Study objective: This study was designed to evaluate the peripheral muscle metabolic and structural characteristics in patients with advanced Chagas disease (ChD), and whether they were related with exercise performance.
Design: Cross-sectional study.
Setting: Out-patient cardiomyopathy clinic of a university hospital.
Patients and methods: We studied 11 stage II patients, 8 stage III patients, and 11 healthy volunteers. All patients underwent exercise testing and peripheral muscle biopsies. The muscles were also studied in control subjects. Muscle biopsy specimens were analyzed for histochemical characteristics. In six patients, the muscle was studied ultrastructurally.
Results: The data demonstrate more glycolytic and less oxidative capacity of the peripheral muscle in patients with advanced ChD (increased proportion of type IIb fibers, increased proportion of fibers with low nicotinamide adenine dinucleotide diaphorase activity, high proportion of darkly stained fibers for [alpha]-glycerophosphate dehydrogenase activity, and lower levels of citrate synthase). Many capillaries in patients with ChD had an abnormal aspect: they were either closed or showed a thicker wall. The ultrastructural study also showed fiber atrophy and abnormal capillaries even in patients with normal functional capacity. Some muscle characteristics (enzyme activity, mean cross-sectional area of the fiber, and capillarity) related with exercise parameters (anaerobic threshold, and peak oxygen pulse).
Conclusions: These findings indicate that patients with advanced ChD have decreased oxidative capacity and a shift to anaerobic metabolism in the skeletal muscle. They also suggest that muscular abnormalities are related to oxygen delivery, which is probably reduced in part by the abnormal muscle microvasculature. Those changes could affect oxygen extraction, and therefore exercise tolerance in these patients. (CHEST 2004; 125:1306-1314)
Key words: cardiomyopathy; Chagas disease: exercise test; pulmonary gas exchange; skeletal muscle
Abbreviations: [alpha]-GPD=[alpha]-glycerophosphate dehydrogenase; ChD=Chagas disease; CHF=congestive heart failure; CS=citrate synthase; CSA=cross-sectional area; HAD=[beta]-hydroxy-acyl-coenzyme A-dehydrogenase; HRR=heart rate reserve; LDH=lactate dehydrogenase; MVV=maximal voluntary ventilation; NAHD-d=nicotinamide adenine dinucleotide diaphorase; [O.sub.2]-Pulse=oxygen pulse; VE=minute ventilation; V[O.sub.2]=oxygen uptake
**********
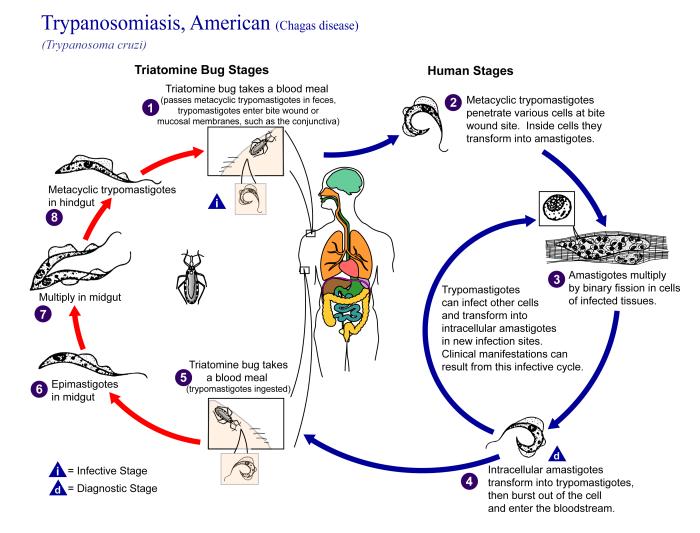
Chagas disease (ChD) is endemic from south of Rio Grande to the Patagonia, effecting around 18 million people. The migration of infected Latin Americans to the United States or to other first-world countries (Canada or Europe), where the disease is uncommon poses two problems: the misdiagnosis or underdiagnosis of ChD in these immigrants, and the possibility of transmission through blood transfusions. (1,2) A recent report of Trypanosoma cruzi in Los Angeles and Miami blood donors indicate that evaluation of transfusion as a mode of T cruzi transmission in the United States is needed. (3) Alterations in heart, skeletal, and smooth muscles develop 10 to 20 years after the infection with the etiologic agent T cruzi. (4)
Several classifications have been used for stratifying patients with ChD. (5,6) Even though congestive heart failure (CHF) is one of the most severe manifestations of chronic Chagasic cardiomyopathy, the majority of the classifications are based on clinical, ECG, and echocardiography features. (5,6) None of them uses the exercise capacity measured directly instead of subjective parameters of the New York Heart Association functional class. One limitation of these systems is that a patient could be stratified in the severe stage because of abnormal ECG findings or ventricular arrhythmia, irrespectively of the functional capacity. This could be limiting, because it is well known that peak exercise oxygen uptake (V[O.sub.2]) in patients with ChD, and CHF of other etiologies has an important prognostic value. (7,8)
Few reports (8-11) have evaluated exercise capacity and the factors affecting exercise tolerance in patients with ChD. However, there are contradictory data on whether ChD affects exercise performance, and the factors determining exercise limitation in these patients are poorly understood.
It is possible that in addition to cardiac impairment, other factors such as peripheral muscle abnormalities may contribute in affecting the functional capacity of these patients. During the last years, several studies (12-26) have shown that skeletal muscle function and structure are altered in patients with chronic cardiopulmonary disease. Few descriptive studies, (27-30) mainly in animals, have reported the presence of skeletal muscle damage in patients with ChD probably associated with neurologic processes.
However, to our knowledge no information is available regarding the peripheral muscle metabolic and histochemical characteristics in patients with advanced ChD, and their relationship with exercise performance. The aims of the present study were as follows: to study the histochemical characteristic of the skeletal muscle in patients with advanced ChD (stage II and stage III), and determine if the abnormalities could be caused by the disease; secondly, to assess the functional capacity of the patients, and evaluate whether the functional measurements relate with the muscle characteristics.
MATERIALS AND METHODS
Patients
The study group consisted of 10 male and 9 female patients recruited from the cardiomyopathy clinic of the Hospital Universitario de Caracas. The committees of human research approved the study, and all the subjects signed the informed consent.
For the purpose of this study, the diagnosis of ChD and the definition of severity were made according to the classification of Puigbo et al. (5) Patients were enrolled if they met the following criteria: (1) serologic and clinical evidence for chronic ChD in stage II and stage III of the disease (stage II is characterized by ECG abnormalities and altered heart segmental motility without CHF; stage III is characterized not only by ventricular dilatation, abnormal ECG findings, and autonomic dysfunction, but also by CHF and/or marked arrhythmia); (2) stable condition, defined as no acute exacerbation of cardiac disease for 6 weeks prior to entry into the study; and (3) the ability to walk on a treadmill.
To establish the presence of exclusion criteria, all the patients underwent medical history, physical examination, and diagnostic studies (ECG, standard chest radiography, resting pulmonary function testing, resting Doppler echocardiography, pertinent laboratory, tests). Patients with any of the following criteria were excluded: (1) cardiovascular disease other than ChD; (2) patients with any pleural or pulmonary disease; (3) neuromuscular disease of any type or other condition that affects the capacity to perform exercise; and (4) diabetes mellitus and other metabolic diseases.
Based on the classification of Puigbo et al, (5) there were 11 patients in stage II and 8 patients in stage III. All patients were in stable condition receiving vasodilator (enalapril), antiarrhythmic (amiodarone), or inotropic drugs (digoxin) at regular doses.
Medical history, physical examination, ECG, standard chest radiography, resting pulmonary function testing, pertinent laboratory tests, and skeletal muscle characteristics were also per formed in 11 age-matched, healthy volunteers to compare with patients with ChD.
Echocardiography
Resting, color Doppler transthoracic echocardiography (Sonos 1000; Hewlett-Packard; Andover, MA) with a 2.5-MHz probe was performed in all patients with ChD. Parasternal long-axis, parasternal short-axis, four-chamber, and subcostal views were recorded. Left ventricular ejection fraction, interventricular septal, left ventricular posterior wall thickness, left atrial diameter, and left ventricular end-diastolic volume were calculated.
Pulmonary Function Testing
FVC was performed using a dry seal spirometer (CardiO2 System; MedGraphics; St. Paul, MN). FVC, FE[V.sub.1], and FVC/ FE[V.sub.1] radio were calculated according to the recommendations of the American Thoracic Society. (31) Normal values for pulmonary measurements were taken from standard reference sources. (32) Maximal voluntary ventilation (M\W) was directly determined over a 12-s period.
Incremental Exercise Testing
The exercise test was performed on a treadmill (CardiO2 System; MedGraphics) using an incremental ramp protocol. Patients were started with a 2-min resting period, followed by a 3-min warm-up (0[degrees] inclination, and speed of 1.3 miles per hour), and finally the incremental ramp (inclination of 1[degrees] per minute, and constant speed of 3.3 miles per hour). The patients were strongly encouraged to walk until discomfort or exhaustion was reported (symptom-limited exercise test) or an abnormal ECG finding noted. Heart rate and rhythm were monitored with a 12-lead ECG, and BP was measured with the cuff technique every minute.
Minute ventilation (VE) and its components were measured using a pneumotachograph. The concentrations of expired oxygen and carbon dioxide were analyzed (breath-by-breath system) with a zirconium dioxide cell oxygen analyzer and an infrared carbon dioxide analyzer, respectively. These measures and flow signals were electronically integrated by a computerized system to yield 30-s averages of VE, V[O.sub.2], carbon dioxide output, and gas exchange ratio. Heart rate reserve (HRR) was determined from the maximal heart rate obtained and maximal predicted heart rate (220--age). Predicted maximal V[O.sub.2] was calculated according to Jones and Campbell. (33) Arterial hemoglobin oxygen saturation was monitored noninvasively with a pulse oximeter.
Skeletal Muscle Study
All patients and control subjects underwent muscle biopsies. Muscle samples of approximately 25 mg were taken from the vastus lateralis part of the quadriceps femoris muscle, with the Bergstrom needle. (34) Briefly, after local anesthesia with 2 mL of lidocaine 2%, a 5-mm skin incision was performed and muscle samples were obtained.
The samples were divided in three parts. One was embedded with optimal cutting temperature compound (Tissue Tek II: Sakura Finetek; Torrance, CA) and frozen in isopentane cooled with liquid nitrogen. Transverse 10-[micro]m serial sections were cut in a cryostat at -20[degrees]C and mounted on cover slips for staining for adenosine triphosphatase after alkaline (pH 10.3) and acid (pH 4.37 and 4.6) preincubation. (35) Sections were also stained for reduced nicotinamide adenine dinucleotide diaphorase (NAHD-d), (36) and [alpha]-glycerophosphate dehydrogenase ([alpha]-GPD). (37) The fibers were classified its high, medium, or low oxidative/glycolytic capacity according to the intensity of the staining evaluated by two different observers. Capillaries were visualized by the [alpha]-amylase-period acid Schiff reaction. (38) Photomicrographs at a final magnification of 200 x were taken from these sections, and the fibers were identified by comparison with the adenosine triphosphatase sections. An area of the photograph was delimited, measured with a planimeter, and fibers and capillaries were counted to calculate the mean area of the fibers, capillaries per millimeter squared, and capillaries/fiber ratio. Also, capillaries around each fiber type were counted, and the mean was expressed as capillary contacts. All the fibers of one type were drawn together, and the area was measured by planimetry to calculate the mean area of each fiber type. The relationship between capillary contacts and each fiber-type cross-sectional area was calculated.
The second part of the muscle sample was homogenized in ice-cooled potassium phosphate buffer. The activities of citrate synthase (CS), [beta]-hydroxy-acyl-coenzyme A-dehydrogenase (HAD), and lactate dehydrogenase (LDH) were assayed using fluorometric techniques. (39) Results are expressed in micromols per min per gram of wet weight.
The third part of the muscle sample was fixed in 3% glutaraldehyde in phosphate buffer, at pH 7.4 and 320 milliosmol, postfixed in 1% Os[O.sub.4], and embedded in epon; sections were cut with a diamond knife in a Porter-Blum MT2 ultramicrotome (Sovvall; Dupont Instruments; Newtown, CT), stained with uranyl acetate and lead citrate, and observed in a Hitachi H-500 transmission electron microscope (Hitachi; Tokyo, Japan), at an acceleration voltage of 100 kilovolts.
Statistical Analysis
Data are presented its mean [+ or -] SD. The differences in skeletal muscle and physical characteristics between patients and control subjects were determined using Mann-Whitney U test. Spearman rank correlation (R) was used to assess the relationship between skeletal muscle characteristics with echocardiography data, and exercise parameters. The acceptable level of statistical significance for each test was p < 0.05.
RESULTS
Pulmonary Function and Exercise Performance Response
Age (ChD, 55 [+ or -] 9 years, vs control, 52 [+ or -] 9 years), height (ChD, 164 [+ or -] 12 cm, vs control, 162 [+ or -] 10 cm), and weight (ChD, 68 [+ or -] 13 kg, vs control, 68 [+ or -] 13 kg) were similar between the groups. As expected, resting pulmonary function measures were similar between patients with ChD and control subjects.
Peak values achieved during the exercise test are shown in Table 1. Patients had a wide range of exercise capacity and functional class. According to the criteria of Weber and Janicki, (40) 58% of the patients had mild-to-no functional impairment (V[O.sub.2] > 20 mL/kg/min), 26% had mild-to-moderate impairment (V[O.sub.2] 16 to 20 mL/kg/min), 5% had moderate-to-severe impairment (V[O.sub.2] 10 to 16 mL/kg/ min), 11% had severe impairment (V[O.sub.2] 6 to 10 mL/kg/min), and none had very severe functional impairment (V[O.sub.2] < 6 mL/kg/min). All the patients as a group have reduced HRR and abnormal oxygen delivery indexes (oxygen pulse [[O.sub.2]-Pulse] and [DELTA]heart rate/[DELTA]V[O.sub.2]). The breathing reserve (maximal VE/MVV), and gas exchange measures (physiologic dead space ventilation, arterial-end tidal carbon dioxide pressure difference, and alveolar-arterial oxygen pressure difference) were in the normal range.
Echocardiography Data
As shown in Table 2, the global systolic left ventricular function was normal with a wide range. Left atrial diameter, mean interventricular septal, and left ventricular posterior wall thickness were within normal values. The study group showed mild left ventricular dilation. As previously noted, there was a wide range distribution in all measured parameters.
Skeletal Muscle Data
Fiber-type distribution in patients aim control subjects is shown in Figure 1. The proportion of IIb fiber was increased in patients with ChD compared to the normal group. No differences were observed in the proportion of type I and IIa fibers between the groups. The percentage of fibers with low oxidative capacity was increased in patients with ChD and also the percentage of fibers with high glycolytic capacity at the expense of a reduction in the percentage of medium, and low glycolytic capacity fibers (Fig. 2). These changes indicate more glycolytic and less oxidative activity of the muscle fibers. Mean cross-sectional area (CSA) of the fibers, CSA of the different fiber types, capillarity measured as capillaries per millimeter squared, capillaries per fiber, and the number of capillary contacts with the different fiber types data are shown in Table 3. Mean CSA of all the fibers, and CSA of type IIa fibers were similar in both groups; however, significant atrophy of types I and IIb fibers was observed in patients with ChD. Capillary contacts to type IIa fibers were higher in control subjects than in patients with ChD, but were similar in type I and type IIb fibers. Although the capillary to fiber ratio showed a trend to be lower in patients with ChD (p = 0.08), the capillary density was higher (p < 0.05). Capillary contacts per type I fiber CSA was also higher in the patients with ChD (Table 3). However, many capillaries in patients with ChD had an abnormal aspect: they were either closed or showed a thick wall (Fig 3).
[FIGURES 1-3 OMITTED]
In six patients in whom muscle was studied ultra-structurally, fiber atrophy was also seen, manifested as parts of the fiber devoid of myofilaments and by the folding of the sarcolemma. Capillaries were abnormal, with thickened basement membrane, proliferative endothelium showing Golgi apparatus, rough sarcoplasmic reticulum, bizarre mitochondria, and some large vacuoles. Some capillaries were also occluded or showed infoldings into the lumen. Figure 4, bottom, B illustrates the ultrastructural abnormalities found in the muscle sample of a patient with ChD and normal functional capacity (maximal V[O.sub.2] > 20 mL/kg/min), compared to a normal subject (Fig 4, top, A).
[FIGURE 4 OMITTED]
Figure 5 shows the enzyme activities in patients with ChD and the control group. CS and LDH levels were decreased in patients with ChD. Similar values were observed in the HAD activity between the groups.
[FIGURE 5 OMITTED]
Correlation Between Exercise and Echocardiography Data With Skeletal Muscle Characteristics in Patients With ChD
Table 4 shows the significant correlation found between exercise data and skeletal muscle characteristics. Significant direct correlations were found between the enzyme CS, HAD, and LDH activities with the anaerobic threshold (V[O.sub.2] liters per minute). Peak [O.sub.2]-Pulse was directly related to capillary/fiber ratio, capillary contacts to type I fiber and CSA of the fiber. No correlations were found between left ventricular ejection fraction and skeletal muscle parameters.
DISCUSSION
There were three important findings in this study of patients with advanced ChD. First, skeletal muscle abnormalities in patients with advanced ChD are characterized by more glycolytic and less oxidative activity. Second, patients with advanced ChD have a wide range of exercise capacity. Third, significant correlations were found between skeletal muscle characteristics (enzyme activity, CSA of the fiber, and capillarity) and oxygen delivery index (anaerobic threshold, and peak [O.sub.2]-Pulse) during exercise. According to these results, exercise performance, and oxygen delivery during exercise in advanced ChD appears to be markedly related with peripheral limitation and skeletal muscle abnormalities.
Several studies (19-26) have shown that skeletal muscle function and structure are altered in patients with different heart diseases, and CHF. Some of these studies (20, 22-24, 26) have compared the muscle characteristic in these patients with normal subjects, and indicate that skeletal muscle changes may play a role in the limitation of exercise capacity. A decrease in the proportion of type I fibers and a corresponding increase in type II fibers (mainly type IIb) compared to normal subjects have been generally reported in patients with CHF. (21,25) In contrast, very contradicting results have been obtained with respect to capillarity in these patients. (20-22,25,26) However, there is an overall tendency for a reduced capillary/fiber ratio, but depending on the degree of atrophy the capillary density may even be increased. The analysis of enzyme activities also suggests an increase of glycolytic activity and decrease oxidative capacity in the skeletal muscle of patients with CHF. (23,24,26)
Only a few old descriptive studies (27-30) in animals and humans have reported the presence of skeletal muscle damage in ChD that suggest denervation. To our knowledge, no previous study has assessed fiber type proportion, capillarity, or enzyme activity in skeletal muscle of patients with ChD in any stage.
The present study, in contrast with the other studies, (27-30) includes the histochemical and morphologic characteristics of the skeletal muscle and their relationship with exercise parameters in patients with ChD. Our findings in patients with ChD agree with those reported in COPD and CHF, (12-14,17,21,25) since we also found an increased proportion of type IIb fibers, and the presence of atrophy in fibers I and IIb. We also observed in the patients with ChD lower levels of CS, accompanied by an increased proportion of fibers with low NADH-d activity and a high proportion of darkly stained fibers for [alpha]-CPD activity. These results indicate a decrease in the oxidative capacity and a shift to anaerobic metabolism as reported in patients with CHF. The reduction of the level of LDH in patients with ChD is an unexpected finding. It is possible that atrophic IIb fibers produce lower enzyme levels, or that there is a metabolic adaptation of the enzymes to the anaerobic mechanism, as suggested by the direct correlation between the anaerobic threshold and the LDH level. Another possibility is a change in the isoenzyme proportion that could be analyzed in future studies.
Several capillary parameters were similar between patients with ChD and control subjects, but the capillary density and the capillary contact/CSA in type I fiber were higher in patients with ChD. However, many capillaries in these patients had an abnormal aspect: they were either closed or showed a thick wall, findings that were also observed at the ultrastructural study. In patients with CHF, it has been reported a reduction in the number of endothelial cells/fiber and a negative correlation between this parameter with exercise capacity. (20) Some authors suggested that these findings might be due to a compensatory maladaptive angiogenic response to exercise intolerance. This argument could he expanded to patients with ChD, but in addition it is possible that vasodilator treatment (like the drugs used by some of the patients included in the study) may also play a role in these changes, because vasodilator drugs have shown to produce an increase in capillary density in the heart as well as in the skeletal muscle. (19) In an experimental study, rat muscle fibers and capillaries were affected by treatment with nitroglycerin, nifedipine, diltiazem, or propranolol. (41)
In patients with CHF, several studies (19-25) have shown that disuse, hypoxia, medication, or malnutrition can lead to skeletal muscle alterations. Additionally, in CHF the compromise of muscle perfusion could also play an important role. In the present study, no correlation was found between left ventricular ejection fraction and any other parameters. Therefore, the decreased blood flow or oxygen delivery to the skeletal muscle cannot be entirely attributed to a central component (cardiac impairment), and alteration in the peripheral circulation or in oxygen extraction could explain in part these changes. The capillary abnormalities could also affect the oxygen diffusion to the muscle fibers, and determine the shift to anaerobic metabolism, and reduced exercise performance. It is well known that the oxygen diffusion from the red cell to the sarcoplasm mainly depends of the capillary. P[O.sub.2] that provide the pressure gradient necessary for oxygen to diffuse. The major factors determining the P[O.sub.2] gradient between red cell and sarcoplasm are the resistances to oxygen diffusion by the red cell membrane, plasma, capillary endothelium, interstitial space, and sarcolemma. (42) It is possible to assume that the presence of capillary abnormalities will affect the capillary P[O.sub.2] gradient and the oxygen diffusion. Although disuse effect cannot be completely ruled out in these patients as a cause of the observed muscle abnormalities, the fact that we found patients with normal functional capacity and muscle or capillary changes suggests a direct effect of the disease. Figure 4 illustrates the ultrastructural abnormalities found in the muscle samples of a patient with ChD and normal functional capacity (maximal V[O.sub.2] of 28 mL/kg/min).
In the chronic phase of ChD, usually no parasites are present at the site of lesions. Autoimmunity has been claimed to be a pathogenic mechanism in the production of lesions in heart and muscle. In mice infected with different strains of T cruzi, half of skeletal muscle cells isolated from rectus femoris expressed Ia antigens on their surface after 30 days after infection. (43) It is possible that capillary abnormalities and part of the found muscle alterations may be a consequence of autoimmune processes.
Several studies (8-11) have evaluated exercise performance in patients with ChD at different evolution stages. Most of them have reported a wide range of exercise capacity in these patients, in particular in the advanced stages (II and III). Mady et al (10) studied 104 patients with ChD with different functional class. Their results indicate that 35.6% of the patients reached a peak V[O.sub.2] > 20 mL/kg/min (range, 20.5 to 30 mL/kg/min). However, Oliveira et al (11) assessed the exercise capacity in 52 patients with ChD at different stages (17 patients at stage IA, 9 patients at stage IB, 14 patients at stage II, and 12 patients at stage III). They observed in all the groups that 34% of the patients reached a peak V[O.sub.2] between 10 mL/kg/min and 20 mL/kg/min, and 52% reached values > 20 mL/kg/min. In addition, they reported that 50% of the stage III patients reached a peak V[O.sub.2] > 20 mL/kg/min.
In the present study, most of the patients (58%) showed a peak V[O.sub.2] > 20 mL/kg/min, and only 16% were < 16 mL/kg/min. Our findings are consistent with those of the previous studies, (10,11) since we also found a wide range of maximal functional capacity in patients with advanced ChD. These results suggest that the current and other classifications used for stratifying patients with ChD in advanced or severe condition cannot accurately identify an individual with severe functional limitation. With these classifications, we could have patients stratified in the advanced stages because of ventricular arrhythmia with a normal functional capacity. As previously noted, both ejection fraction and maximal exercise V[O.sub.2] have been used for stratifying patients in heart failure due to ChD (8) or other etiologies, (7) and identifying those with poor prognosis. It would be important to consider including parameters from the exercising gas exchange such as the maximal V[O.sub.2] per kilogram in the stratification of patients with ChD in order to increase its accuracy and prognostic value. The heterogeneity of the disease, which is reflected in the stage classification, limits the interpretation of the results and has moved us to propone a new classification of the disease excluding the ventricular arrhythmia as a factor used to include a patient in advanced stages.
In summary, the present study shows that patients with ChD have a wide range of exercise capacity, from normal to severe functional impairment. The analysis of the skeletal muscle in these patients showed an increase of type IIb fibers proportion, although in 57% of the patients these fibers and type I fibers were atrophied. In addition, many capillaries were altered, and the levels of CS and LDH were decreased. The ultrastructural study also showed fiber atrophy and abnormal capillaries even in patients with normal functional capacity. There was a direct relationship between enzyme activities with the anaerobic threshold, and between oxygen delivery with capillarity and CSA of the fibers. These findings suggest that skeletal muscle abnormalities in patients with ChD could be related with the oxygen delivery, which is probably affected in part by the alterations of the muscular microvasculature, although disuse effects cannot be completely ruled out. Those changes could affect the skeletal muscle oxygen extraction, and therefore the exercise tolerance in these patients.
ACKNOWLEDGMENT: The authors thank Hector J. Finol, PhD, for skeletal muscle ultrastructural analysis.
REFERENCES
(1) Rassi A Jr, Rassi A, Little WC. Chagas' heart disease. Clin Cardiol 2000; 23:883 889
(2) Hagar JM, Rahimtoola SH. Chagas' heart disease in the United States. N Engl J Med 1991; 325:763-768
(3) Leiby DA, Herron RM, Read EJ, et al. Trypanosoma cruzi in Los Angeles and Miami blood donors: impact of evolving donor demographics on seroprevalence and implications for transfusion transmission. Transfusion 2092; 42:549-555
(4) World Health Organization. Sixth Program report, Chagas' disease: special program for research and training in tropical diseases. Geneva, Switzerland: UNDP, World Bank, WHO, 1983
(5) Puigbo JJ, Gordian H, Suarez C, et al. Clinical aspects in Chagas' disease. In: Madoery RJ, Madoery C, Camera MI, eds. Actualizaciones en la enfermedad de Chagas. Buenos Aires, Argentia: Organismo Oficial del Congreso Nacional de Medicina, 1992; 27-38
(6) Hagar JM, Rahimtoola SH, Chagas' heart disease. Curr Probl Cardiol 1995; 20:825-924
(7) Stelken AM, Younis LT, Jennison SH, et al. Prognostic value of cardiopulmonary exercise testing using percent achieved of predicted oxygen uptake for patients with ischemic and dilated cardiomyopathy. J Am Coll Cardiol 1996; 27:345-352
(8) Mady C, Cardosa RH, Barretto AC, et al. Survived and predictors of survival in patients with congestive heart failure due to Chagas' cardiomyopathy. Circulation 1994; 90:3098-3102
(9) Mady C, Ianni BM, Arteaga E, et al. Maximal functional capacity, and diastolic function in patients with cardiomyopathy due to Chagas' disease without congestive heart failure. J Card Fail 2000; 6:220-224
(10) Mady C, Cardosa RH, Ianni BM, et al. Normal maximal functional capacity in patients with congestive heart failure due to Chagas' cardiomyopathy [in Portugese]. Arq Bras Cardiol 1996; 67:1-4
(11) Oliveira FP, Pedrosa RC, Giannella-Neto A. Gas exchange during exercise in different evolutional stages of chronic Chagas' heart disease. Arq Bras Cardiol 2000; 75:481-498
(12) Satta A, Migliori GB, Spanevello A, et al. Fiber types in skeletal muscles of chronic obstructive pulmonary disease patients related to respiratory function and exercise tolerance. Eur Respir J 1997; 10:2853-2860
(13) Whittom F, Jobin J, Simard PM, et al. Histochemical and morphological characteristics of the vastus lateralis muscle in COPD patients. Med Sci Sports Exerc 1998; 30:1467-1474
(14) Jobin J, Maltais F, Doyon JF, et al. Chronic obstructive pulmonary disease: capillarity and fiber-type characteristics of skeletal muscle. J Cardiopulm Rehabil 1998; 18:432-437
(15) Maltais F, Simard AA, Simard C, et al. Oxidative capacity of the skeletal muscle and lactic acid kinetics during exercise in normal subjects and in COPD. Am J Respir Crit Care Med 1996; 153:288-293
(16) Montes de Oca M, Celli BR. Peripheral muscle in COPD: deconditioning or myopathy? Arch Bronconeumol 2001; 37: 82-87
(17) Jakobsson P, Jorfeldt L, Brundin A. Skeletal muscle metabolites and fiber types in patients with advanced chronic obstructive pulmonary disease (COPD), with and without chronic respiratory failure. Eur Respir J 1990; 3:192-196
(18) Mador MJ, Bozkanat E. Skeletal muscle dysfunction in chronic obstructive pulmonary disease. Respir Res 2001; 2:216-224
(19) Torres SH, Almeida D. Rosenthal J, et al. Skeletal muscle changes with training in patients with coronary artery disease. J Cardiopulm Rehabil 1990; 10:271-278
(20) Duscha BD, Kraus WE, Keteyian SJ, et al. Capillary density of skeletal muscle: a contributing mechanism for exercise intolerance in class II-III chronic heart failure independent of other peripheral alterations. J Am Coll Cardiol 1999; 33: 1956-1963
(21) Lipkin DP, Jones DA, Round JM, el al, Abnormalities of skeletal muscle in patients with chronic heart failure. Int J Cardiol 1988; 18:187-195
(22) Drexler H, Riede U, Munzel T, et al. Alteration of skeletal muscle in chronic heart failure. Circulation 1992: 85:1751-1759
(23) Ralston MA, Merola AJ, Leier CV. Depressed aerobic enzyme activity of skeletal muscle in severe chronic heart failure. J Lab Clin Med 1991; 117:370-372
(24) Sullivan MJ, Green HJ, Cobb FR. Altered skeletal muscle metabolic response to exercise in chronic heart failure: relation to skeletal muscle aerobic enzyme activity. Circulation 1991; 84:1597-1607
(25) Sullivan MJ, Green HJ, Cobb FR. Skeletal muscle biochemistry and histology in ambulatory patients with long-term heart failure. Circulation 1990; 81:518-527
(26) Duscha BD, Annex BH, Keteyian SJ, et al. Difference in skeletal muscle between men and women with chronic heart failure. J Appl Physiol 2001; 90:280-286
(27) Laguens RP, Cossio PM, Diez C, et al. Immunopathologic and morphologic studies of skeletal muscle in Chagas' disease. Am J Pathol 1975; 89:153-162
(28) Meckert PM, Laguens RP. Selectivity of alterations in skeletal fibers in chronic Chagas' disease of the mouse. Experientia 1988; 44:14-16
(29) Taratuto A, Pagano MA, Fumo T, et al. Histological and histochemical changes of the skeletal muscle in human chronic Chagas' disease [in Portugese]. Arq Neuropsiquiatr 1978; 36:327-331
(30) Sica RE, Gonzalez SM, Cappa SM, et al. Peripheral nervous system involvement in human and experimental chronic American tripanosomiasis. Bull Soc Pathol Exot 1995; 88: 156-163
(31) American Thoracic Society. Standardization of spirometry 1987 update: ATS statement. Am Rev Respir Dis 1987; 136: 1285-1298
(32) Cherniak RM, Raber MD. Normal standards for ventilatory function using an automated wedge spirometer. Am Rev Respir Dis 1972; 106:38-46
(33) Jones NL, Campbell AJM. Clinical exercise testing. 2nd ed. Philadelphia, PA: W.B. Sanuders. 1982
(34) Bergstrom J. Muscle electrolytes in man. Scand J Clin Lab Invest 1962; 68:1-100
(35) Brooke MH, Kaiser KK. Muscle fibers types: how many and what kind? Arch Neurol 1970; 23:369-379
(36) Novikoff AB, Shin WY, Drucker J. Mitochondrial localization of oxidation enzymes: staining results with tetrazolium salts. J Biophys Biochem Cytol 1961; 9:47-61
(37) Wattemberg ML, Leong JL. Effect of coenzyme Q 10 and menadione on succinate dehydrogenase activity as measured by tetrazolium salt reduction. J Histochem Cytochem 1969; 8:296-303
(38) Andersen P. Capillary density in muscles of man. Acta Physiol Scand 1975; 95:203-205
(39) Lowry OH, Passonneau JV. A flexible system of enzyme analysis. New York, NY: Academic Press, 1972
(40) Weber KT, Janicki JS. Cardiopulmonary exercise testing for evaluation of chronic cardiac failure. Am J Cardiol 1985; 55:22A-31A
(41) Torres SH, Kaswan D. Andujar J. et al. Effect of vasoactive drugs on muscle fiber types and capillaries. Acta Cient Venez 1994; 45:199-206
(42) Wittenberg BA, Wittenberg JB. Transport of [O.sub.2] in muscle. Annu Rev Physiol 1989; 51:857-875
(43) Meckert PC, Hontebeyrie-Joskowicz M, Chambo J, et al. Trypanosome cruzi: aberrant expression of class II major histo-compatibility complex molecules in skeletal and heart muscle cells of chronically infected mice. Exp Parasitol 1991; 72:8-14
* From the Pulmonary Division (Drs. Montes de Oca and Vazquez), University Hospital of Caracas, Central University of Venezuela; Section for Muscle Adaptation (Drs. Torres, Hernandez, and Ms. Anchustegui), Institute of Experimental Medicine, Central University of Venezuela; Centro Medico de Caracas (Dr. Loyo); and Cardiomyopathy Unit (Dr. Puigbo) University Hospital of Caracas, Caracas, Venezuela.
Support was provided by Consejo Nacional de Investigaciones Cientificas y Tecnologicas (S1-97001106) Consejo de Desarrollo Cientifico y Humanistico, UCV, 09.33.4367.1999.
Manusscript received June 12, 2003: revision accepted November 5, 2003.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Maria Montes de Oca, MD. CCS 5150, PO Box 025323, Miami, FL 33102-5323; e mail: mmdeoca@cantv.net
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group