Urogenital infections with Chlamydia trachomatis are widespread and usually asymptomatic. Major complications from infection include ectopic pregnancies and female infertility.[1] Although contact tracing reduces the prevalence of chlamydia infection,[2] the test rate among partners is often low, partly because male contacts have to have a urethral swab taken by a doctor.
As the polymerase chain reaction can successfully detect infection in urine samples,[3] we investigated whether the test rate could be increased by asking the male contacts of infected women to send a urine sample directly from home to a laboratory instead of having a doctor take a urethral swab.
Subjects, methods, and results
Ninety six women with C trachomatis infection seen in general practices in Aarhus County, Denmark, were randomly divided according to their date of birth into an intervention group (45 patients) and a control group (51 patients). Women in die intervention group were asked to complete a questionnaire, including the number of male sexual partners over the preceding six months, and to supply their partners with an envelope containing a 10 ml sterile container, information on collecting the first urine sample of the morning, and a prepaid envelope for returning the sample to the laboratory at the Aarhus University Hospital. Envelopes supplied by the control group contained a request for the partner to visit his doctor as well as a contact slip and a prepaid envelope to be given to the doctor for returning a urethral swab sample.
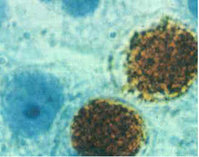
Swab samples were examined by enzyme immunoassay (MicroTrak II, Behring, Germany). Specimens with an optical density greater than 30% of the recommended cut off point were confirmed by polymerase chain reaction assay (Amplicor, Roche, Switzerland).[4] Urine samples were analysed by the same polymerase chain reaction. It sample was considered positive only if the result was confirmed on retesting.
The table shows the results of contact tracing. Forty four out of 65 (68%) partners were examined in the intervention group compared with 19 out of 68 (28%) in the control group ([chi square] 2 = 19.50; P [is less than] 0.01). The difference in test rate was 0.4 (0.68 minus 0.28) (95% confidence interval 0.24 to 0.56). Although not significant, there were more new cases of C trachomatis per index case in the intervention group (0.27) than in the control group (0.14). The difference between the two groups was 0.13 (-0.03 to 0.29). Furthermore, there was a trend for partners of women in the intervention group to be tested earlier than those of women in the control group, with a mean delay time of 12.6 days and 17.7 days respectively. Thus the difference between the two groups was 5.1 days (-1.6 to 11.8). The prevalence of C trachomatis in samples from the intervention and control groups was 27% and 39% respectively.
(*) Result unknown for one partner.
Comment
Contact partners of women with C trachomatis infection may be deterred from seeking medical help because of the intimate nature of the infection and because a urethral swab is needed. Urine samples obtained at home provide a non-invasive and less time consuming alternative.
A similar procedure for contact tracing of female partners of men infected with C trachomatis should be considered as the organism has been detected in urine samples from Women.[5]
We thank the participating general practitioners.
Contributors: BA coordinated the primary study hypothesis and the core ideas, designed the protocol, obtained approval from the ethics committee, coordinated inclusion of patients, scanned the data, and coordinated the interpretation of results and writing of the paper. LO discussed the primary hypothesis, core ideas, analysis, and protocol design and participated in the interpretation of results and writing of the paper. JKM discussed the hypothesis and ideas, led the analysis of the samples obtained, participated in die interpretation of results, and edited the paper. FO discussed the hypothesis and core ideas and participated in the protocol design, coordination of contact with the general practitioners, the interpretation of results, and the writing of the paper. FO is the guarantor of the paper.
Funding: University of Aarhus, Denmark and Nycomed DAK.
Conflict of interest: None.
[1] Cates W Jr, Wasserheit JN. Genital chlamydial infections: epidemiology and reproductive sequelae. Am J Obstet Gynecol 1991;164:1771-81.
[2] Ripa T. Epidemiologic control of genital Chlamydia trachomatis infections. Scand J Infect Dis Suppl 1990;69:157-67.
[3] Jaschek G, Gaydos CA, Welsh LE, Quinn TC. Direct detection of Chlamydia trachomatis in urine specimens from symptomatic and asymptomatic men by using a rapid polymerase chain reaction assay. J Clin Microbiol 1993;31:1209-12.
[4] Ostergaard L, Moller JK. Use of PCR and direct immuno-fluorescence microscopy for confirmation of results obtained by Syva MicroTrak Chlamydia enzyme immunoassay. J Clin Microbiol 1995;33:2620-3.
[5] Ostergaard J, Moller JK, Andersen B, Olesen E Diagnosis of urogenital Chlamydia trachomatis infection in women based on mailed samples obtained at home: multipractice comparative study. BMJ 1996;313:1186-9.
(Accepted 25 April 1997)
See p 351
Research Unit and Department of General Practice, University of Aarhus, DK-8000 Aarhus C, Denmark
Berit Andersen, research assistant
Frede Olesen, consultant physician
Aarhus University Hospital, DK-8000 Aarhus C
Lars Ostergaard, senior registrar of infectious diseases
Jens K Moller, director of clinical microbiology Correspondence to: Dr Andersen ba@alm.aau.dk
BMJ 1998;316:350-1
COPYRIGHT 1998 British Medical Association
COPYRIGHT 2000 Gale Group