based on work with sputum, Worlitzsch and coworkers argued that catalase released by neutrophils will scavenge hydrogen peroxide and prevent myeloperoxidase from converting it to hypochlorous acid (44). Furthermore, they proposed that myeloperoxidase is immobilized in the sputum matrix and thereby unable to exert its toxic effects. However, these workers conceded that catalase may not be present in very young children with CF who have minimal or no sputum. Indeed, the presence of 3-chlorotyrosine in BALF clearly demonstrated that insufficient catalase was present in the airways to stop myeloperoxidase from producing hypochlorous acid.
In CF the α^sub 1^-proteinase defense mechanism in the airways may be overwhelmed by release of elastase from neutrophils (17). This effect would be exacerbated if hypochlorous acid inactivates α^sub 1^-proteinase inhibitor by oxidizing its critical methionine residue. Our data suggest that this is a distinct possibility. Methionine is converted to methionine sulfoxide in proteins at much lower concentrations of hypochlorous acid than are required to form 3-chlorotyrosine (45, 46). Also, the high levels of 3-chlorotyrosine and protein carbonyls present in proteins from the airways of children with CF were similar to those achieved when a milligram of purified albumin was treated with approximately 100 nmol of hypochlorous acid (24). This equates to 20 times the amount of hypochlorous acid required to inactivate α^sub 1^-proteinase inhibitor (47).
Very high levels of carbonyls were present in proteins in BALF from children with CF. They were markedly elevated compared with the disease control subjects and higher than previous levels we have measured in lavage fluid from premature infants (31), and in sputum from adults with asthma (26). This comparative data indicates that the children's lungs were subjected to substantial oxidative stress. The levels of protein carbonyls were not related to neutrophilic inflammation or infection. In contrast, in individuals with asthma, protein carbonyls were strongly related to the content of myeloperoxidase and eosinophil peroxidase in sputum, as well as halogenated tyrosines (26). It is conceivable that in our patients with CF, the airway proteins were oxidized by other oxidants besides those produced by myeloperoxidase.
Peroxynitrite is a potential candidate for promoting formation of protein carbonyls in CF. It is formed from the reaction of nitric oxide with superoxide (48), and produces carbonyls on proteins (49). Nitric oxide levels in exhaled breath are low in patients with CF (50, 51) partly due to decreased expression of inducible nitric oxide synthase (52). But the elevated levels of nitrate/nitrite and 3-nitrotyrosine in sputum (53, 54) and exhaled breath (55) indicate that metabolism of nitric oxide is enhanced in CF. The presence of 3-nitrotyrosine in sputum suggests that peroxynitrite is produced in CF (54). However, 3-nitrotyrosine is also formed through myeloperoxidase-dependent oxidation of nitrite (56). Thus, it has yet to be established unequivocally that peroxynitrite is formed in the lungs of patients with CF.
There is potential for other peroxidases to participate in oxidation of airway proteins. These enzymes include eosinophil peroxidase, which is the major protein of eosinophils (57), and lactoperoxidase, which has been shown to be present in normal human airway secretions (37, 58). Eosinophil peroxidase is unlikely to have contributed to protein oxidation in the children we studied because eosinophils were rarely present in their BALF, nor could we detect any activity from this enzyme. However, eosinophilic activation has been detected in sputum from adult patients (59, 60). We also did not detect lactoperoxidase activity in any of the BALF samples from the children with CF. This may have resulted because lactoperoxidase was not present in the part of the lung we sampled. However, it is also possible that the enzyme was inactivated by its own products (61), and consequently not detected by our assay. Given the high degree of oxidative stress in the airways of young children with CF, and the potential of lactoperoxidase to participate in radical production, its activity in this disease warrants close scrutiny.
Another explanation for the high levels of protein carbonyls that were measured in this study is that antioxidant defenses are impaired in CF. Thus, normal levels of oxidant production may lead to abnormal degrees of oxidative damage. Indeed, patients with CF have decreased amounts of antioxidants in plasma due their associated malabsorption problems (62). An even more intriguing scenario is that a defective CFTR impedes glutathione efflux (63), which results in markedly decreased glutathione concentrations in epithelial lining fluid (64). Glutathione is involved in several redox processes that protect against oxidative stress (65) and it could act as an endogenous antioxidant in the airways (63). However, it was recently found that glutathione treatment of the lower airways did not affect markers of oxidative injury (66).
In conclusion, we have shown that there is considerable oxidative stress in the airways of young children with CF. Hypochlorous acid is one of the oxidants formed but others must also be produced. Identification of these oxidants and their sources should lead to novel strategies for preventing deterioration of lung function. Caution must be advised when considering therapies aimed at quenching neutrophil oxidant production. These therapies could interfere with oxidative killing mechanisms of neutrophils and further complicate infections in patients with CF. It is noteworthy though that myeloperoxidase deficiency generally does not predispose individuals to infection (6). Consequently, targeting this enzyme may have the advantage of preventing production of a toxic oxidant without compromising host defense.
References
1. Ratjen F, Doring G. Cystic fibrosis. Lancet 2003;361:681-689.
2. De Rose V. Mechanisms and markers of airway inflammation in cystic fibrosis. Eur Respir J 2002;19:333-340.
3. Brown RK, Kelly FJ. Evidence for increased oxidative damage in patients with cystic fibrosis. Pediatr Res 1994;36:487-493.
4. Brown RK, Wyatt H, Price JF, Kelly FJ. Pulmonary dysfunction in cystic fibrosis is associated with oxidative stress. Eur Respir J 1996;9:334-339.
5. Kettle AJ, Winterbourn CC. Myeloperoxidase: a key regulator of neutrophil oxidant production. Redox Rep 1997;3:3-15.
6. Klebanoff SJ. Oxygen Metabolites from Phagocytes. In: Gallin JI, Snyderman R, editors. Inflammation: basic principles and clinical correlates. Philadelphia: Lippincott Williams & Wilkins; 1999, pp. 721-768.
7. Regelmann WE, Schneider LA, Fahrenkrug SC, Gray BH, Johnson S, Herron JM, Clawson CC, Clawson DJ, Wangensteen OD. Proteinase-free myeloperoxidase increases airway epithelial permeability in a whole trachea model. Pediatr Pulmonol 1997;24:29-34.
8. Slungaard A, Mahoney JR. Thiocyanate is the major substrate for eosinophil peroxidase in physiologic fluids. J Biol Chem 1991;266:4903-4910.
9. Meyer KC, Zimmerman J. Neutrophil mediators, Pseudomonas, and pulmonary dysfunction in cystic fibrosis. J Lab Clin Med 1993;121:654-661.
10. Mohammed JR, Mohammed BS, Pawluk LJ, Bucci DM, Baker NR, Davis WB. Purification and cytotoxic potential of myeloperoxidase in cystic fibrosis sputum. J Lab Clin Med 1988;112:711-720.
11. Regelmann WE, Siefferman CM, Herron JM, Elliot GR, Clawson CC, Gray BH. Sputum peroxidase activity correlates with the severity of lung disease in cystic fibrosis. Pediatr Pulmonol 1995;19:1-9.
12. Brown RK, Kelly FJ. Role of free radicals in the pathogenesis of cystic fibrosis. Thorax 1994;49:738-742.
13. van der Vliet A, Eiserich JP, Marelich GP, Halliwell B, Cross CE. Oxidative stress in cystic fibrosis: does it occur and does it matter? Adv Pharmacol 1997;38:491-513.
14. Dominguez C, Gartner S, Linan S, Cobos N, Moreno A. Enhanced oxidative damage in cystic fibrosis patients. Biofactors 1998;8:149-153.
15. van der Vliet A, Nguyen MN, Shigenaga MK, Eiserich JP, Marelich GP, Cross CE. Myeloperoxidase and protein oxidation in cystic fibrosis. Am J Physiol 2000;279:L537-L546.
16. Portal BC, Richard M, Faure HS, Hadjian A, Favier AE. Altered antioxidant status and increased lipid peroxidation in children with cystic fibrosis. Am J Clin Nutr 1995;61:843-847.
17. Kahn TZ, Wagener JS, Bost T, Martinez J, Accurso FJ, Riches DWH. Early pulmonary inflammation in infants with cystic fibrosis. Am J Respir Crit Care Med 1995;151:1075-1082.
18. Hammond KB, Abman SH, Sokol RJ, Accurso FJ. Efficacy of statewide neonatal screening for cystic fibrosis by assay of trypsinogen concentrations. N Engl J Med 1991;325:769-774.
19. Hoiby N. Hemophilus influenzae, Staphylococcus aureus, Pseudomonas cepacia, and Pseudomonas aeruginosa in patients with cystic fibrosis. Chest 1988;94:97S-103S.
20. Thomas EL, Grisham MB, Jefferson MM. Cytotoxicity of chloramines. Methods Enzymol 1986;132:585-593.
21. Bozeman PM, Learn DB, Thomas EL. Assay of the human leukocyte enzymes myeloperoxidase and eosinophil peroxidase. J Immunol Methods 1990;126:125-133.
22. Kettle AJ, Winterbourn CC. Superoxide modulates the activity of myeloperoxidase and optimizes the production of hypochlorous acid. Biochem J 1988;252:529-536.
23. Wu W, Samoszuk MK, Comhair SAA, Thomassen MJ, Farver CF, Dweik RA, Kavuru MS, Erzurum SC, Hazen SL. Eosinophils generate brominating oxidants in allergen-induced asthma. J Clin Invest 2000;105: 1455-1463.
24. Chapman ALP, Senthilmohan R, Winterbourn CC, Kettle AJ. Comparison of mono and dichlorinated tyrosines with carbonyls for detection of hypochlorous acid-modified proteins. Arch Biochem Biophys 2000; 377:95-100.
25. Buss IH, Chan TP, Sluis KB, Domigan NM, Winterbourn CC. Protein carbonyl measurement by a sensitive ELISA method. Free Radic Biol Med 1997;23:361-366.
26. Aldridge RE, Chan TP, Van Dalen CJ, Senthilmohan R, Town GI, Winn MC, Venge P, Kettle AJ. Eosinophil peroxidase produces hypobromous acid in the airways of stable asthmatics. Free Radic Biol Med 2002;33:847-856.
27. Rennard SI, Basset G, Lecossier D, O'Donnell KM, Pinkston P, Martin PG, Crystal RG. Estimation of volume of epithelial lining fluid recovered by lavage using urea as marker of dilution. J Appl Physiol 1986; 60:532-538.
28. Domigan NM, Charlton TS, Duncan MW, Winterbourn CC, Kettle AJ. Chlorination of tyrosyl residues in peptides by myeloperoxidase and human neutrophils. J Biol Chem 1995;270:16542-16548.
29. Fu S, Wang H, Davies M, Dean R. Reactions of hypochlorous acid with tyrosine and peptidyl-tyrosyl residues give dichlorinated and aldehydic products in addition to 3-chlorotyrosine. J Biol Chem 2000;275:10851-10858.
30. Winterbourn CC, Chan TP, Buss IH, Inder TE, Mogridge N, Darlow BA. Protein carbonyls and lipid peroxidation products as oxidation markers in preterm infant plasma: associations with chronic lung disease and retinopathy and effect of selenium supplementation. Pediatr Res 2000;48:84-90.
31. Buss IH, Darlow BA, Winterbourn CC. Elevated protein carbonyls, lipid peroxidation products and myeloperoxidase in tracheal aspirates from premature infants. Pediatr Res 2000;47:640-645.
32. Cantin A. Cystic fibrosis lung inflammation: early, sustained, and severe. Am J Respir Crit Care Med 1995;151:939-941.
33. Hoiby N. Inflammation and infection in cystic fibrosis-hen or egg? Eur Respir J 2001;17:4-5.
34. Rosenfeld M, Gibson RL, McNamara S, Emerson J, Burns JL, Castile R, Hiatt P, McCoy K, Wilson CB, Inglis A, et al. Early pulmonary infection, inflammation, and clinical outcomes in infants with cystic fibrosis. Pediatr Pulmonol 2001;32:356-366.
35. Berger M. Lung inflammation early in cystic fibrosis: bugs are indicted, but the defense is guilty. Am J Respir Crit Care Med 2002; 165:857-858.
36. Griese M, Ramakers J, Krasselt A, Starosta V, Van Koningsbruggen S, Fischer R, Ratjen F, Mullinger B, Huber RM, Maier K, et al. Improvement of alveolar glutathione and lung function but not oxidative state in cystic fibrosis. Am J Respir Crit Care Med 2004;169:822-828.
37. Wijkstrom-Frei C, El-Chemaly S, Ali-Rachedi R, Gerson C, Cobas MA, Forteza R, Salathe M, Conner GE. Lactoperoxidase and human airway host defense. Am J Respir Cell Mol Biol 2003;29:206-212.
38. Van Dalen CJ, Whitehouse MW, Winterbourn CC, Kettle AJ. Thiocyanate and chloride as competing substrates for myeloperoxidase. Biochem J 1997;327:487-492.
39. Linsdell P. Relationship between anion binding and anion permeability revealed by mutagenesis within the cystic fibrosis transmembrane conductance regulator chloride channel pore. J Physiol 2001;531:51-66.
40. Miller ME, Cosgriff JM, Schwartz RH. Sweat bromide excretion in cystic fibrosis. J Lab Clin Med 1986;108:406-410.
41. Buss IH, Senthilmohan R, Darlow BA, Mogridge N, Kettle AJ, Winterbourn CC. 3-Chlorotyrosine as a marker of protein damage by myeloperoxidase in tracheal aspirates from preterm infants: association with adverse respiratory outcome. Pediatr Res 2003;53:455-462.
42. Hazen SL, Heinecke JW. 3-Chlorotyrosine, a specific marker of myeloperoxidase-catalyzed oxidation, is markedly elevated in low density lipoprotein isolated from human atherosclerotic intima. J Clin Invest 1997;99:2075-2081.
43. Upston JM, Niu X, Brown AJ, Mashima R, Wang H, Senthilmohan R, Kettle AJ, Dean RT, Stocker R. Disease stage-dependent accumulation of lipid and protein oxidation products in human atherosclerosis. Am J Pathol 2002;160:701-710.
44. Worlitzsch D, Herberth G, Ulrich M, Döring G. Catalase, myeloperoxidase and hydrogen peroxide in cystic fibrosis. Eur Respir J 1998;11:377-383.
45. Pattison DI, Davies MJ. Absolute rate constants for the reaction of hypochlorous acid with protein side chains and peptide bonds. Chem Res Toxicol 2001;14:1453-1464.
46. Chapman AL, Winterbourn CC, Brennan SO, Jordan TW, Kettle AJ. Characterisation of non-covalent oligomers of proteins treated with hypochlorous acid. Biochem J 2003;375:33-40.
47. Matheson NR, Travis J. Differential effects of oxidizing agents on human plasma α^sub 1^-proteinase inhibitor and human neutrophil myeloperoxidase. Biochemistry 1985;24:1941-1945.
48. Stamler JS, Singel DJ, Loscalzo J. Biochemistry of nitric oxide and its redox-active forms. Science 1992;258:1898-1902.
49. Ischiropoulos H, al-Mehdi AB. Peroxynitrite-mediated oxidative protein modifications. FEBS Lett 1995;364:279-282.
50. Jobsis Q, Raatgeep HC, Schellekens SL, Kroesbergen A, Hop WC, de Jongste JC. Hydrogen peroxide and nitric oxide in exhaled air of children with cystic fibrosis during antibiotic treatment. Eur Respir J 2000;16:95-100.
51. Ho LP, Innes JA, Greening AP. Exhaled nitric oxide is not elevated in the inflammatory airways diseases of cystic fibrosis and bronchiectasis. Eur Respir J 1998;12:1290-1294.
52. Meng QH, Springall DR, Bishop AE, Morgan K, Evans TJ, Habib S, Gruenert DC, Gyi KM, Hodson ME, Yacoub MH, et al. Lack of inducible nitric oxide synthase in bronchial epithelium: a possible mechanism of susceptibility to infection in cystic fibrosis. J Pathol 1998; 184:323-331.
53. Linnane SJ, Keatings VM, Costello CM, Moynihan JB, O'Conner CM, Fitzgerald MX, McLoughlin P. Total sputum nitrate plus nitrite is raised during acute pulmonary infection in cystic fibrosis. Am J Respir Crit Care Med 1998;158:207-212.
54. Jones KL, Hegab AH, Hillman BC, Simpson KL, Jinkins PA, Grisham MB, Owens MW, Sato E, Robbins RA. Elevation of nitrotyrosine and nitrate concentrations in cystic fibrosis sputum. Pediatr Pulmonol 2000;30:79-85.
55. Ho LP, Innes JA, Greening AP. Nitrite levels in breath condensate of patients with cystic fibrosis is elevated in contrast to exhaled nitric oxide. Thorax 1998;53:680-684.
56. Eiserich JP, Hristova M, Cross CE, Jones AD, Freeman BA, Halliwell B, van der Vliet A. Formation of nitric oxide-derived inflammatory oxidants by myeloperoxidase in neutrophils. Nature 1998;391:393-397.
57. Henderson WR. Eosinophil Peroxidase: Occurence and biological function. In: Everse J, Grisham MB, editors. Peroxidases, Chemistry and Biology. Boston: CRC Press; 1990, p. 105-121.
58. El-Chemaly S, Salathe M, Baier S, Conner GE, Forteza R. Hydrogen peroxide-scavenging properties of normal human airway secretions. Am J Respir Crit Care Med 2003;167:425-430.
59. Koller DY, Urbanek R, Gotz M. Increased degranulation of eosinophil and neutrophil granulocytes in cystic fibrosis. Am J Respir Crit Care Med 1995;152:629-633.
60. Koller DY, Gotz M, Eichler I, Urbanek R. Eosinophilic activation in cystic fibrosis. Thorax 1994;49:496-499.
61. Jenzer H, Kohler H, Broger C. Role of hydroxyl radicals in irreversible inactivation of lactoperoxidase by excess H^sub 2^O^sub 2^. Arch Biochem Biophys 1987;258:381-390.
62. Winklhofer-Roob BM. Oxygen free radicals and antioxidants in cystic fibrosis: the concept of an oxidant-antioxidant imbalance. Acta Paediatr 1994;Suppl. 395:49-57.
63. Linsdell P, Hanrahan JW. Glutathione permeability of CFTR. Am J Physiol 1998;275:C323-C326.
64. Gao L, Kim KJ, Yankaskas JR, Forman HJ. Abnormal glutathione transport in cystic fibrosis airway epithelia. Am J Physiol 1999;277:L113-L118.
65. Rahman I, MacNee W. Oxidative stress and regulation of glutathione in lung inflammation. Eur Respir J 2000;16:534-554.
66. Dakin CJ, Numa AH, Wang H, Morton JR, Vertzyas CC, Henry RL. Inflammation, infection, and pulmonary function in infants and young children with cystic fibrosis. Am J Respir Crit Care Med 2002;165:904-910.
Anthony J. Kettle, Timothy Chan, Iris Osberg, Revathy Senthilmohan, Anna L. P. Chapman, Tessa J. Mocatta, and Jeffrey S. Wagener
Free Radical Research Group, Department of Pathology, Christchurch School of Medicine and Health Sciences, Christchurch, New Zealand; and Department of Pediatrics, University of Colorado Health Science Center and Children's Hospital, Denver, Colorado
(Received in original form November 6, 2003; accepted in final form September 27, 2004)
Supported by the Health Research Council of New Zealand, the Asthma and Respiratory Foundation of New Zealand, the Cystic Fibrosis Foundation (USA), and grant number MO1-RR00069 of the General Clinical Research Centers Program, National Institutes of Health (USA).
Correspondence and requests for reprints should be addressed to Dr. Tony Kettle, Ph.D., Free Radical Research Group, Department of Pathology, Christchurch School of Medicine and Health Sciences, P.O. Box 4345, Christchurch, New Zealand. E-mail: tony.kettle@chmeds.ac.nz
Am J Respir CHt Care Med Vol 170. pp 1317-1323, 2004
Originally Published in Press as DOI: 10.1164/rccm.200311-1516OC on October 1, 2004
Internet address: www.atsjournals.org
Conflict of Interest Statement: A.J.K. received $180,000 between 2001 and 2003 from AstraZeneca for a collaborated research project; T.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; I.O. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; R.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; A.L.P.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; T.J.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; J.S.W. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
Acknowledgment: The authors appreciate the helpful advice on analytical techniques given to us by Professor Christine Winterbourn.
Copyright American Thoracic Society Dec 15, 2004
Provided by ProQuest Information and Learning Company. All rights Reserved