Hydatid disease is a parasitic infection of humans and herbivorous animals caused by Echinococcus granulosus. A 20-year-old male soldier from Booshehr province police center was admitted with left upper quadrant pain that began 1 year before admission. Sonography disclosed an echogenic mass measuring 14 × 16 cm near the spleen and kidneys; a computed tomography scan confirmed it as a hypodense mass of the spleen that was 16 × 17 × 18 cm in dimension. Casoni skin test and indirect fluorescent antibody were positive. Through laparatomy, a splenectomy was successfully performed.
Introduction
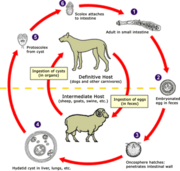
The genus Echinococcus contains three species for which humans are accidental intermediate hosts. After ingestion by a suitable intermediate host, the eggs hatch and oncospheres penetrate the intestinal mucosa and enter the circulation. They lodge primarily in the liver, but they can lodge in other organs and tissues as well, where they begin to grow, which slowly develops into a cavity lined with germinal epithelium, outside of which develops a laminated acellular area of dullness and resonance in percussion. It may be demonstrated with pelvic cysts. Slow leakage of hydatid fluid from the cyst sensitizes the patient and elicits eosinophilia.1,2
The prevalence of the hydatid cyst in different studies is low, and splenic ones constitute a small fraction of them (4%, 5/8%, 20%, and 3% of all abdominal hydatid cysts).
Case Reports
A 20-year-old man was admitted with local pain in the left upper quadrant of his abdomen that had developed slowly since 1 year before admission. He resided in rural areas of Karaj, a city in Tehran, and had close contact with cattle and dogs. The patient had been employed in a police center in Booshehr, a city in the southwest province of Booshehr, for 1 year before admission.
During the physical examination, there was a painful mass 15 cm below the left side of the costal margin. Sonography revealed an echogenic mass with an echofree area measuring 14 × 16 cm with a limiting membrane. The sonographer reported this mass as a big cystic lesion.
An abdominal computed tomography scan was performed and showed a hypodense, cystic mass 16 × 17 × 18 cm in dimension in the spleen (Fig. 1). Sonographic and radiographic studies did not show any other cysts in the liver or lungs.
Casoni skin test and indirect fluorescent antibody were positive. [In Casoni's intradermal test, hydatid fluid is injected into the skin; immediate or delayed production of wheal-and-flare reaction denotes hydatid infection. Because of its nonspecificity, this test is now rarely used (Borland's Medical Dictionary).] The patient was not vaccinated against encapsulated organisms before splenectomy.
Under general anesthesia and through laparatomy with left paramedian incision, splenectomy was performed successfully. The pathology report included spleen tissue that measured 23 × 20 × 12 cm with cystic consistency and fibrotic subcapsular regions.3,4 Two perforated and transparent cysts with 15 and 4 cm in diameters were identified on pathologic analysis. The cysts were perforated intraoperatively.
Discussion
As the cyst develops, brood capsules bud off from the germinal epithelium; these are lined with germinal epithelium from which develop protoscolices. The protoscolex of hydatid cyst resembles the scolex of an adult worm and will2,5,6 develop into a worm if the hydatid is consumed by its definitive host.
The unilocular cyst evokes an inflammatory reaction in the surrounding tissues that produces an encapsulating fibrous adventitia. Dysfunction of the organ by the common unilocular cyst is chiefly due to pressure. The neighboring tissue cells, depending upon the density of the tissues, undergo atrophy and pressure necrosis as the cyst increases in size. In the abdomen, the cysts give rise to increasing discomfort, but symptoms do not appear until the cysts have obtained a considerable size.
A remarkable feature is the extensive involvement of the organs and the long-term existence of the cyst before symptoms may be detected.2 The rupture of a cyst sets free protoscolices, bits of germinal membrane, brood capsules, and daughter cysts that may reach other tissues through blood or by direct extension and develop into secondary cysts.1,2
Hydatid cyst rupture may occur from coughing, muscle strain, blows, aspiration, and operative procedures. After cyst rupture, signs of secondary echinococcosis may not appear up to 8 years. The mortality rate is higher in secondary or infected cysts than in primary uncomplicated ones. Rupture may be accompanied by an irregular fever, gastrointestinal disturbances, abdominal pain, cyanosis, syncope, and delirium. If considerable hydatid material suddenly enters the circulation, serious anaphylactic symptoms or even sudden death may result.
The percent distribution of cysts in humans is approximately as follows: liver including secondary peritoneal invasion, 66%; lung, 22%; kidneys, 3%; bones, 2%; brain, 1%; and other tissues such as muscles, spleen, eye, heart, thyroid, 6% (Fig. 2).
A splenic cyst may cause dull pain and bulging of the ribs although spotty below the spleen that was extended near the umbilical area in abdominal cavity (Fig. 3).
According to an annual report by Iran's Ministry of Health, the incidence rate of hydatidosis from 1994 to 1999 has been 0.52, 0.93, 0.96, 0.96, 0.79, and 0.67 in 100,000 people, respectively.7 Total number of hydatid cysts in 1999 was 435, among which Khorasan, Isfahan, and Pars had the highest rates: 106, 51, and 36 in 100,000 people, respectively. Liver involvement was the most prevalent, counting for nearly 80% of all hydatid cysts. Approximately 20% of cysts were taken out from the lung, and only less than 2% were confirmed to have primary splenic origin.7 It is interesting to note that according to the aforementioned report, both the hometown (Karaj) and workplace (Booshehr) of our patient is within the same incidental zone, which is 0.11 to 0.62 in 100,000 people.
Safioleas et al.8 reported that in their studies splenic echinococcosis represents 5.8% of all abdominal hydatid cysts; 14 patients were operated on for splenic hydatid cysts in the Athens University Medical Schools during a 22-year period. Prousalidis et al.9 reported that among 49 patients suffering from hydatid cysts between 1967 and 1994, 10 had parasitic cysts in the spleen. Gollackner et al.10 operated on a series of 74 patients for abdominal cysts between June 1949 and December 1995; in 69 cases, only liver was affected and 3 patients had cysts in their spleen. Khoury et al,11 reported only 4 splenic cysts among 108 hydatid cysts in 83 patients who were approached laparoscopically in American University of Beirut Medical Center. Elfortiaet al.12 reported on a Libyan woman who had developed perihilar splenic varices without other signs of portal hypertension.
So according to the different reports and data from many countries, splenic hydatidosis is a rare condition in abdominal hydatid cysts that causes spleen involvement and leads to splenectomy. The condition in the police force is not much different from other reports because this case is one of the two cases encountered during the last 15 years. It is worth noting that both were operated in Vali-e-Asr hospital.
Conclusion
Splenic involvement is rare in patients with hydatid disease even in endemic countries.13,14 Because hydatidosis is a serious and potentially fatal disease, preventive measures should be directed toward reducing infection with the adult parasite in dogs and with larvae in sheep and dogs. The public should be informed about the route of transmission, warned about the danger of intimate contact with dogs, and instructed in personal cleanliness.
References
1. Brown HW, Neva FA: Basic Clinical Parasitology, Ed 5, pp 191-8. Appleton-Century Crofts, 1983,
2. Markell EK, Voge M, John DT: Medical Parasitology, Ed 7, pp 244-54. Philadelphia, W.B. Saunders Company, 1992.
3. Saidi F: Treatment of echinococcal cysts. In Mastery of Surgery, Ed 2, pp 818-37. Edited by Nyhus LM, Baker RJ, Sadisten DC. London, Little, Brown, and Company, 1992.
4. Kune CA, Morris DL: Hydatid disease. In Maingost' s Abdominal Operations, Ed 9, pp 1225-40. Edited by Schwarte SI, Ellis H. Appleton and Lange, 1990.
5. Itzchak Y, et al: Role of ultrasound in the diagnosis of abdominal hydatid disease. J Clin Ultrasound 1980; 8: 341-5.
6. Al-Mohaya S, Al-Awami M, Vaidya MP, Knox-Macaulay H: Hydatid cyst of the spleen. Am J Trop Med Hyg 1986; 35: 995-9.
7. Annual Report. Iran, Communicable Disease Control Department of Ministry of Health and Medical Education, 1999.
8. Safioleas M, Misiakos E, Manti C: Surgical treatmwnt for splenic hydatidosis. World J Surg 1997; 21: 324-8.
9. Prousalidis J, Tzardlnoglou K, Sgouradis L, Katsohis C, Aletras H: Uncommon sites of hydatid. World J Surg 1998; 22: 17-22.
10. Gollackner B, et al: Radical surgical therapy of abdominal cystic hydatid disease: factors of recurrence. World J Surg 2000; 24: 717-21.
11. Khoury G, et al: Laparoscopic treatment of hydatid cysts of the liver and spleen. Surg Endosc 2000; 14: 234-5.
12. Elfortia M, et al: Segmentai portal hypertension due to a splenic echino cyst. Eur J Ultrasound 2000; 11: 21-3.
13. Ballaux KE, Himpens JM, Leman G, van Den Bossche MR: Hand-laparoscopic splenectomy for hydatid cyst. Surg Endosc 1997; 11: 942-3.
14. Vahedian-Ardakani J: Hydatid cyst of liver presenting as cutaneous abscesses. Annl Sudi Med 1997; 17: 235-6.
Guarantor: Mohammad R. Jahani, PhD
Contributors: Mohammad R. Jahani, PhD*; Ghasem Roohollahi, MD[dagger]; Mohammad J. Gharavi, PhD[double dagger]
*Head Health Office of Islamic Republic of Iran Police Force, Edward Brown Alley, Tehran, Iran.
[dagger]Vali-e-Asr Hospital, Health Division of Police Force of Islamic Republic of Iran, Tehran, Iran.
[double dagger]Department of Parasitology, Iran Medical Science University, Tehran, Iran. This manuscript was received for review in December 2002. The revised manuscript was accepted for publication in March 2003.
Reprint & Copyright © by Association of Military Surgeons of U.S., 2004.
Copyright Association of Military Surgeons of the United States Jan 2004
Provided by ProQuest Information and Learning Company. All rights Reserved