The standard of care for the treatment of HIV type 1 infection includes a combination of highly active antiretroviral drugs (HAART) with the goal of suppressing plasma HIV RNA (viral load) to undetectable levels.1 Currently, 14 drugs are available to treat HIV-1 (see Table 1). The ongoing approval of new drugs has expanded patient-care options but has also contributed to the increased complexity of treatment. Clinicians must consider the pharmacokinetics, drug interactions, and resistance patterns of these drugs, as well as potential patient adherence issues.
Abacavir and efavirenz are two recently approved antiretroviral drugs. This article provides general information on the use of these two drugs and their role in the treatment of HIV-1.
Abacavir (Ziagen)
Mechanism of Action
Abacavir (ABC) is a member of the nucleoside reverse transcriptase inhibitor family (NRTI), sometimes referred to as nucleoside analogues. Unlike other NRTIs, which are thymidine or purine analogues, ABC is a guanosine analogue.2 ABC is converted by intracellular enzymes to carbovir triphosphate, which is a potent inhibitor of HIV-1 reverse transcriptase. Carbovir triphosphate competes with deoxyguanosine 5'-triphosphate and becomes incorporated into the growing viral DNA. The absence of the 3'-OH group results in chain termination and interruption of viral replication.2-4
Pharmacokinetics
ABC is rapidly and extensively absorbed after oral administration. In an open-label, single-dose study, the mean absolute bioavailability of 300-mg tablets was 83%.4,5 Studies evaluating the effect of food presence on ABC absorption suggest that, overall, this drug can be given with or without food.235 The oral solution and tablets can be used interchangeably because of comparable systemic absorption.5
ABC's plasma protein binding is independent of its concentration and is approximately 50%.2,5 After I.V. administration of 150 mg of ABC, the apparent volume of distribution was 0.86 +/- 0.154 1/kg, which suggests that ABC distributes into extravascular spacing. In four HIV-infected patients, the mean cerebrospinal fluid to plasma concentration ratio was 18% at 90 to 120 minutes after administration of 200 mg of ABC.3,5
ABC is metabolized in the liver through conjugation involving alcohol dehydrogenase and glucuronyl transferase. Because it does not undergo significant oxidation involving the cytochrome P-450 enzyme system, clinically significant interactions between ABC and drugs metabolized by these enzymes are unlikely. The two major inactive metabolites are primarily excreted in the urine and feces. Only 1.2% was excreted in the urine as unchanged ABC. Because renal excretion of ABC is a minor route, this may suggest that dosage adjustment for patients with renal dysfunction is not necessary. Dosage adjustment in hepatic insufficiency is currently unknown.2,5
Dosing and Administration
ABC is available as a 300-mg tablet and as an oral strawberry-banana flavored solution of 20 mg/ml.4 The recommended dose for adults is 300 mg twice daily; in children age 3 months to 16 years, the recommended dose is 8 mg/kg twice daily (up to a maximum of 300 mg twice daily). ABC can be taken without regard to meals. Dosage adjustment in renal and hepatic insufficiency is currently unknown.4,5
Adverse Reactions
ABC is associated with a hypersensitivity reaction that is seen in approximately 5% of patients. This reaction is not dose-related. It usually occurs within the first 6 weeks of therapy, but it may be observed at any time during treatment. The initial presentation of the hypersensitivity reaction usually involves fever, skin rash (urticarial or maculopapular), fatigue, nausea, vomiting, or abdominal pain. Myalgias, arthralgias, parethesias, and elevated liver enzymes (AST and ALT) also have been observed. Patients who develop a skin rash or two or more of the other symptoms should seek medical attention and immediately discontinue ABC.
Rechallenge of ABC following the hypersensitivity reaction can be potentially fatal and should not be readministered under any circumstances. Patients must be taught that they should never begin ABC again if it has been stopped because of a hypersensitivity reaction. Such patients should then consider themselves "allergic" to ABC in the same way one would consider a penicillin allergy. Health care providers should report hypersensitivity reactions to the ABC Hypersensitivity Registry by calling 1-800-270-0425. A Medication Guide (see Figure 1) and a Warning Card (see Figure 2) are included with each new prescription and refill. Patients should be instructed to carry the Warning Card with them.2,3,6
The use of ABC alone or in combination with other NRTIs has been associated with lactic acidosis and severe hepatomegaly with steatosis. Risk factors that may be associated with this adverse event include obesity and prolonged need for nucleoside analogues. Patients who develop clinical laboratory evidence of lactic acidosis or hepatotoxicity should discontinue nucleoside analogue therapy (including ABC).4 More common adverse effects include nausea, vomiting, rash, headache, loss of appetite, malaise, and fatigue.3,4,8
Resistance Patterns
High-level resistance to the NRTIs is associated with the development of specific mutations on the HIV-1 reverse transcriptase gene.9 HIV-1 isolates with decreased sensitivity to ABC have been selected in vitro. The mutations that HIV-1 selects in the presence of ABC include codons 65, 74, 115, and 184. These codons are similar to the mutations observed with other NRTIs including didanosine, zalcitabine, and lamivudine.2 The mutations at codons 74 and 184 have been the most frequently observed. Additionally, sensitivity to ABC appears to be reduced in patients who are resistant to two or more NRTIs, specifically zidovudine or lamivudine.10 HIV-1 isolates that are resistant to multiple NRTIs will most likely demonstrate cross-resistance to ABC.2,4,10
Preliminary Results
ABC has been studied as a part of triple nucleoside combinations and in combinations with protease inhibitors. Initial treatment of the HIV-infected patient should include two NRTIs and a protease inhibi-, tor.' However, triple NRTIs may be an alternative initial therapy; this is currently being evaluated.
In an open-label, randomized study, 74 therapy-naive patients were treated with ABC 300 mg twice daily in combination with one of the following protease inhibitors: amprenavir 1,200 mg b.i.d., indinavir 800 mg t.i.d., ritonavir 600 mg b.i.d., nelfinavir 750 mg t.i.d., or saquinavir (soft gel capsules) 1,200 mg t.i.d. In an intention-to-treat analyses, this study demonstrated that 41% to 59% of patients achieved plasma HIV RNA levels of less than 400 copies/ml at 48 weeks. Of these patients, 44% to 60% had plasma HIV RNA levels of less than 50 copies/ml at 48 weeks.
In this study, the most common adverse effects included diarrhea, nausea, vomiting, malaise and fatigue, headache, cough, skin rash, and fever/chills. The hypersensitivity reaction to ABC occurred in four of these patients. Long-term suppression of HIV RNA and disease progression greater than 96 weeks using ABC have not been established.2,11,12
Efavirenz (Sustiva)
Mechanism of Action
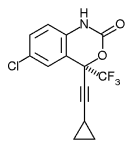
Efavirenz (EFV) belongs to the class of antiretroviral medications known as non-nucleoside reverse transcriptase inhibitors (NNRTIs). Nevirapine (Viramune) and delavirdine (Rescriptor) are two other NNRTIs with Food and Drug Administration (FDA) approval for HIV-1 treatment.
The NNRTIs exert their antiretroviral effect by noncompetitive inhibition of HIV-1 reverse transcriptase (RT).13 Like other NNRTIs, EFV works by binding to a hydrophobic pocket adjacent to the enzyme-active site. Thus, EFV does not compete with NRTIs.13,14
Pharmacokinetics
The pharmacokinetic parameters of EFV make it an attractive antiretroviral medication and justify its oncedaily dosing. EFV has a terminal half-life (tA) of 52 to 76 hours following single doses and 40 to 55 hours after multiple doses.15 The decrease in the tS after multiple doses is due to the ability of EFV to induce its own metabolism.16 In HIV-infected patients, time-to-peak plasma concentrations are reached in 3 to 5 hours and steady-state plasma concentrations are achieved in 6 to 10 days.ls
EFV exhibits high plasma protein binding (99.5% to 99.75%), predominantly to albumin. Cerebrospinal fluid (CSF) concentrations approximate 0.69% of corresponding plasma concentrations.is The bioavailability of EFV is increased by 50% on average when taken with foods high in fat.tS Although the manufacturer states EFV may be taken without regard to meals, they do caution against administering doses with high-fat meals.16
EFV is principally metabolized into inactive metabolites in the liver by the cytochrome P-450 system. The major isoenzymes responsible are CYP3A4 and CYP2D6. EFV has been shown to both induce and inhibit cytochrome P-450 enzymes.13 Drugs metabolized by the same enzyme system could potentially interact with EFV and result in altered plasma concentrations of the coadministered drug or of EFV. Clinicians should use caution in administering EFV to patients with compromised hepatic function.15,18
Dosing and Administration
The recommended adult dosage of EFV is 600 mg daily, in combination with other antiretroviral drugs, typically a protease inhibitor and/or NRTI(s). Patients should be instructed to take EFV at bedtime to improve the tolerability of CNS adverse effects. EFV is approved for use in pediatric patients age 3 years and older, weighing greater than 10 kilograms. Dosing is based on weight and is described in the EFV product information insert. EFV can be taken with or without food; however, a high-fat meal may increase the absorption of EFV, which may potentially increase the CNS adverse effects.
Fetal abnormalities have been seen in EFV-treated monkeys. Pregnancy should be avoided in women treated with EFV, and patients should be instructed to use a method of barrier contraception. A pregnancy test should be performed prior to EFV initiation.15
Adverse Reactions
The most commonly occurring adverse effects reported with EFV are those related to the central nervous system (CNS). Of the 2,215 patients studied prior to FDA approval of EFV 52% experienced some type of CNS symptom such as dizziness, somnolence, insomnia, abnormal dreaming, confusion, impaired concentration, depression, nervousness, hallucinations, or euphoria.15,24 These symptoms begin within 1 to 2 hours after EFV dosing and generally lessen in frequency and severity over time. Most patients report resolution within a few weeks.15
Dermatologic adverse effects are also common with EFV use. During clinical trials, approximately 25% of EFV-treated patients experienced skin rash, compared with 17% in the control groups. The rashes reported were usually mild to moderate maculopapular skin eruptions that presented within the first 2 weeks of therapy initiation and resolved within 1 month of continued therapy. In clinical trials, children experienced a greater incidence and severity of skin rash.15
Other adverse events associated with EFV are gastrointestinal disturbances (nausea, vomiting, diarrhea) and fatigue. Elevation of liver enzymes, serum triglycerides, and cholesterol also have been reported."
Drug Interactions
Because of the metabolic pathway of EFV, certain drugs should not be administered concurrently due to the potential for precipitating serious or life-threatening adverse events such as cardiac arrhythmias, prolonged sedation, or respiratory depression. Such drugs include astemizole, cisapride, midazolam, triazolam, or ergot alkaloids.15
An interaction between EFV and the macrolide antibiotic clarithromycin has been observed. Benedek and colleagues showed a 39% reduction in the area under the curve of clarithromycin and an increase by 34% in clarithromycin's active metabolite (14-OH clarithromycin) when administered with EFV.21 The clinical significance of this interaction is unknown, but the manufacturer recommends using azithromycin if a macrolide antibiotic is needed with EFV.15
Resistance Patterns
The predominantly observed reverse transcriptase mutation leading to EFV resistance is the K103N mutation. An abstract by Jeffrey, et al. reported a 19-fold loss of activity of EFV against the K103N mutant strain. The double mutants Y188L and S48T/G190S have also been seen but to a lesser degree.2526 Crossresistance to other NNRTIs have been observed in vitro.15 Crossresistance of EFV and protease inhibitors is unlikely because of the different enzymes targeted to suppress HIV replication.15
Current Use in Therapy
The Guidelines for the use of Antiretroviral Agents in HIV-Infected Adults and Adolescents (December 1998) includes EFV as a preferred antiretroviral drug for treatment of established HIV infection in combination with two NRTI drugs. EFV is the only NNRTI to achieve this status. Both nevirapine and delavirdine are listed as alternative drugs; they have both been successful in suppressing HIV-1 RNA to undetectable levels in the majority of patients receiving therapy for more than 28 weeks when given in combination with two NRTIs. However, EFV-containing regimens compare favorably with protease inhibitorcontaining regimens in achieving undetectable HIV-1 RNA levels for patients remaining on therapy for greater than 36 weeks.15,26
EFV can be used in PI- and NNRTI-naive patients as part of a combination regimen with two NRTIs for those patients who wish to delay protease inhibitor use. This combination would also be an alternative for patients who experienced intolerable adverse events when taking PIs. A combination of EFV with the protease inhibitor indinavir aDV) was shown to be effective and may be an alternative for patients who cannot tolerate NRTIs.
Riddler and colleagues presented the results of their study at the 12th World AIDS Conference in Geneva." In patients randomized to receive EFV 600 mg at bedtime plus IDV 1,000 mg q8h, 89% had undetectable HIV-RNA levels (
Conclusion
ABC and EFV are two potent new additions to the antiretroviral regimens used to treat patients with HIV infection. Treatment decisions are complex and involve a thorough understanding of all currently available antiretroviral agents and the patient's treatment history. Although these decisions should be made by providers who are experienced in the management of HIV infection, it is important that all providers are aware of the implications and potential complications in using these therapies.
REFERENCES
Guidelines for the Use Of Antiretrovirals Agents in HIV-Infected Adults and Adolescents. MMWR 1998;47(RR-5).
Ziagen general information. Glaxo Wellcome Inc. Medical Services, Research Triangle Park, N.C.,January 6, 1999.
Foster RH, Faulds D: Abacavir. Drugs 1998;55: 729-36.
Product Information, Ziagen, abacavir. Glaxo Wellcome Inc., Research Triangle Park, N.C., 1998.
Pharmacokinetics of Ziagen. Glaxo Wellcome Inc. Medical Services. Research Triangle Park, N.C., January 4, 1999.
Ziagen hypersensitivity reactions. Glaxo Wellcome Inc. Medical Services, Research Triangle Park, N.C.January 6,1999. DRUGDEX(R): Abacavir: Drug Evaluation. Micromedex, Inc., Englewood, Colo., Revised 12/98.
Saag MS, Torres RA, Sonnerborg A, et al.: Antiretroviral effect and safety of abacavir alone and in combination with zidovudine in HIVinfected adults. AIDS 1998;12:F203-F209. VanLaethem K, Witvrouw M, Schmit JC, et al.: The multiple nucleoside analogue resistance mutations confer cross-resistance to abacavir (abstract). 6th Conference on Retroviruses and Opportunistic Infections,January 31, 1999:113.
Kuritzkes D: Clinical implications of antiretroviral resistance. HIV Clinical Management. Medscape, Inc., New York, N.Y 1999;13. Glaxo Wellcome Inc. Medical Services: Efficacy and durability of Ziagen. March 9,1999.
Glaxo Wellcome Inc. Medical Services: Ziagen In combination With Agenerase and Efavirenz. January 6, 1999.
Holtzer CD, Coleman RL: Use of nonnucleoside reverse transcriptase inhibitors. AmJ Health-Sys Pharm 1998;55:283-87. 14. Dobkin J: Efavirenz receives FDA approval. Infect Med 1998;15(i1):747. Product Information: Sustiva, efavirenz. DuPont Pharmaceuticals. Wlmington, Del., 1998.
16. DRUGDEX(R): Efavirenz: Drug evaluation. Micromedex, Inc., Englewood, Colo., Revised 12/98.
17. Tashima KT, Caliendo AMC, Ahmad MA, et al.: Cerebrospinal fluid HIVI RNA levels and efavirenz concentration in patients enrolled in clinical trials (abstract no. 32202). 12th World AIDS Conference Geneva, Switzerland, June 28, 1998.
18. Fiske W, Benedek I, Brennan J, et al.: Pharmacokinetics of efavirenz in subjects with chronic liver disease (abstract no. 367). 6th Conference on Retroviruses and Opportunistic Infections, January 31,1999. 19. Fiske WD, Benedek IH, Joseph JL, et al.: Pharmacokinetics of efavirenz and ritonavir after multiple oral doses in healthy volunteers (abstract no. 42269). 12th World AIDS Conference Geneva, Switzerland, June 28, 1998. 20. Fiske WD, Benedek IH, White SJ, et al.: Pharmacokinetic interaction between efavirenz and nelfinavir in healthy volunteers (abstract no. 349). 5th Conference on Retroviruses and Opportunistic Infections. Chicago, Ill., February 1-5, 1998.
21. Benedek IH, Joshi A, Fiske WD, et al.: Pharmacokinetic interaction studies in healthy volunteers with efavirenz and the macrolide antibiotics, azithromycin and clarithromycin (abstract no. 347). 5th Conference on Retroviruses and Opportunistic Infections. Chicago, Ill., February 1-S, 1998.
22. Benedek IH, Joshi A, Fiske WD, et al.: Pharmacokinetic interaction between efavirenz and rifampin in healthy volunteers (abstract no. 42280). 12th World AIDS Conference Geneva, Switzerland, June 28, 1998. 23. Joshi AS, Fiske WD, Benedek IH, et al.: Lack of a pharmacokinetic interaction between efavirenz and ethinyl estradiol in healthy female volunteers (abstract no. 348). 5th Conference on Retroviruses and Opportunistic Infections. Chicago, Ill., February 1-5,1998.
24. Ruiz NM, Bessen LJ, Manion DJ, et al.: Potential adverse experiences associated with efavirenz in adults (abstract no. 655). 6th Conference on Retroviruses and Opportunistic Infections, January 31, 1999. 25. Jeffrey S, Baker D, Tritch C, et al.: A resistance and cross-resistance profile for sustiva (Efavirenz, DMP 266) (abstract no. 702). 5th Conference on Retroviruses and Opportunistic Infections. Chicago, Ill., February 1-5, 1998.
26. Bacheler H, George H, Hollis G, et al.: Resistance to efavirenz (Sustiva) in vivo (abstract no. 703). 5th Conference on Retroviruses and Opportunistic Infections. Chicago, Ill., February 1-5,1998.
27. Riddler S, Kahn J, Hicks C, et al.: Durable clinical Anti-HIV-1 activity (72 weeks) and tolerability for efavirenz (DMP 266) in combination with indinavir (IDV) (abstract no. 12359). 12th World AIDS Conference Geneva Switzerland, June 28, 1998.
Barbara D. Klaus, RN, ANP, CS, MSN, editor of this column, is a Nurse Practitioner at the Infectious Disease Section, Veterans Affairs Medical Center, Denver, and is also on the clinical faculty of the School of Nursing, University of Colorado Heaith Sciences Center.
Michael J. Grodesky RN, ANP, CS, MS, co-editor of this column, is a Nurse Practioner in the Infectious Disease Group Practice at University Hospital in Denver. He is also on the clinical faculty of the University of Colorado Health Sciences Center School of Nursing.
ABOUT THE AUTHORS
Jane Wolbach, PharmD, is a clinical pharmacy specialist in the Infectious Disease Group Practice Pharmacy at University Hospital in Denver, and a member of the University of Colorado Health Sciences Center School of Pharmacy adjoint faculty.
Kam Capoccia, RPh, PharmD(c), is a clinical pharmacist who is completing her doctorate in pharmacy at the University of Colorado Health Sciences Center School of Pharmacy.
Copyright Springhouse Corporation Jun 1999
Provided by ProQuest Information and Learning Company. All rights Reserved