Over 5,000 babies are born each year in the United States with a cleft lip or palate (about 1 in every 700 births). Cleft lip without cleft palate is the third most common congenital malformation among babies born in the United States, and is estimated to occur roughly twice as often in males than in females. Cleft palate without cleft lip is the fifth most common, and it affects roughly twice as many girls as boys. Clefts may be unilateral (affecting the left or right side only) or bilateral (affecting both sides). Left-side clefts represent 70% of all unilateral clefts. Research in the 1980s and 1990s indicated that the incidence of lip and palate clefts was increasing. In the United States, Native Americans have the highest incidence of clefts, at 1 in 278 live births, and African Americans have a lower incidence, at 1 in 3,330 live births. Among whites of European descent, there is a facial cleft rate of approximately 1 in 750 live births.
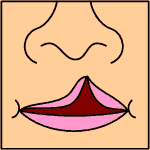
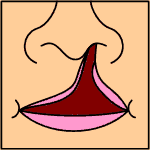
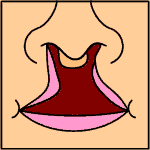
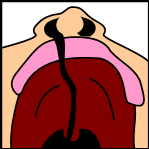
During the first nine weeks of normal fetal development, the bony and muscular parts of the face, mouth, and throat come together. It is during the fifth through ninth weeks of fetal development that genetic and environmental factors are most likely to affect lip and palate development. Cleft palate occurs when the right and left segments of the palate fail to join properly. Cleft lip occurs when the lip elements fail to come together. A cleft lip may be complete, extending through the entire length of lip to the floor of the nose. Alternatively, the cleft lip may be incomplete, with some closure in the muscle and lip area between the mouth opening and the nose. The incomplete cleft lip results in less facial distortion because the connected parts of muscle and tissue have a stabilizing effect. In a complete cleft lip, the muscles pull away from the center of the face, resulting in distortion of the nose and mouth.
Causes of clefts are not completely known or understood; in fact, there does not appear to be a single factor that contributes to all clefts. Most scientists believe that clefting is multifactorial, that is, it occurs as a result of a combination of genetic and environmental factors. In the United States and western Europe, researchers report that a family history of facial clefts is present in approximately 40% of all cases. The likelihood of a baby being born with a facial cleft increases if a first degree relative (mother, father, or sibling) has a cleft. Alcohol and drug abuse, lack of vitamins (especially folic acid) during the first weeks of pregnancy, and diabetes mellitus in the mother all appear to be related to the occurrence of facial clefts. Researchers from the California Birth Defects Monitoring Program found that women considering pregnancy may be able to reduce the risk of facial clefts (and possibly other birth defects) by taking a multivitamin containing folic acid for one month prior to becoming pregnant and for at least the first two months after conception.
Although some types of clefts can be detected during pregnancy by an ultrasound test, many are not discovered until birth. Generally, within the first few days following birth of an infant with a facial cleft, a team will be assembled to prepare a plan for treatment of the cleft. The interdisciplinary team usually includes representatives from several medical or psychological disciplines, including pediatrics, plastic surgery, otolaryngology, orthodontia, prosthodontics, oral surgery, speech and language pathology, audiology, nursing, and psychology. It is common for one team member, often a nurse with specialized training, to coordinate service and communication between the team members and the family. The cleft defect is corrected by a series of surgeries, the first of which may be performed within the first days after birth. Other aspects of physical and psychological development for a child with a cleft lip or palate are managed by other members of the team.
Children with clefts of the palate are at risk for ear infections, since the palatal muscles may not function efficiently to open the small tubes connecting the throat to the middle ear (eustachian tubes). For this reason, an otolaryngologist (ear, nose, and throat or ENT specialist) is included on the team. An audiologist will also participate in the infant's early care, testing his hearing using special audiometric equipment designed for use with infants and toddlers.
Related to the increased vulnerability of the ears is a greater risk of speech development problems. A speech pathologist with knowledge about cleft lip and palate should evaluate the infant in the first six months of life, and at least once a year after that. Approximately 80% of children with cleft palate develop normal speech after the cleft is closed, although development may be slower than normal. For 20%, additional surgery and speech therapy will be necessary.
Infancy
Infants with cleft lip or cleft soft palate generally have few feeding problems. However, when the cleft involves the hard palate, the infant is usually not able to suck efficiently. For these infants, caregivers must experiment with various feeding techniques, such as specially shaped nipples or alternate feeding positions. The infant with a cleft should be held in nearly a sitting position (at least at a 45-degree angle) during feeding to minimize the chance that the breastmilk or formula will flow back into the nose. In addition, the infant should be burped frequently, approximately every three or four minutes. The sucking reflex is strong in all infants, and should be encouraged in infants with facial clefts even if the sucking is inefficient, since the reflex appears to contribute to later development of speech. It is important to keep the cleft clean, and not to allow formula, mucous, or other matter to collect in the cleft.
DEALING WITH CLEFT LIP OR PALATE
Parents of a newborn baby with a cleft lip or palate are often confused and afraid of the impact the defect will have on their child's life. These feelings can be alleviated by learning about the cleft and the processes required to correct it. They also must communicate with family, siblings, and friends about what they are learning about clefts. It is important for people who come into contact with the child to realize that a cleft is not a wound, although it may give the impression that it is tender or sore. Parents can help others to understand that the cleft does not hurt, and that it will be repaired. To ensure normal psychological and speech development, parents should interact with their infant-talking, singing, taking photographs-- as they would any newborn in the family, and should encourage others to do the same.
As the child with a cleft grows and develops, he or she will certainly experience many good and bad reactions from adults and children. Other children may tease the child or use the term "harelip." it may be helpful for parents of a child with a facial cleft to meet with his classmates and teachers to explain the history of the term "harelip." Although a facial cleft was once referred to as a "harelip" to reflect its similarity to the mouth of a rabbit, the term is considered rude and insulting today. Educating adults and children about cleft lip and palate is the best way to relieve others' anxiety about the defect and lessen any negative psychological effects that bad reactions might have on the child.
Toddlerhood
As the child moves from infancy to toddlerhood, speech and hearing development continue to be monitored. Additional surgeries may be performed to continue to correct and refine the cleft. In addition, a pediatric dentist cares for the newly developing teeth. An appliance to help with speech development, known as an obturator, may also be prepared by a prosthodontic specialist to support the development of normal speech.
If a child is enrolled in a preschool program, teachers and staff should be briefed on the child's situation, the progress that has been made in correcting the cleft, and the special support the child may need as he or she begins the first organized school experience. If the child has difficulty adjusting psychologically to the cleft and to the reactions of others, a psychologist can be consulted to help the child cope with his feelings.
School-age years
Beginning elementary school is an exciting time for all children and their families. In most cases, the surgeries required to close the cleft have been completed by this time. Speech therapy and counseling continue through these years. At around the time the child is ready to enter school, the cleft palate team, in consultation with the family, may consider the need for additional surgery to improve the physical appearance of the cleft. These surgeries usually involve improving the symmetry and appearance of the nose and lips. The child's face will continue to grow and develop--for boys until about 16-18 years of age, for girls until about 14-16. The decision to undergo surgeries for improvement of appearance must take further growth and psychological factors into consideration. Consultation with members of the cleft palate team will help the parents and child decide when to do the final touch-ups.
School-age children may also need reconstructive work to improve the appearance and function of the teeth and gums. When the cleft goes through the upper gum, there may be insufficient bone to support the permanent teeth, and a bone graft may be recommended. A small piece of bone, usually from the child's hip, ribs, or leg, is removed and grafted into the gum area at the front of the mouth near the teeth. Orthodontic treatment is usually necessary either prior to or after the graft.
With advances in surgical techniques and with more complete repair of facial clefts at an early age, it is realistic to expect 80% of children with clefts to have normal speech development by the time they enter school. Continuation of speech therapy will result in continuous improvement for most common speech problems.
Adolescence
Adolescents face universal challenges in forming their own identities. It appears that teenagers with cleft lip or palate are just as likely to be emotionally healthy as their peers. The primary problems related to cleft lip and palate that persist into adolescence affect appearance and speech. During adolescence, facial growth is nearly complete, making it possible to perform any refinements to the nose and mouth areas, if necessary or desirable. Speech problems such as misarticulation (mispronouncing words) and hypernasality (nasal tone of voice) may still appear in adolescence, even though speech therapy may have successfully controlled both. These two problems increase with fatigue, and an adolescent's lifestyle may regress speech improvement. In some cases, the repaired palate may not be growing at a sufficient rate to prevent nasality from developing. The cleft palate team can assess the adequacy of the palate for speech functioning and suggest a strategy for treatment. In adolescence, the palate may need some additional minor repair, or the teen may be instructed to use a prosthetic device to improve palate closure until the palate growth is sufficient.
Some adolescents may want to join a support group of people with clefts of the lip or palate. Most of these groups are locally organized by parents of children with cleft lip or palate. The Cleft Palate Foundation is a national association that provides interested adolescents and their families with information about social or educational groups in their area.
Further Reading
For Your Information
Books
- Berkowitz, Samuel. The Cleft Palate Story: A Primer for Parents of Children with Cleft Lip and Palate. Chicago: Quintessence Books, 1994.
- Moller, Karlind T., Clark D. Starr, and Sylvia A. Johnson. A Parent's Guide to Cleft Lip and Palate. Minneapolis: University of Minnesota Press, 1990.
- Powers, Gene R. Cleft Palate. Austin, TX: PRO-ED, 1986.
- Starr, Philip. Cleft Lip and/or Palate: Behavioral Effects from Infancy to Adulthood. Springfield, IL: Charles C. Thomas, 1983.
- Wicka, Donna Konkel. Advice to Parents of a Cleft Palate Child. 2d ed. Springfield, IL: Thomas, 1982.
- Wynn, Sidney K. and Alfred L. Miller, editors. A Practical Guide to Cleft Lip and Palate Birth Defects: Helpful, Practical Information and Answers for Parents, Physicians, Nurses, and Other Professionals. Springfield, IL: Thomas, 1984.
Gale Encyclopedia of Childhood & Adolescence. Gale Research, 1998.