Home Study Program
NEONATAL CLEFT LIP AND CLEFT PALATE REPAIR
The article "Neonatal cleft lip and cleft palate repair" is the basis for this AORN Journal independent study. The behavioral objectives and examination for this program were prepared by Rebecca Holm, RN, MSN, CNOR, clinical editor, with consultation from
Susan Bakewell, RN, MS, education program professional, Center for Perioperative Education.
A minimum score of 70% on the multiple-choice examination is necessary to earn 2 contact hours for this independent study. Participants receive feedback on incorrect answers. Each applicant who successfully completes this study will receive a certificate of completion. The deadline for submitting this study is March 31, 2005.
Send the completed application form, multiple-choice examination, learner evaluation, and appropriate fee to
AORN Customer Service c/o Home Study Program 2170 S Parker Rd, Suite 300 Denver, CO 80231-5711
or fax the information with a credit card number to (303) 750-3212.
BEHAVIORAL OBJECTIVES
After reading and studying the article on neonatal cleft lip and cleft palate repair, the nurse will be able to
(1) discuss the epidimiology of cleft lip and cleft palate deformities,
(1) define the anatomy pertinent to cleft lip and cleft palate deformities,
(2) identify the risks involved with neonatal surgery,
(3) discuss current options for repairing cleft lip and cleft palate deformities,
(4) describe the intraoperative care of the neonate undergoing cleft lip and cleft palate repair, and
(5) explain the postoperative care required by the neonate recovering from cleft lip and cleft palate repair.
This program meets criteria for CNOR and CRNFA recertification, as well as other continuing education requirements.
The birth of an infant is an exciting and stressful event, even when the pregnancy, labor, and delivery go well. For the parents of an infant born with a facial anomaly, however, it can be a devastating experience. Facial clefting is one of the most common birth deformities. Feelings of fear, guilt, resentment, inadequacy, shame, and grief are common among parents and family members of babies born with cleft deformities. (1) Such feelings can interfere with parent-infant bonding and may have psychosocial effects on both the infant and family members. (2) Reactions of family members, friends, and even strangers can be painful for the parents of these babies. The usual smiles of others often turn to looks of discomfort and surprise. Infants with facial deformities also may have substantial feeding difficulties and impaired speech development. Speech difficulties, in combination with abnormal facial appearance, can heighten parental stress and decrease acceptance from society when repair of a cleft lip and palate are delayed. Early repair of cleft lip and palate deformities during the neonatal period improves parent-infant bonding; aids in feeding, which promotes growth; and has positive effects on speech development.
EPIDIMIOLOGY
Cleft lip and palate is a common birth defect, occurring in approximately one out of every 700 live births. (3) Cleft deformities are more prevalent among people of Asian descent (ie, 2.1 out of every 1,000 live births). The incidence in people of Caucasian descent is one out of every 1,000 live births and the incidence among people of African American descent is among the lowest (ie, 0.4 out of every 1,000 live births). (4)
History shows that heredity plays a role in the occurrence of cleft lip and palate deformities. There is a 40% increase of clefting in siblings of a child with a cleft lip or palate. (5) Parental age also seems to be a contributing factor; the risk of having an infant with a cleft lip or palate deformity increases in parents older than age 30. (6) Certain medications, such as phenytoin sodium, have been shown to increase the incidence of cleft lip and palate. (7) No matter the cause, surgical repair is necessary for these babies.
EMBRYOLOGY
Clefting occurs when there is failure of fusion or diminished mesenchymal penetration between migrating embryological processes. An infant may be born with a cleft lip, a complete or incomplete cleft palate, or both. Between the fourth and eighth week in utero, the upper lip and palate form from the migration and connection of three bilateral processes (ie, nasomedial, nasolateral, maxillary). The nasomedial process forms the columnella of the nose, prolabium of the lip, and alveolar ridge of the maxilla. This portion of the true maxilla eventually will hold the two central and two lateral incisors. The premaxilla is the segment of bone from the back of the teeth to the incisor foramen from which the anterior palatal vessels and nerves emerge.
The nasolateral process forms the ala, dome, and sil of the nose. The maxillary process forms the canine to molar teeth. The junction of these three processes produces the intact maxilla and intact lip. Two maxillary processes produce the areas of the maxilla. The maxilla begins to close anteriorly and closure proceeds in the posterior direction. The maxilla fuses with the vomer bone and the nasal septum. When this process faults, a splitting of the normal anatomy may occur.
ANATOMY
The anatomy pertinent to cleft lip and palate consists of the upper lip, nose, and hard and soft palates. The mucosa, skin, muscle, cartilage, bone, and nerve and blood supplies to these areas may all be affected by a cleft defect.
Upper lip. The upper lip consists of the mucosa lining the inside of the mouth, obicularis oris muscle, and skin. The obicularis oris muscle allows the lip to smile and pout. There is no fat between the obicularis otis muscle and its attachments to the dermis of the skin. This anatomy is relatively distinct, and it is important during surgery to separate these three layers so they each can be repaired definitively. There is a very definite pout of the vermilion of the lip, known as the central tubercle, which acts as the mid-portion and thickest part of the upper lip. There is a very definite, but subtle, line between the wet and dry vermilion, which should be reproduced during surgical repair. The wet vermilion is slightly more red and moist compared to the dry vermilion, which is pinker in appearance. The philtral dimple is between the philtral ridges of the upper lip, which also must be reconstructed. The peaks of cupid's bow must be on a parallel line. The deformity easily will be noticeable after repair if one peak is higher than the other. Sensation of the lip is supplied from the infraorbital nerve, which also supplies the lateral ala of the nose. These nerves are not in the planes of the dissection and should not be injured.
Nose. The nose should be symmetrical with the ala bases in both the anterior and posterior plane as well as the superior and inferior plane. The nose and nostril openings also should be as symmetrical as possible. Figure 1 provides a comparison of the anatomical features of a normal developed lip and nose with those of a cleft lip deformity.
[FIGURE 1 OMITTED]
Palate. The hard palate constitutes approximately the anterior two-thirds of the roof of the mouth, and the soft palate constitutes the posterior one-third. The blood supply of the palate is provided anteriorly through the incisor foramen and posteriorly through the great palatine foramen where the great palatine artery emerges. When an infant has a cleft, the soft palate muscle apparatus, which normally elevates the palate, is attached abnormally to the posterior edge of the hard palate. This segment includes the levator palatini muscles and the palatal pharyngeous muscle complex. The tensor palatini muscle joins this muscular sling as it sweeps around the hamulus, a bony prominence of the lateral palate. On contraction, the tensor palatini muscle provides the vacuum that is needed to empty the eustachian tube, and the levator muscles provide the motion that is necessary to lift the soft palate to touch the posterior pharynx to close it off. The functions of the palate include swallowing, sucking, speech, and aiding inner ear drainage. Repairing the muscles of a cleft palate and placing them into a normal anatomical configuration allows these functions to occur. Figure 2 provides a comparison of the anatomical features in a normal developed palate with that of a cleft palate deformity.
[FIGURE 2 OMITTED]
HISTORY
Surgical cleft lip repairs have been reported as early as 390 AD in China. During this time period, cleft lip repair simply involved freshening the edges of the cleft and passing straight needles through each side of the wound. These wound edges then were approximated by passing a thread in a figure eight pattern. As recent as 1930, a wire was passed through the open structures of the lip, and approximation was achieved by twisting the wire until the sides collapsed together. (8) These early techniques simply closed the gap of the defect. Current surgical interventions focus on completing the failed embryological development through complete anatomical dissection and geometric rearrangement of muscle, mucosa, and skin flaps, resulting in a more satisfactory cosmetic and functional result. Until recently, early surgical repair of the cleft lip or palate in neonates was not considered safe. The "Rule of 10's" long has been the standard guideline. (9) This rule states that an infant must reach 10 pounds of body weight, 10 weeks of age, and have a hemoglobin level of 10 gm per 100 mL before it is considered safe to surgically perform a cleft repair. This rule eliminated neonates 28 days of age or younger from the possibility of early repair. Advances in neonatology and pediatric anesthesia now have made it possible to perform cleft repair surgery during the neonatal period.
RISKS OF NEONATAL SURGERY
The success of neonatal cleft lip and palate repair surgery is related directly to the expertise of the numerous practitioners involved (ie, plastic surgeons, pediatric anesthesia care providers, intensive care physicians, perioperative pediatric nursing staff members). The risks associated with elective neonatal surgery of any type are related closely to the anatomical and physiological differences between adults and neonates. The neonatal airway differs from an adult airway in the following important ways.
* The epiglottis is U-shaped and protrudes into the pharynx.
* The larynx is relatively cephalic in position.
* The vocal cords are short and concave.
* In infants and children less than eight years of age, the narrowest portion of the airway is at the cricoid cartilage below the vocal cords, which is in contrast to older children and adults in whom the narrowest portion of the airway is at the vocal cords.
These anatomical differences have the following important yet practical consequences.
* It is difficult to create a single clear visual plane from the mouth through the pharynx to the glottis, thus the potential is greater for difficult laryngoscopy or endotracheal intubation.
* Endotracheal tube size must be selected based on the size of the cricoid ring rather than the glottic opening, as usually is done.
* The lower airway of neonatal patients is smaller and its supporting cartilage less developed than in adults; therefore, neonatal patients' airways easily can become obstructed by mucus, blood, or edema.
Neonatal surgical patients are more likely to develop difficulties with airway management than adults. Neonatal patients have a higher metabolic rate; neonates consume oxygen at 6 to 8 mL per kg per minute compared to the adult rate of 3 to 4 mL per kg per minute. (10) Hypoxia occurs more rapidly because of this metabolic rate. (11)
Neonates with a cleft lip or palate may have other associated syndromes or congenital anomalies. For this reason, a complete medical evaluation before surgery is essential.
Neonates also have more difficulty maintaining their own body temperature as a result of the distribution of brown fat. Brown fat is the major source of heat production through a process of nonshivering thermogenesis. A cold-stressed neonate is at risk for hypoxemia, metabolic acidosis, rapid depletion of glycogen stores, and reduction of blood glucose levels. (12) Neonates can lose body heat through four mechanisms of heat loss, including radiation, convection, conduction, and evaporation.
* Radiation is the loss of heat in the form of radiant energy from a warmer surface (ie, the body) to a cooler one (ie, the environment) even though the two are not in direct contact.
* Convection, which is the loss of heat through circulating air currents, depends on the temperature gradient between the body and ambient air (ie, wind chill factor).
* Conduction is the loss of heat from a warmer surface through direct contact with a cooler one. For example, heat is lost from the body to the cooler OR bed and to cold sheets and drapes.
* Evaporation is the transfer of heat as fluids convert to a gaseous state. Most evaporation occurs from exposed viscera, perspiration, respiration, or drying of prepping solutions. (13)
CRANIOFACIAL TEAM
Each patient is evaluated by a pediatric anesthesia care provider. Laboratory tests (eg, hemoglobin, hematocrit, platelet count) are ordered routinely. The neonate is evaluated for any cardiac or respiratory problems and other congenital anomalies. Referrals are made, as needed, and family members are counseled regarding the anesthetic risks. Many neonates are diagnosed by prenatal ultrasound, which allows parents to meet with craniofacial team members before the birth of their infant. These parents have time to become more informed about cleft deformities and have the support of the craniofacial team, which can decrease parental stress and anxiety. The craniofacial team consists of dentists, orthodontists, social workers, speech therapists, feeding specialists, psychologists, and otolaryngologists in addition to plastic surgeons, anesthesia care providers, and nurses. When a representative of the craniofacial team meets the parents, he or she offers support in several ways. First and foremost, a craniofacial team member educates the parents regarding cleft deformities and available treatment. Second, the team member helps parents gain realistic expectations through education regarding their infant's appearance after surgery.
The craniofacial team members provide the parents with pictures of other patients to help them visualize the repair process. Pictures also show immediate postoperative sutures and swelling. A craniofacial team member teaches the parents that infants are obligate nasal breathers and that their baby may be fussy after the procedure related to the anatomical changes in the palate and nasal anatomy. Someone from the team also teaches the parents about normal postoperative edema and bruising, which decreases within 48 to 72 hours. Craniofacial team members are available to teach troubleshooting techniques with regard to feeding.
A member of the craniofacial team introduces the new parents to the parent-to-parent network available to parents of infants with cleft deformities. This parent-to-parent networking provides support and information that can help prepare parents for their infant's surgical procedure. The parent-organized web site http://www.cleft.org is another parent-to-parent support method. It provides information regarding cleft lip and palate, including how to care for these infants at home before and after surgical repair.
PREPARATION OF THE OPERATING ROOM
The circulating nurse, scrub person, and anesthesia care provider work cooperatively to prepare the OR for the procedure. A perioperative team member performs the following tasks before the neonate is brought into the room:
* places gel-filled pads on the OR bed to protect the neonate's skin by reducing skin pressure;
* checks the functional status of the electrosurgical unit, suction, and OR lights;
* brings needed supplies, instruments, and equipment into the room;
* brings the plastic surgery specialty cart into the room for immediate access to specialty plastic surgery supplies;
* places all equipment in the proper position, keeping in mind that the OR bed will be turned 90 degrees after induction of general anesthesia;
* ensures that a variety of appropriately sized endotracheal tubes are available;
* ensures that special tape is available to prevent damage to the neonate's fragile skin; and
* places a shoulder roll close to the OR bed to be used for positioning the patient to provide increased palatal exposure for the procedure.
The goal of patient care related to temperature regulation is to maintain the neonate's body temperature at approximately 36 [degrees] C (98.8 [degrees] F). The OR bed is warmed using temperature-regulating blankets. These blankets then are covered with sheets that are warmed by radiant heat lamps until the neonate is brought into the room to prevent heat loss through conduction. Additional measures that also are employed to reduce heat loss include
* decreasing the amount of skin surface exposed during the surgical procedure;
* wrapping the neonate's extremities with cotton cast padding and plastic wrap;
* covering the neonate's head with a cap; and
* increasing the OR temperature to 26.7 [degrees] C (80 [degrees] F) and keeping it at that temperature during the entire surgical procedure.
PREOPERATIVE CARE
When the infant and family members arrive in the preoperative holding area, they are greeted by the circulating nurse and anesthesia care provider. All perioperative team members must remember that they are greeting a family under a great deal of stress, and events are happening quickly for them. The mother has given birth recently and may be experiencing the hormonal fluctuation of the postpartum period. In addition, family members and friends, while trying to be supportive during this time, may be experiencing many different emotions of their own regarding the situation. Family members need reassurance that the infant will not experience pain during the surgical procedure. They also may be worried about the infant's postoperative appearance. The perioperative nurse must support and educate family members by taking time to talk with them regarding the surgical procedure in an unhurried manner and by encouraging questions.
Cleft lip and palate surgery takes approximately three hours. A staff member will speak to family members every hour during surgery to let them know how the infant is doing. The parents are informed that they will be able to be with their infant in the postanesthesia care unit (PACU) after the surgical procedure and after the PACU nurse has initiated monitoring and the infant is stable.
The circulating nurse assesses the neonate's skin color, level of consciousness, and movement. The nurse then checks the medical chart for a signed informed consent form, verifies with the parents the patients' allergies and NPO status, and reviews the history and physical examination information, laboratory results, most recent weight, and other pertinent medical information. Based on this assessment, the circulating nurse establishes a nursing care plan specific to this patient. Table 1 outlines the patient-specific nursing diagnoses and plan of care appropriate for a neonate undergoing cleft lip and palate repair.
INTRAOPERATIVE CARE
When the circulating nurse and scrub person have completed preparation of the OR, the anesthesia care provider carries the neonate to the OR. In the room, the neonate can be held or placed on the bed for a mask induction of anesthetic agents. The circulating nurse assists the anesthesia care provider by applying appropriately sized electrocardiogram pads, blood pressure cuff, and pulse oximeter. If the infant has a pacifier, it can be left in place during induction, acting as an oral airway, and it is removed after the infant is asleep. An assisting anesthesia care provider places an IV line and administers medication in preparation for intubation. The primary anesthesia care provider intubates the neonate using an appropriately sized oral RAE endotracheal tube. This tube is taped in the midline so it does not distort the anatomy of the lip.
Positioning. The circulating nurse gently log rolls the neonate to his or her side, checks skin integrity, and applies a pediatric electrosurgical unit dispersive pad on the neonate's back. Any alterations in skin integrity (eg, lesions, rashes) are noted on the intraoperative record. The circulating nurse inserts a lubricated rectal temperature probe and tapes it to the neonate's leg to prevent dislodgement during the procedure. This allows the anesthesia care provider to monitor the neonate's temperature throughout the procedure. During induction and the preparatory phase, radiant heat lamps are used to maintain the neonate's temperature and prevent chilling. The circulating nurse and anesthesia care provider position the neonate with his or her head at the end of the OR bed in a gel head ring with a shoulder roll placed horizontally under his or her shoulders. The shoulder roll allows for hyperextension of the neonate's head, which provides greater exposure of the surgical site. The assisting anesthesia care provider and the circulating nurse place a stocking cap on the neonate's head and wrap the neonate's arms and legs with cotton cast padding and plastic wrap for temperature regulation. They position the neonate in an anatomically correct supine position, ensuring that elbows and heels are padded, and place a warm sheet over the neonate from the chest down.
Surgical prep. The surgeon inserts the cleft palate mouth gag and infiltrates the palatal structures with 5 mg per kg of 0.25% lidocaine with epinephrine 1:400,000 using a 3-mL syringe. This size syringe generates enough force to cause hydrodissection of the palatal tissues, thus decreasing the amount of bleeding during the procedure. Infiltration is performed before prepping and draping the neonate to allow time for the hemostatic action of the epinephrine to become effective.
The circulating nurse preps the neonate's face with betadine soap three times followed by betadine solution three times. He or she preps the neonate's face and mouth and also the mouth gag in a circular manner, proceeding from the incision line circumferentially outward. The nurse ensures that prep solution does not get into the neonate's ears or pool under the his or her neck. The surgeon and scrub person then apply the surgical drapes.
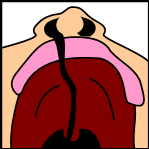
Surgical procedure. If the neonate has both a cleft lip and cleft palate, the palate is repaired first so that the lip is not disrupted after it has been repaired. The surgeon places a radiopaque sponge in the back of the neonate's throat to minimize the amount of blood ingested and then makes an incision along the hard palate. The surgeon exposes the tensor veli palatini and levator palatini muscles, but only as much as necessary to limit scarring, which increases the potential for problems with postoperative palate mobility.
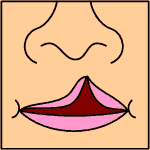
The surgeon makes releasing incisions along the lateral aspects of the soft palate so there is no tension along the medial closure line. This limits the potential for fistula formation. The surgeon makes additional incisions in the nasal mucosa and the posterior edge of the soft palate musculature where it is abnormally attached to the hard palate. The surgeon elevates the oral mucosa just enough to allow for the edges to be sewn together. Suture material for the closure is dependent on the size of the neonate. Beginning at the uvula and working anteriorly, the surgeon closes the mucosa of the nasal side using a 4-0, 5-0, or 6-0 braided absorbable suture with a small, specially designed fishhook needle. This needle allows the surgeon greater control when placing the suture in tight spaces, such as the vomer area or posterior pharynx. The surgeon closes the oral mucosa and muscle layers using braided absorbable suture in a horizontal mattress fashion (Figure 3). Cellulose gauze, which dissolves in seven to 10 days, is placed over the raw surfaces of the hard palate to assist with hemostasis. The surgeon places a traction suture in the neonate's tongue, which can be used if postoperative airway obstruction occurs. The position of the tongue can be changed by pulling downward on the traction stitch, thus relieving the airway obstruction. The mouth gag then is removed carefully, avoiding inadvertent extubation.
[FIGURE 3 OMITTED]
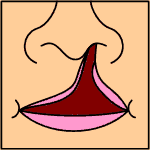
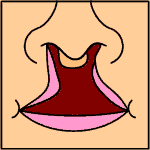
Repair of the cleft lip begins after completion of the cleft palate repair. The surgeon uses methylene blue to tattoo the desired anatomical design of the lip and then injects 5 mg per kg of 0.25% lidocaine with epinephrine 1:400,000. The goals of cleft lip repair are symmetry of the nostril floor and nostril sil and a natural appearance of cupid's bow. The surgeon also strives for a functional repair of the muscles and an aesthetically pleasing approximation of the skin edges. The two most common techniques for the repair of the cleft lip are the Tennison-Randall triangular flap and the Millard rotational advancement technique. The Tennison-Randall triangular flap recognizes that cupid's bow is high on the cleft side. A diagonal incision is made directly above the raised peak and onto the philtrum. A triangular defect is created by this incision, which is filled at closure with a triangular flap from the cleft side, thus tissue is added to the lower one-third of the lip on the non-cleft side. The major disadvantage of this method is that the z-plasty crosses the philtral line (ie, the vertical groove on the surface of the upper lip) below the nose. The advantage of this technique is that length is added to the medial lip element, rebuilding a functional nostril floor and preserving cupid's bow.
The Millard rotational advancement technique advances a triangle of tissue in the upper one-third of the lip. A distinct difference between this method and the Tennison-Randall triangular flap is that the philtral line is not crossed. The surgeons at Children's Hospital Of The King's Daughters, Norfolk, Va, employ a combination of both techniques, which allows them to address the differences of each neonate's cleft lip. In most procedures, 5-0 braided absorbable suture on a small cutting needle is used for closure of the muscle layer. A 7-0 chromic suture, followed by surgical glue, is used to close the skin (Figure 4). This surgical glue allows for skin closure with a decrease in the amount of suture material needed, thus creating a more pleasing cosmetic result. No further dressing is needed. The throat pack is removed, and the anesthesia care provider extubates the neonate in the OR. The circulating nurse and anesthesia care provider transport the neonate on a stretcher or isolette to the PACU. Arm restraints are not used at Children's Hospital Of The King's Daughters, and no difficulties with surgical site compromise have thus far been encountered.
[FIGURE 4 OMITTED]
POSTOPERATIVE CARE
The goals of PACU nursing care include airway maintenance, hemostasis, pain control, and age-related concerns. On arrival in the PACU, the assigned nurse verifies stability by assessing the patency and adequacy of oxygenation, initiating oxygen therapy, and monitoring oxygen saturation using pulse oximetry. The circulating nurse and anesthesia care provider give report to the PACU nurse, including information about the surgical procedure and other psychosocial information. The PACU nurse frequently monitors the neonate's pulse oximetry, respiratory rate and depth, applies humidified oxygen, and assesses breath sounds. Any patient undergoing surgery in or around the airway, especially the neonatal patient, is at risk for a laryngospasm. Though it is most likely to occur in the OR during extubation, it can occur postoperatively in the PACU. If a laryngospasm occurs in the PACU, the PACU nurse would administer oxygen by mask with positive pressure while an anesthesia care provider is summoned. If this is unsuccessful in stopping the laryngospasm, the PACU nurse may need to administer 0.5 to 1.0 mg per kg of succinylcholine by IV.
In the event of airway obstruction, the nurse repositions the patient supine and ensures that the tongue is not obstructing the airway by applying jaw thrust or chin lift. If airway obstruction continues, the nurse pulls downward on the tongue traction stitch to reposition the tongue, which relieves the obstruction.
The structures of the lip and palate are very vascular, which makes hemostasis a critical postoperative concern. The PACU nurse observes for bleeding by monitoring the lip and palate and watching for excessive swallowing, which may indicate that the neonate is swallowing blood. If the lip is bleeding, the nurse applies pressure or ice.
Postoperative pain from cleft lip and palate repair also is a concern but often is difficult to assess. The nurse monitors and assesses behavioral clues, such as crying and body movements. Pain control measures include comforting of the neonate by staff members or parents and administration of acetaminophen. Narcotic agents rarely are used because of their potential for causing respiratory depression.
Another postoperative priority is to reunite the neonate with his or her parents. Simply being held and comforted by a parent can decrease pain, anxiety, and bleeding. Neonates are allowed to feed via breast or bottle immediately after surgery, which has not proven to compromise the suture line. The average hospital stay after cleft lip and palate repair is one to two days. Parents and family members often are overwhelmed with the change in their infant's appearance postoperatively in comparison to the preoperative deformity though complete healing takes several months (Figures 5 and 6).
[FIGURES 5-6 OMITTED]
DISCHARGE AND HOME CARE
The infant is discharged to home with his or her parents after they receive home care instructions from a variety of craniofacial team members. The nurse instructs the parents to report redness or drainage at the incision site; a rectal, axillary, or tympanic temperature of 101 [degrees] F (38.6 [degrees] C); or pain as demonstrated by increased crying or fussiness that is uncontrolled with acetaminophen. A feeding specialist will have worked with the parents while the neonate is in the hospital, and the neonate should be eating well by discharge; however, the parents are instructed to report any feeding problems in the unlikely event that they occur. The nurse instructs the parents to make a follow-up appointment with the surgeon at one week and eight weeks postoperatively. The parents are encouraged to return to normal activities with their infant after discharge from the hospital. There are no postoperative limitations on activities.
CONCLUSION
To date, 214 neonatal cleft lip and palate repairs have been performed at Children's Hospital Of The King's Daughters. The most common complication is the formation of a palatal fistula, which is a repairable complication. The rate of palatal fistula at Children's Hospital Of The King's Daughters is 6%. Neonatal cleft lip and palate repair, therefore, is considered safe, has positive effects on parent-neonate bonding and speech development, improves feeding, and promotes growth.
NOTES
(1.) American Cleft Palate-Craniofacial Association, Parameters for Evaluation and Treatment of Patients with Cleft Lip/Palate or Other Craniofacial Anomalies (Pittsburgh: American Cleft Palate-Craniofacial Association, 1993) 19-26.
(2.) J Atwell, ed, Paediatric Surety (New York: Oxford University Press, 1998) 798-799.
(3.) R C Barden et al, "Effects of craniofacial deformity in infancy on the quality of mother-infant interactions," Child Development 60 (August 1989) 819-824.
(4.) S Berryman, Operation Smile Cleft Lip and Cleft Palate Interdisciplinary Training Manual (Norfolk, Va: Operation Smile Education Department, 1999) 1-1 -1-6, 6-1 - 6-13.
(5.) M J Denk, M P Magee, Jr, "Cleft palate closure in the neonate: Preliminary report," The Cleft Palate-Craniofacial Journal 33 (January 1996) 57-61.
(6.) M J Eliason, M A Hardin, W H Olin, "Factors that influence ratings of facial appearance for children with cleft lip and palate," The Cleft Palate-Craniofacial Journal 28 (April 1991) 190-194.
(7.) M J Eliason, "Cleft lip and palate: Developmental effects," Journal of Pediatric Nursing 6 (April 1991) 107-113.
(8.) E N Elmendorf III, L L D'Antonio, R A Hardesty, "Assessment of the patient with cleft lip and palate: A developmental approach," Clinics in Plastics Surgery 20 (October 1993) 607-621.
(9.) M C Jones, "Facial clefting: Etiology and developmental pathogenesis," Clinics' in Plastic Surgery 20 (October 1993) 599-606.
(10.) S S Maldonado, C Nygren, "Pediatric surgery," in Alexander's Care of the Patient in Surgery, 11th ed, M H Meeker, J C Rothrock, eds (St Louis: Mosby, 1999) 1247-1250.
(11.) D R Millard, Jr, "Introduction to clefts 1993: Past, present, and future," Clinics in Plastic Surgery 20 (October 1993) 597-598.
(12.) L F Whaley, D L Wong, Nursing Care of Infants and Children, third ed (St Louis: Mosby, 1987) 315-316.
(13.) R Moss, "Inadvertent perioperative hypothermia," (Clinical Issues) AORN Journal 67 (February 1998) 5-17.
RESOURCES
Operation Smile, www.operationsmile.org (accessed 30 Jan 2002).
Smile, http://www.cleft.org (accessed 30 Jan 2002).
AORN, Association of periOperative Registered Nurses, is accredited as a provider of continuing education in nursing by the American Nurses Credentialing Center's (ANCO's) Commission on Accreditation. AORN recognizes this activity as continuing education for registered nurses. This recognition does not imply that AORN or the ANCC's Commission on Accreditation approves or , endorses any product included in the activity. AORN maintains the following state board of nursing provider numbers: Alabama ABNPO075, California CEP 13019, and Florida FBN 2296. Check with your state board of nursing for acceptability of education activity for relicensure.
Professional nurses are invited to submit manuscripts for the Home Study Program. Manuscripts or queries should be sent to Editor, AORN Journal, 2170 S Parker Rd, Suite 300, Denver, CO 802315711. As with all manuscripts sent to the Journal, papers submitted for Home Study Programs should not hove been previously published or submitted simultaneously to any other publication.
Answer Sheet
NEONATAL CLEFT LIP AND CLEFT PALATE REPAIR
Please fill out the application and answer form on this page and the evaluation form on the back of this page. Tear the page out of the Journal or make photocopies and mail to:
or fax with credit card information to (303) 750-3212.
A score of 70% correct is required for credit.
Program offered March 2002.
The deadline for this program is March 31, 2005.
1. Record your six-digit member identification number in the appropriate section below (see your member card).
2. Completely darken the space that indicates your answer to the examination starting with question one. Use blue or black ink.
3. Record the time required to complete the program --
4. Enclose fee if information is mailed.
[ILLUSTRATION OMITTED]
Debra J. Sandberg, RN, CNOR, is a perioperative staff nurse and RN first assistant at Children's Hospital Of The King's Daughters, Norfolk, Va.
William P. Magee Jr, DDS, MD, FACS is the chief of the department of plastic surgery and director of the craniofacial cleft lip and cleft palate team at Children's Hospital Of The King's Daughters, Norfolk, Va; an associate professor at Eastern Virginia Medical School. Norfolk, Va; and the chairman of the board and cofounder of Operation Smile.
Michael J. Denk, MD, FACS, is a plastic surgeon at Children's Hospital Of The King's Daughters, Norfolk, Fa, and an assistant clinical professor at Eastern Virginia Medical School, Norfolk, Va.
COPYRIGHT 2002 Association of Operating Room Nurses, Inc.
COPYRIGHT 2002 Gale Group