* Context.-Bioelectronic sensors, which combine microchip and biological components, are an emerging technology in clinical diagnostic testing. An electronic detection platform using DNA biochip technology (eSensor) is under development for molecular diagnostic applications. Owing to the novelty of these devices, demonstrations of their successful use in practical diagnostic applications are limited.
Objective.-To assess the performance of the eSensor bioelectronic method in the validation of 6 Epstein-Barr virus-transformed blood lymphocyte cell lines with clinically important mutations for use as sources of genetic material for positive controls in clinical molecular genetic testing. Two cell lines carry mutations in the CFTR gene (cystic fibrosis), and 4 carry mutations in the HFE gene (hereditary hemochromatosis).
Design.-Samples from each cell line were sent for genotype determination to 6 different molecular genetic testing facilities, including the laboratory developing the DNA biochips. In addition to the bioelectronic method, at least 3 different molecular diagnostic methods were used in the analysis of each cell line. Detailed data were collected from the DNA biochip output, and the genetic results were compared with those obtained using the more established methods.
Results.-We report the successful use of 2 applications of the bioelectronic platform, one for detection of CFTR mutations and the other for detection of HFF mutations. In all cases, the results obtained with the DNA biochip were in concordance with those reported for the other methods. Electronic signal output from the DNA biochips clearly differentiated between mutated and wild-type alleles. This is the first report of the use of the cystic fibrosis detection platform.
Conclusions.-Bioelectronic sensors for the detection of disease-causing mutations performed well when used in a "real-life" situation, in this case, a validation study of positive control blood lymphocyte cell lines with mutations of public health importance. This study illustrates the practical potential of emerging bioelectronic DNA detection technologies for use in current molecular diagnostic applications.
Emerging technologies that incorporate biological elements into microchip-based devices have resulted in the development of novel clinical diagnostic methods, particularly in the area of clinical molecular genetics (reviewed in McGlennen1). Nucleic acid-based bioelectronic sensors are one of many applications of these technologies that hold promise for low-cost, automated diagnostic systems.
Nucleic acid-based bioelectronic detection involves the generation of an electronic signal mediated by nucleic acid hybridization and serves as the basis for the eSensor DNA detection technology (Motorola Life Sciences, Pasadena, Calif).2-4 The technical specifications of the eSensor platform have been described previously.4 The method is based on hybridization between 3 single-stranded DNA molecules: a DNA capture probe, a target DNA, and an electrically active DNA signal probe. DNA capture probes of approximately 21 bases are immobilized in specified patterns on low-density arrays of gold electrodes on printed circuit boards. The capture probes are specific for a region of the target molecule flanking the site of polymorphism with a sequence in common for all genotypes. Unlabeled target DNA molecules, which in a clinical situation would be derived from patient samples, are added to the immobilized capture probes together with the DNA signal probes. The signal probes are specific for either the mutant or the wild-type target sequence, and are labeled with 1 of 2 different ferrocene-derivative DNA oligonucleotides (designated I and II) that have unique electrochemical potentials, and that generate detectably different signals.5,6 Each target DNA molecule hybridizes to both a signal probe and an immobilized capture probe, thus bringing the ferrocene label of the signal probe into close proximity with the gold electrode, leading to the generation of a characteristic electrical signal that identifies the sequence of the target. Existing eSensor DNA arrays contain up to 36 electrodes for the simultaneous detection of multiple DNA mutations or polymorphisms from a single sample of target DNA.
In this study, the eSensor platform was used as part of an ongoing clinical validation process for several Epstein-Barr virus (EBV)-transformed blood lymphocyte cell lines carrying cystic fibrosis (CF; CFTK gene; OMIM 602421) and hereditary hemochromatosis (HHC; HFE gene; OMIM 235200) mutations, which were under development for use as positive controls in molecular diagnostic testing.7,8 Positive control material is not readily available for many mutations of public health importance, and the lack of these materials has been described as "the issue of utmost urgency" for clinical genetic testing.9,10 Blood lymphocyte cell lines are extremely long-lived and can provide a reliable, virtually unlimited supply of control material for molecular genetic testing applications.11,12 The cell lines described in this study will provide valuable source material for several important mutations.
The cell lines described here are part of a larger study involving 21 cell lines and 11 genetically based diseases. This study seeks to develop a method to derive stable lymphoblastoid cell lines from residual, anonymous clinical blood samples with mutations of public health importance, and to validate the cell lines as high-quality sources of positive control material for molecular genetic testing. The results of the larger study, including the results of other phases of the clinical validation, will be reported elsewhere. Bioelectronic detection was used for analysis of the CFTR and HFE mutations in the 6 cell lines described in this article. In an earlier phase of the study, these cell lines had been shown to be viable and uncontaminated. The mutation status of the cell lines had also been previously determined, and the mutations were demonstrated to be stable through 20 population doublings in culture.
Two of the cell lines carry CF mutations. Cystic fibrosis is the most prevalent serious inherited disease of childhood, with more than 1000 known mutations in the CFTR gene,13 and has a carrier frequency estimated at 1:25 in non-Hispanic white, including Ashkenazi Jewish, populations.14 The American College of Medical Genetics (ACMG) has developed a panel of 25 mutant CF alleles that are recommended for general population screening and diagnostic testing.15 The 2 CF cell lines used in this study are each compound heterozygous for mutations included in the ACMG panel ([Delta]F508,16 621+1G>,17 3120+1G>lA,18 and R117H19), and the 3 common variants of the T allele (5T, 7T, and 9T) are also represented. T-allele status alone is rarely associated with particular health consequences; however, it can influence the clinical effects of certain CF mutations20 and is therefore included in some CF testing. The CFTR cell lines were derived from stock cultures obtained from the National Institute of General Medical Sciences (NIGMS) Human Genetic Cell Repository and were known to carry mutations in the CFTR gene. The NIGMS cell lines are currently available to researchers and clinicians; however, they were incompletely characterized, and although some of the mutations in these cell lines had been confirmed, the cell lines had not undergone rigorous validation for use as positive controls for clinical molecular genetic testing. We provide additional information on the status of the CFTR gene in these 2 cell lines, including T-allele status, and show that they perform well as positive controls for a variety of clinical molecular genetic testing methods, including the eSensor bioelectronic method. Additional validation studies on these cell lines will be reported elsewhere.
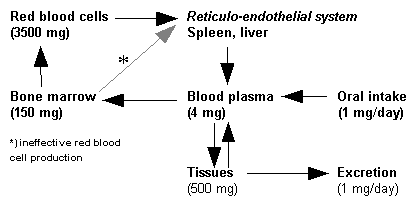
Four cell lines with mutations in the HFE gene were derived from anonymous, residual clinical blood samples. HFE mutations result in HHC, which is characterized by abnormally high iron absorption and has a variety of potentially serious consequences, including hepatic fibrosis or cirrhosis, diabetes mellitus, and congestive heart failure. The mutation frequency has been estimated to exceed 10% in the general population.21 Hereditary hemochromatosis responds well to treatment; however, symptoms generally appear after 40 years of age, and irreversible organ system damage may have already occurred. Early diagnosis, which could be aided by the use of genetic testing, is critical for successful management of the disease. Three mutations have been associated with HHC (C282Y, H63D, and S65C22), and all of these are represented in the 4 HFE cell lines used in this study. Cell lines with mutations in the HFE gene are available from the NIGMS collection; however, as with the CF cell lines, they have not undergone a rigorous clinical validation, and none has been characterized for the recently described S65C mutation.
For this study, frozen cell pellets from each cell line were sent to molecular genetic testing facilities for analysis using a variety of molecular techniques. The eSensor bioelectronic DNA detection platform was included together with more traditional methods. In all cases, the mutations previously detected in the cell lines were correctly identified. This study illustrates an important use of bioelectronic sensor technology in a current molecular genetic testing application.
MATERIALS AND METHODS
Cell Lines and Performing Laboratories
The following laboratories participated in the testing of the cell lines: Greenwood Genetic Center, Greenwood, SC; DNA Diagnostic Lab, Henry Ford Hospital, Detroit, Mich; Genetics Laboratory, University of Tennessee Medical Center, Knoxville; Laboratory Corporation of America, Research Triangle Park, NC; H. A. Chapman Institute of Medical Genetics, Tulsa, Okla; Molecular Diagnostics Laboratory, SUNY Upstate Medical University, Syracuse, NY; Molecular Genetics Laboratory, Mayo Clinic, Rochester, Minn; and Motorola Life Sciences, Pasadena, Calif.
The 2 EBV-transformed cell lines with CFTR mutations were originally obtained from the NIGMS Human Genetic Cell Repository at Coriell Cell Repositories (Camden, NJ). CF1 and CF2 were derived from GM07441 and GM13591, respectively. The NIGMS cell lines had been previously determined to carry the CFTR mutations 3120 + 1G> A (GM07441), and [Delta]F508 and R117H (GM13591). During preliminary characterization of CF1 and CF2 for the clinical validation process described in this report, the previously described mutations were confirmed, and an additional mutation (621 + 1G>T) was identified in CF1. The T-allele status for each cell line was determined (7T/9T for CFl and 5T/ 9T for CF2).
Four blood lymphocyte cell lines with mutations in the HFE gene were established from anonymous, residual clinical blood samples using standard EBV transformation protocols as previously described.12 The result of the original clinical test was known for each residual blood sample at the time of EBV transformation, and the mutations were confirmed in the transformed cell lines after viability was established. Epstein-Barr virus transformation and cell line culture were performed at Coriell Cell Repositories.
Each EBV-transformed cell line was originally derived from an individual donor subject, and no cell line mixtures were used. Quality control procedures at Coriell Cell Repositories ensure that all cell lines are free from mycoplasmic, microbial, or fungal contamination and from cross-contamination by other cell lines. Appropriate institutional review board approvals were obtained for all institutions participating in this project. The mutations in both the CFTR and HFE cell lines were determined to be stable through five 10-fold expansions (approximately 20 population doublings) in culture.
The mutations present in the 6 cell lines are shown in Table 1. Frozen cell pellets of approximately 1.5 × 10^sup 7^ cells were prepared from each cell line, sufficient to yield at least 100 µg DNA on extraction by most methods. Cell pellets from each cell line were shipped on dry ice to 6 laboratories for DNA extraction and molecular genetic testing, performed per local standard procedures. Several different genetic testing methods were used for each cell line (Table 2).
Genotyping by Bioelectronic Detection
DNA Samples and Polymerase Chain Reaction Amplification.-To facilitate the use of this novel technology, the laboratory using bioelectronic detection methods (Motorola Life Sciences) was informed of the gene to analyze in each cell line (HFE or CFTR) and of the mutations present, but not of the specific genotype of any particular cell line. DNA was purified from frozen cell pellets using the Epicentre Technologies (Madison, Wis) MasterPure extraction kit. Purified DNA samples were checked for degradation using agarose gel electrophoresis (no degradation was detectable), and DNA concentrations were determined by UV spectrophotometry. Polymerase chain reaction (PCR) primers are shown in Table 3. One primer from each pair was labeled with biotin to facilitate removal of 1 DNA strand from each amplified product following PCR. Samples for analysis of the HFE mutations H63D and C282Y were amplified in duplex. (Note: The version of the eSensor platform used in this study was not designed to detect the HFE S65C mutation.) The PCR reaction mixes included 100 ng genomic DNA, 0.3 µM of each primer, 800µM deoxynucleotide triphosphate mixture (dNTP), 5 µL 10× PCR buffer (Invitrogen, Carlsbad, Calif), 1mM magnesium chloride, and 5 U Platinum Taq DNA polymerase (Invitrogen) in a final volume of 50 ×L. Hot-start PCR was carried out with a model PTC-200 thermal cycler (MJ Research Inc, Watertown, Mass) programmed as follows: initial sample denaturation at 95°C for 5 minutes, followed by thermal cycling (95°C for 45 seconds, 59°C for 60 seconds, and 72°C for 45 seconds) for 40 cycles, followed by an extension step at 72°C for 10 minutes. Polymerase chain reaction products were examined by agarose gel electrophoresis and ethidium bromide staining.
For analysis of the CF mutations R117H, 621 + 1G>A, F508, and 3120 + 1G>A, 3 PCR amplicons were used (Table 3). The PCR reactions were carried out in triplex. The reaction mixes contained 200 ng genomic DNA, 0.35 µM of each primer, 400µM dNTP, 10 µL 10× PCR buffer, 3mM magnesium chloride, and 5 U HotStar TaqTM DNA polymerase (Qiagen, Valencia, Calif) in a final volume of 100 µL. Hot-start PCR was carried out with a PTC-200 thermal cycler, programmed as follows: initial sample denaturation at 95°C for 5 minutes, followed by thermal cycling (94°C for 30 seconds, 54°C for 30 seconds, and 72°C for 30 seconds) for 45 cycles, followed by an extension step at 72°C for 10 minutes. The PCR products were examined by agarose gel electrophoresis and ethidium bromide staining.
Biotin-labeled, single-stranded DNA was removed from the double-stranded PCR products so that only the strand of interest (the unlabeled strand) would be available for analysis by the eSensor DNA detection system. Briefly, M-280 streptavidin magnetic beads (Dynal, Lake Success, NY) were prepared according to the manufacturer's protocol. Approximately 90 µL of magnetic bead solution was added to approximately 45 µL of each PCR product, and the samples were incubated at room temperature for 30 minutes with slight agitation. The beads with bound double-stranded amplicon were magnetically separated, and the supernatants were removed by aspiration. The beads were then resuspended in 20 µL of a denaturing solution of 0.1M sodium hydroxide for 5 minutes at room temperature, again magnetically separated, and the supernatants containing unlabeled single-stranded (ss-) amplicon were then harvested and neutralized with 10 µL 0.2M hydrogen chloride at room temperature. The DNA solutions were either used immediately or stored until use at -20°C.
Genotype Determination Using the eSensor Hybridization Platform.-For HFE genotyping, both HFE-C (C282Y) and HFE-H (H63D) were detected on a single chip. The cocktail for genotype analysis contained the ss-amplicons from the duplex PCR reaction and all 4 HFE signaling probes (Table 4). The CF detection system included capture probes for all 25 CF mutations in the ACMG-recommended screening panel plus T-allele variants, arrayed on 2 DNA chips. Genotyping of the 4 CF cell lines was performed twice. In the first instance, the cocktails contained the ss-amplicons from the triplex PCR reaction described above plus signaling probes for the wild-type and mutated sequences of interest (Table 4). In the second instance, cocktails were prepared that contained PCR amplicons and capture probes for all 25 CF mutations on the chips, plus the T-allele (primer, capture probe, and signal probe sequences for mutations not targeted in this study are not shown).
The cocktail for both HFE and CFTR genotyping included 70 µL hybridization buffer (containing 0.8M untreated hybridization buffer, 1mM 6-mercapto-1-hexanol, 1% fetal bovine serum, and 125nM of each HFE or CF signaling probe), which was added to the ss-amplicon samples. Samples were injected into the chips and incubated for 2 hours at 40°C. The chips were then scanned with an eSensor 4800 Reader to determine the genotypes of the samples.
Detection Platform Optimization.-At the time of this study, the biochips for CFTR and HFE mutation detection were still under development at Motorola Life Sciences. The DNA detection platform was tested, and hybridization conditions were optimized to ensure that no nonspecific electrical signals would be generated. Initial hybridization conditions were also optimized for specific binding of target DNAs, using both target mimic oligonucleotides (Table 5) and biologically derived samples known to be positive or negative for the mutations of interest. These tests would generally not need to be performed in standard clinical use. First, hybridization experiments using only signal probes (Table 4) and capture probes (Table 6) were done, in which each capture probe was tested for hybridization with increasing numbers of different signal probes to confirm that no electrical signal could be detected in the absence of the target molecule. Second, hybridization was performed using a signal probe cocktail, which contained all the signal probes for either HFE or CFTR, as appropriate, and 1 or increasing numbers of different target mimics to identify any cross-reactivity that could result in the generation of a signal in the absence of exact sequence complementarity. Third, hybridization of individual amplicons, generated by PCR of DNA derived from anonymous patient specimens, was performed in the presence of the signal probe cocktail. Conditions were optimized in all cases so that target DNAs bound as desired to their specific capture probes, and no nonspecific cross-reactivity was detected. It was sometimes necessary to introduce mismatched base pairs into the sequence of the capture probe to minimize electrical signals resulting from nonspecific cross-reactivity of the target molecules with the capture probes (data not shown).
Other Testing Methods.-A variety of commonly used molecular genetic testing techniques were used by the other laboratories. Details of the experimental principles have been described previously.23 For analysis of the CFTR gene, most laboratories used multiple methods to determine and/or confirm sample genotype. Four laboratories used direct DNA sequence analysis, which was generally performed following amplification of the region(s) of interest by PCR. Another common technique involved restriction fragment length polymorphism analysis, in which the region of interest was amplified using PCR, then digested with 1 or more restriction enzymes. The presence of a particular mutation may create or destroy a restriction site, and the DNA fragments produced following restriction enzyme digestion show characteristic banding patterns when electrophoretically separated. Two laboratories used commercial kits. The Roche CF-31 Linear Array from Roche Molecular Diagnostics (Pleasanton, Calif) is a strip-based assay, in which multiplex PCR using biotinylated primers amplifies the regions of interest. The amplification products are then hybridized to strips with linear arrays of bands specific to each potentially mutated site. The hybridization pattern indicates the genotype of the sample and is visualized using streptavidin-peroxidase and tetramethyl benzidine. The ABI Cystic Fibrosis Assay from Applied Biosciences (Foster City, Calif) also starts with a multiplex PCR. The amplified fragments are then hybridized to fluorescently labeled probes against nonpolymorphic regions of the gene adjacent to potential mutation sites, as well as to probes with mobility-modifying tails that are specific for either the mutant or wild-type sequence. The hybridized fluorescently labeled probes are then ligated to the mobility-modified probes to yield DNA fragments with unique combinations of mobility and fluorescence, which on analysis allow determination of the genotype. Three laboratories used mutation scanning techniques, including conformation sensitive gel electrophoresis and other types of heteroduplex analysis. These techniques take advantage of the change in mobility of double-stranded DNA fragments under particular conditions that result when the 2 strands are slightly mismatched, for example, when a wildtype strand hybridizes with a strand containing a point mutation. The mobility differences can be detected by various electrophoretic methods.
The most commonly used method for detecting HFE mutations was restriction fragment length polymorphism. One laboratory used the LightCycler (Roche Diagnostics Corporation, Indianapolis, Ind). This automated system performs PCR using sequencespecific primers for mutated and/or unmutated sites, then analyzes melting curves of the PCR products and primers to determine genotype.
RESULTS
For the 6 B-lymphocyte cell lines undergoing validation, all testing laboratories and all methods correctly detected the known mutations (see Table 1), except where the laboratory did not test for a particular mutation.
For bioelectronic detection using the eSensor DNA platform, DNA capture probes are covalently bound in defined patterns to gold electrodes arrayed on printed circuit boards and are subsequently hybridized to target DNA derived from the sample undergoing testing and electrically active signal probes specific for mutant or wild-type DNA. This results in the generation of characteristic electronic signals, which indicate the genotype of the target sample.
The results of eSensor genotyping for the 4 HFE cell lines are shown in Figure 1. Two different ferrocene-derivative oligonucleotide signaling moieties with different electrochemical potentials are used for wild-type and mutant sequences, and the signal generated by the particular combination of bound signal probe is unique to each genotype. As mentioned previously, this version of the DNA biochip was not designed to detect S65C, so a genotype of WT/WT was reported for HFE4.
The results of CF genotyping are shown in Figure 2. The nanoampere signals shown were generated using target produced by triplex PCR for the mutations of interest as described in the "Methods and Materials" section. Genotyping for the entire set of 25 CF mutations and the T-allele yielded the same genetic results as the restricted primer set, plus T-allele status. In all instances for both CF and HFE cell lines, there was perfect concordance between the mutations detected by the eSensor method and those detected by other types of genetic analysis. The electro-chemical signal data for T-allele analysis are not presented here. The T-allele has 3 primary forms (5T, 7T, and 9T); however, only 2 different ferrocene labels are used in this system. Detection requires unique combinations of hybridization reactions and specially designed probes using both labels to differentiate between the 3 forms of the allele. Graphic representation of the nanoampere signals is not practical. In a clinical situation, the electrochemical signals are processed within the biochip and displayed as a genotype to the end user.
COMMENT
This study illustrates the successful use of the eSensor bioelectronic detection system in the validation of 6 blood lymphocyte cell lines for use as positive controls for cystic fibrosis and hereditary hemochromatosis mutations in molecular genetic testing.
The version of the eSensor HFE chip used for the validation of the HFE cell lines did not examine specimens for the HFE S65C mutation, principally due to lack of availability of the needed signaling probes specific for S65C. Thus, a result of WT/WT for cell line HFE4, which has the genotype S65C/WT, was reported for this testing method. All other laboratories participating in this study reported a genotype of S65C/WT for the cell line HFE4. Many laboratories do not include the S65C mutation in their standard HFE testing. Although S65C has been associated with mild disease in some studies,22 the clinical significance remains unclear, and many clinicians consider it a benign polymorphism. However, because of its close proximity to the site of the H63D mutation (see Figure 3), the presence of S65C can interfere with testing for H63D. Difficulties arise primarily with methods that rely on DNA hybridization, as opposed to direct DNA sequence analysis or restriction fragment length polymorphism. Like H63D, S65C introduces a single-base mismatch when hybridized to a wild-type sequence, and depending on the design of the assay, could produce changes in mobility and/or melting temperature similar to those seen with H63D, resulting in a false-positive result. In assays that use allele-specific oligonucleotide hybridization to detect mutations, the presence of an S65C mutation could potentially interfere with binding of both wild-type-specific and H63D-specific sequences, giving an erroneous result. Although we did not test all possible allelic combinations, in the case of the eSensor, the presence of the S65C mutation in cell line HFE4 did not result in a false-positive result for H63D. The mutation occurs within the region of the target DNA that is complementary to the signaling probe (Figure 3); however, the design of the eSensor detection system allowed accurate determination of the genotype in this case. During initial development of the H63D assay at Motorola, the potential for interference in genotyping between closely spaced mutations was examined using target mimics (76mers) for various genotypes of H63D, some of which also contained the S65C polymorphism. In these tests, the correct H63D genotype was always obtained.
The successful use of the eSensor DNA detection system in the validation of these cell lines demonstrates this platform's utility for multiplex detection of polymorphisms. The eSensor system technology could serve in numerous capacities, not only for research/development and clinical genetic testing applications, but also for pharmacogenetics, infectious disease test panels, and industry. The small panel sizes used in this study are useful models for arrayed platforms, and it is anticipated that clinical and/or commercial implementation of medically appropriate diagnostic panels will have significantly higher densities, in the tens to hundreds of analytes range.
This work was supported by contract 200-2000-10050 from the Centers for Disease Control and Prevention, Atlanta, Ga. The authors thank Ana Stankovic, MD, PhD, and Laurina Williams, PhD, in the Public Health Practice Program Office of the Centers for Disease Control and Prevention for their assistance with this project.
References
1. McGlennen RC. Miniaturization technologies for molecular diagnostics. Clin Chem. 2001;47:393-402.
2. Farkas DH. Bioelectronic DNA chips for the clinical laboratory. Clin Chem. 2001;47:1871-1872.
3. Umek RM, Lin SS, Chen Y-P, et al. Bioelectronic detection of point mutations using discrimination of the H63D polymorphism of the Hfe gene as a model. Mol Diagn. 2000;5:321-328.
4. Umek RM, Lin SW, Vielmetter J, et al. Electronic detection of nucleic acids: a versatile platform for molecular diagnostics. J Mol Diagn. 2001;3:74-84. 5. Yu CJ, Wan Y, Yowanto H, et al. Electronic detection of single-base mismatches in DNA with ferrocene-modified probes. J Am Chem Soc. 2001;123:11155-11161.
6. Yu CJ, Wang H, Wan Y, et al. 2'-Ribose-ferrocene oligonudeotides for electronic detection of nucleic acids. J Organic Chem. 2001;66:2937-3942.
7. Stenzel TT, Bernacki SH, Beck JC, et al. Establishment of stably transformed cell lines from residual clinical blood samples for use in performance evaluation and quality assurance in molecular genetic testing. Am J Hum Genet. 2001;69:438.
8. Stenzel TT, Bernacki SH, Beck JC, et al. Use of residual clinical blood samples to establish stable EBV transformed cell lines for PE/QA of molecular genetic testing. Genet Med. 2002;4:212.
9. Williams LO, Cole EC. General Recommendations tor Quality Assurance Programs tor Laboratory Molecular Genetic Tests, Final Monograph. Atlanta, Ga: Centers for Disease Control and Prevention, Public Health Practice Program Office, Division of Laboratory Services; 1999. Available at: http://www.phppo.cdc.gov/dls/pdf/genetics/dyncor.pdf. Accessed September 4, 2003.
10. Williams LO, Cole EC, Lubin IM, Iglesias NI, Jordan RL, Elliott LE. Quality assurance in human molecular genetics testing: status and recommendations. Arch Palhol Lab Med 2003;127:1353-1358.
11. Louie LG, King MC. A novel approach to establishing permanent lymphoblastoid cell lines: Epstein-Barr virus transformation of cryopreserved lymphocytes. Am J Hum Genet. 1991;48:637-638.
12. Beck JC, Beiswanger CM, John EM, Satariano E, West D. Successful transformation of cryopreserved lymphocytes: a resource for epidemiological studies. Cincer Epidemiol Biomarkers Prev. 2001;10:551-554.
13. Riordan JR, Rommens JM, Kerem B, et al. Identification of the cystic fibrosis gene: cloning and characterization of complementary DNA. Science. 1989;245:1066-1073.
14. Richards CS, Bradley LA, Amos J, et al. Standards and guidelines for CFTR mutation testing [published correction appears in Genet Med. 2002;4:471]. Genet Med 2002;4:379-391.
15. Grody WW, Cutting CR, Klinger KW, Richards CS, Watson MS, Desnick RJ, tor the Subcommittee on Cystic Fibrosis Screening, Accreditation of Genetic Services Committee, American College of Medical Genetics. Laboratory standards and guidelines for population-based cystic fibrosis carrier screening. Genet Med. 2001;3:149-154.
16. Kerem B, Rommens JM, Buchanan JA, et al. Identification of the cystic fibrosis gene: genetic analysis. Science. 1989;245:1073-1080.
17. Zielenski J, Bozon D, Kerem B, et al. Identification of mutations in exons 1 through 8 of the cystic fibrosis transmembrane conductance regulator (CFTR) gene. Ceramics. 1991;10:229-235.
18. Macek M Jr, Mackova A, Hamosh A, et al. Identification of common cystic fibrosis mutations in African-Americans with cystic fibrosis increases the detection rate to 75%. Am J Hum Genet. 1997;60:1122-1127.
19. Gervais R, Dumur V, Rigot JM, et al. High frequency of the R117H cystic fibrosis mutation in patients with congenital absence of the vas deferens. N Engl J Med. 1993;328:446-447.
20. Kiesewetter S, Macek M Jr, Davis C, et al. A mutation in CFTR produces different phenotypes depending on chromosomal background. Nature Genet. 1993;5:274-278.
21. Feder JN, Gnirke A, Thomas W, et al. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nature Genet. 1996;13: 399-408.
22. Mura C, Raguenes O, Ferec C. HFE mutations analysis in 711 hemochromatosis probands: evidence for S65C implication in mild form of hemochromatosis. Blood. 1999;93:2502-2505.
23. Molecular Diagnostics tor the Clinical Laboratorian. Totowa, NJ: Humana Press; 1997.
Susan H. Bernacki, PhD; Daniel H. Farkas, PhD; Wenmei Shi, PhD; Vivian Chan, BS; Yenbou Liu, MS; Jeanne C. Beck, PhD; Karen Snow Bailey, PhD; Victoria M. Pratt, PhD; Kristin C. Monaghan, PhD; Karla J. Matteson, PhD; Frederick V. Schaefer, PhD; Michael Friez, PhD; Antony E. Shrimpton, PhD; Timothy T. Stenzel, MD, PhD
Accepted tor publication July 29, 2003.
From the Department of Pathology, Duke University Medical Center, Durham, NC (Drs Bernacki and Stenzel); Motorola Life Sciences, Pasadena, Calif (Drs Farkas and Shi, Ms Chan, and Mr Liu); Coriell Institute for Medical Research, Camden, NJ (Dr Beck); the Department of Laboratory Medicine, Mayo Clinic, Rochester, Minn (Dr Snow Bailey); Laboratory Corporation of America, Research Triangle Park, NC (Dr Pratt); the Department of Medical Genetics, Henry Ford Hospital, Detroit, Mich (Dr Monaghan); the Departments of Medical Genetics and Pathology, University of Tennessee Medical Center, Knoxville (Dr Matteson); Chapman Institute of Medical Genetics, Tulsa, Okla (Dr Schaefer); Greenwood Genetic Center, Greenwood, SC (Dr Friez); and the Department of Clinical Pathology, SUNY Upstate Medical University, Syracuse, NY (Dr Shrimpton). Dr Farkas is now with the Department of Pathology, Baylor College of Medicine, Houston, Tex; Ms Chan is now with the Molecular Pathology Department, Stanford Hospital and Clinics, Stanford, Calif; Dr Snow Bailey is now with the Department of Diagnostic Genetics, Auckland Hospital, Auckland, New Zealand; Dr Pratt is now with Nichols Institute, Quest Diagnostics, Chantilly, Va; Dr Stenzel is now with Vysis, Inc, an Abbott Laboratories Company, Downers Grove, Ill; and Motorola Life Sciences is now Clinical MicroSensors, a Motorola Company.
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US government.
Reprints: Timothy T. Stenzel, MD, PhD, Vysis, Inc, 3100 Woodcreek Dr, Downers Grove, IL 60515-5400 (e-mail: timothy.stenzel@vysis. com).
Copyright College of American Pathologists Dec 2003
Provided by ProQuest Information and Learning Company. All rights Reserved