A 61-year-old white man with acute onset of edema of both lower extremities had mildly abnormal liver function tests, high serum iron indices (ferritin, 554.0 ng/ mL; iron saturation, 90%), and a heterozygous mutation of the hemochromatosis gene (H63D). Medical history, physical examination, and results of laboratory tests were otherwise unremarkable. Liver biopsy revealed marked fibrosis (Figure 1, A, hematoxylin-eosin; Figure 1, B, trichrome) and 2+ iron overload predominantly in periportal hepatocytes (Figure 2, Prussian blue). Iron deposition in the bile ductal epithelium and Kupffer cells was minimal. Unexpectedly, there were clusters of intracytoplasmic eosinophilic globular inclusions of various sizes predominantly in the periportal hepatocytes (Figure 1, A), which were periodic acid-Schiff positive diastase resistant (Figure 3, A) and immunoreactive to [alpha]^sub 1^-antitrypsin (AAT) antibody (Figure 3, B). Serum AAT level was 29 mg/dL, which was in the range for PiZ/Z homozygotes. Therefore, the patient had both hereditary hemochromatosis and AAT deficiency.
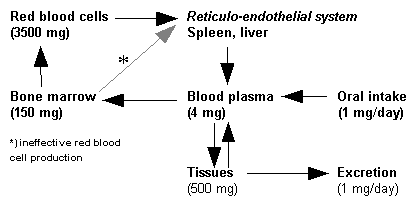
Hereditary hemochromatosis (HH)1,2 is an autosomal recessive disorder characterized by excessive accumulation of iron, most of which is deposited in the parenchymal organs such as liver and pancreas sometimes resulting in micronodular cirrhosis and diabetes mellitus. In addition, patients with HH have a 200-fold risk of developing hepatocellular carcinoma, which is the most common cause of death in such patients. HH is one of the most common inborn errors of metabolism in the US white population; 0.45% of individuals of northern European descent are homozygotes and 11% are heterozygotes. Symptoms are only seen in 25% of the affected individuals and usually first appear in the fifth to sixth decades of life. Men are more commonly affected (male-female ratio, 5-7:1). The genetic defects are 2 missense mutations in the hemochromatosis gene, HFE, located on chromosome 6p. HFE encodes a 343-amino acid transmembrane protein that mediates iron absorption through the small intestinal epithelium. Homozygotes for a less common gene mutation that results in a cysteine-to-tyrosine substitution at amino acid position 282 (C282Y) represent 83% of HH patients, although the more common mutation that results in a histidine-to-aspartate substitution at amino acid position 63 (H63D) is only found in 10% of HH patients. The remaining 5% to 10% of HH patients are heterozygous for C282Y and have mild to moderate iron overload. H63D heterozygotes usually do not have increased iron storage. Persons with homozygous or compound heterozygous (H63D on one gene, C282Y on the other) HFE gene mutations, especially C282Y homozygotes, should have serum iron indices, such as ferritin and transferrin iron saturation, evaluated, and a liver biopsy should be obtained if indicated. Early diagnosis and genetic counseling for the family members are critical because cirrhosis and other clinical diseases can be prevented by therapeutic phlebotomy, and a patient's life expectancy may return to normal. However, treatment for iron overload does not reduce the risk for hepatocellular carcinoma.
AAT deficiency1,3 is an autosomal recessive disorder marked by abnormally low serum levels of this protease inhibitor (Pi). The AAT gene on chromosome 14q encodes more than 75 forms of AAT. The most common deficiency alleles are PiZ and PiS; 90% of normal individuals have the PiM/M genotype. The frequency of the PiZ gene is 1.2%, and 1 in 7000 white people in North America are PiZ/Z homozygotes. The mutant PiZ allele has a missense mutation that results in a glutamic acid-to-lysine substitution, which causes abnormal folding and failure of secretion of AAT from the endoplasmic reticulum in hepatocytes and possible hepatic injury. PiZ/Z patients are prone to cirrhosis and emphysema and have an increased risk for hepatocellular carcinoma, which develops in 2% to 3% of AAT-deficient men. Although all patients with PiZ/Z genotype will have accumulated AAT in the liver, only 8% to 20% of them will have severe liver disease. AAT-deficient individuals usually have liver damage during infancy, and 10% to 20% of AAT-deficient newborns exhibit cholestasis. If they do not develop severe liver disease in childhood, they generally are disease free until late in life, when men are much more likely than women to be affected; for PiZ/Z patients between the ages of 51 and 60 years, the incidence of liver disease is 15% in men and 0% in women. The diagnosis of AAT deficiency is confirmed by low serum levels of AAT, Pi typing with isoelectric focusing in polyacrylamide gels, or single-strand conformational polymorphism analysis of paraffin-embedded liver tissue. AAT-deficient patients are usually managed with supportive measures; however, liver transplantation can be curative. AAT deficiency is the most common inherited disease for which liver transplantation is performed in children.
Although both hereditary hemochromatosis (HH) and AAT deficiency are relatively common in the white population, patients with both conditions are uncommon. It is unusual for H63D heterozygotes, such as this patient, to have iron overload. Whether the coexistent AAT deficiency may exacerbate iron overload in these patients is unclear. Analyses of a small series of patients have suggested possible association of these 2 conditions;4 however, study of a recent larger series failed to substantiate any association.5 It is still unclear whether coexistence of HH and AAT deficiency further increases the risk for hepatocellular carcinoma.
References
1. Crawford JM. Inborn errors of metabolic and pediatric liver disease. In: Kumar V, Cotran RS, Robbins SL, eds. Robbins Basic Pathology. 7th ed. Philadelphia, Pa: WB Saunders; 2003:615-619.
2. Bacon BR. Hemochromatosis: diagnosis and management. Gastroenterology. 2001;120:718-725.
3. Ishak KG, Sharp HL, Schwarzenberd SJ. Metabolic errors and liver disease. In: MacSween RNM, Burt AD, Portmann BC, Ishak KG, Scheuer PJ, Anthony PP, eds. Pathology of the Liver. 4th ed. Philadelphia, Pa: Churchill Livingstone; 2002: 174-180.
4. Rabinovitz M, Gavaler JS, Kelly RH, et al. Association between heterogenous [alpha]^sub 1^-antitrypsin deficiency and genetic hemochromatosis. Hepatology. 1992; 16:145-148.
5. Fargion S, Bissoli F, Fracanzani AL, et al. No association between genetic hemochromatosis and [alpha]^sub 1^-antitrypsin deficiency. Hepatology. 1996;24:1161-1164.
Rulong Shen, MD; Wendy L. Frankel, MD; Ping Wen, MD, PhD
Accepted for publication December 10, 2003.
From the Department of Pathology, The Ohio State University Medical Center, Columbus.
The authors have no relevant financial interest in the products or companies described in this article.
Reprints: Ping Wen, MD, PhD, Department of Pathology, The Ohio State University Medical Center, E-410 Doan Hall, 410 W Tenth Ave, Columbus, OH 43210 (e-mail: wen-2@medctr.osu.edu).
Copyright College of American Pathologists Apr 2004
Provided by ProQuest Information and Learning Company. All rights Reserved