Urogenital infections caused by Chlamydia trachomatis are common and may cause female infertility and ectopic pregnancy. Such infections are treatable but as C trachomatis often causes no symptoms they may' remain undetected. As screening for C trachomatis reduces the number of complications,[1] and self reportable screening criteria seem to have a low predictive value for infection,[2] testing people not seeking medical care seems relevant. C trachomatis can be detected by amplification of DNA from urine and vaginal secretions--samples that can be obtained at home and mailed directly to the laboratory.[3 4] Usually a swab sample is taken by a doctor but if a patient can collect a sample at home this may result in improved screening rates and thus more infections being detected.
Subjects, methods, and results
We randomised all 17 high schools in Aarhus County into two screening groups. In the home sampling group the females were asked to collect two urine samples and one vaginal flush sample[3] and the males were asked to collect one first void urine sample. These samples were mailed directly from home to the microbiology department at Aarhus University Hospital. In the usual testing (control) group the students were offered testing at their doctors or at the local clinic for sexually transmitted diseases. Both groups received a questionnaire and information on C trachomatis infection. The students were asked for their identification number, from which the number of infected respondents in the control group was calculated.
Students in the home sampling group were asked to give an address for receipt of the test results or the address of their doctor. To ensure that infected students followed our advice to seek treatment they were asked to give their doctor an envelope that contained a slip to be returned.
Students who returned the questionnaire were designated responders, and sexually experienced responders were called eligible responders. The efficacy measures were the number of tested and infected students respectively.
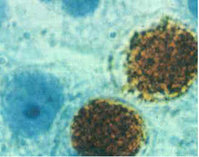
Home samples were analysed by an amplified C trachomatis test kit (TMA, Gen-Probe, San Diego, CA). Swab samples were analysed by enzyme immunoassay (Microtrak II, Behring Diagnostics, Marburg, Germany) and confirmed by DNA amplification.[5]
In the home sampling group, 1254 of 2603 (48%) females responded compared with 1097 of 2884 (38%) in the control group, and of the 1733 males in the home sampling group, 590 (34%) responded compared with 316 of 1689 (19%) in the control group (table). There was no difference in knowledge of C trachomatis infection between the two groups: mean age (females 18.0 years (SD 1.5 years), males 18.2 years (SD 1.7 years)); having a regular intimate relationship (47% of females and 36% of males); and presence of urogenital symptoms (12% of females and 3% of males).
Efficacy of home sampling for C trachomatis infection compared with usual testing by doctor taking swab (95% confidence interval shown for differences between rate)
(*) P < 0.001.
([dagger]) P<0.05.
In the home sampling group, 867 (93.4%) eligible females were tested compared with 63 (7.6%) in the control group ([chi square]= 1298, P [is less than] 0.001). The figures for detected infections were 43 (4.6%) and 5 (0.6%) respectively ([chi square]=26.9, P [is less than] 0.001). In the home sampling group, 430 (97.3%) eligible males were tested compared with 4 (1.6%) in the control group ([chi square] = 620, P [is less than] 0.001). The figures for detected infections were 11 (2.5%) and 1 (0.4%) respectively ([chi square]=4.15, P= 0.042). Statistical significance was also achieved when all students were considered the target population. The slip was returned for 95% of the infected students.
The prevalence of infection was highest in the control group, implying that students in this group were more concerned about the possibility of infection. This was shown by the higher rate of tested females with symptoms in the control group (38%) compared with the home sampling group (12%) ([chi square]=23.8, P [is less than] 0.001).
Comment
The efficacy of screening for C trachomatis is improved when patients can collect their own samples at home and mail them directly to a laboratory rather than having a swab taken by their doctor. Asking patients to provide home samples may reduce the number of complications from C trachomatis and its prevalence.
We thank Mette Jensen and Gitte Hoj for their technical assistance.
LO initiated and coordinated the formulation of the primary study hypothesis and the core ideas, designed the protocol, obtained approval from the ethics commitee and the Danish Data Protection Agency, participated in informing the students, performed data collection, analyses, interpretation, and writing of the paper; he will act as guarantor for the paper. BA discussed core ideas, participated in protocol design, information process, data collection and interpretation, and edited the paper. FO discussed core ideas, participated in protocol design, information process, and interpretation of data, and edited the paper. JKM discussed core ideas, participated in protocol design, information process, data scanning, analysis and interpretation, and edited the paper.
Funding: The study was funded by the Danish National Board of Health (grant No 210 i 1997), Lovens Kemiske Fabriks Research Foundation, Nycomed DAK, Pfizer, and Chairman Jacob Madsen and Hustru Olga Madsen's foundation.
Conflict of interest: None.
[1] Scholes D, Stergachis A, Heidrich FE, Andrilla H, Holmes KK, Stamm WE. Prevention of pelvic inflammatory disease by screening for cervical chlamydial infection. N Engl J Med 1996;334:1362-6.
[2] Ronsmans C, Bulut A, Yolsal N, Agacfidan A, Filippi V. Clinical algorithms for the screening of Chlamydia trachomatis in Turkish women. Genitourin Med 1996;72:182-6.
[3] Ostergaard L, Moller JK Andersen B, Olesen E Diagnosis of urogenital Chlamydia trachomafis infection in women based on mailed samples obtained at home: multipractice comparative study. BMJ 1996;313: 1186-9.
[4] Andersen B, Ostergaard L, Moller JK, Olesen F. Home sampling versus conventional contact tracing for detecting Chlamydia trachomatis infection in male partners of infected women: randomised study. BMJ 1998; 316:350-1.
[5] Ostergaard L, Moiler JK. Use of PCR and direct immuno-fluorescence microscopy for confirmation of results obtained by Syva MicroTrak Chlamydia enzyme immunoassay. J Clin Microbiol 1995;33:2620-3.
(Accepted 22 December 1997)
RELATED ARTICLE: Questions to doctors
(*) Life situation was defined as social situation, life problems, lasting work disability, or circumstances related to work or lack of work.
Department of Infectious Diseases, Aarhus University Hospital, PP Orumsgade 11, DK-8000 Aarhus C, Denmark
Lars Ostergaard, senior registrar
Research Unit for General Practice, University of Aarhus, DK-8000 Aarhus C, Denmark Befit Andersen, research assistant
Frede Olesen, consultant physician
Department of Clinical Microbiology, Aarhus University Hospital Jens K Moiler, director
Correspondence to: Dr Ostergaard segalt@dadlnet.dk
BMJ 1998;317:26-7
COPYRIGHT 1998 British Medical Association
COPYRIGHT 2000 Gale Group