Studies of the molecular function of HFE, the protein defective in hereditary hemochromatosis, have provided important insights into the control of intestinal iron absorption. A recent study suggests that HFE controls the recycling rate of the transferrin receptor and thereby ultimately controls the iron status of the enterocyte. In hereditary hemochromatosis, a defect in HFE causes relative iron starvation in the enterocyte leading paradoxically to the development of an "anemic" enterocyte phenotype in the midst of bountiful body iron stores. Despite ever-increasing stores of body iron, the inappropriately low iron status of the hereditary hemochromatosis enterocyte continues to drive the hyper-absorption of dietary iron, eventually leading to iron overload.
Key Words: enterocyte, hereditary hemochromatosis, intestinal iron absorbtion, HFE
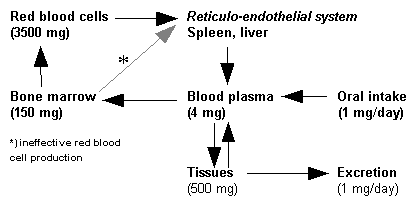
In the absence of blood loss, there is very little iron lost from the body. Endogenous iron losses are approximately 1 mg per day in men and, owing to regular blood loss with menstruation, almost twice that level in women of reproductive age. Typical levels of iron in the diet are approximately 6 mg per 1000 kcal, but the efficiency of dietary iron absorption is relatively low, particularly in diets containing high amounts of inhibitory substances, such as phytates and polyphenols.1 Because endogenous iron losses are minimal,2 the primary focal point of iron homeostasis is the control of the efficiency of intestinal iron absorption. Under conditions of iron deficiency or high iron demand, the efficiency of iron absorption by the intestine increases. This homeostatic response allows the restoration of tissue iron stores and provision of iron for hemoglobin synthesis and other cellular functions. Nevertheless, the combination of high physiologic iron demand and low iron availability in many diets all too often exceeds the ability of the intestinal regulatory capacity to fully compensate. It is perhaps not surprising then that iron deficiency is the most common micronutrient deficiency in the world, affecting billions of people. Iron deficiency leads to impaired function of various systems in the body, including insidious cognitive, immune, and muscle dysfunction, in addition to the well known hematologic signs of iron-deficiency anemia that are caused by an inability to produce the iron-containing, oxygen-transporting protein, hemoglobin.
At the other end of the iron balance spectrum is iron overload. This condition can stem from inappropriately high iron intake, dysregulation of intestinal iron absorption, or excessive blood transfusions that can occur in the treatment of certain blood disorders, such as thalassemia. The most common cause of acute poisoning in children in the United States is due to acute gastrointestinal exposure to high amounts of iron from eating iron supplements. These exposures are difficult to treat and can be fatal. Mandated improved packaging of these iron-- containing supplements by manufacturing them with childproof caps is an important step in the prevention of this form of child poisoning. In addition, continued proper storage of iron supplements, including prenatal supplements, by the consumer is imperative to prevent this problem. Beyond acute poisoning events, however, other more chronic situations of frank iron overload resulting from ingestion of high amounts of iron have been reported, such as iron overload caused by long-term consumption of iron-contaminated beer as seen in some areas of Africa.3 Chronic iron overload develops because of the lack of normal homeostatic mechanisms for ridding the body of excess iron. Normal variations in body iron flux can be easily handled by temporary storage on transferrin, a circulating iron-binding protein that delivers iron throughout the body and is normally only onequarter saturated. When iron is in excess, the body tries to minimize the potentially toxic effects by sequestering excess iron in the iron storage protein ferritin. Normally, essentially no free non-transferrin-bound iron circulates in the plasma. Too much can be dangerous because it can exceed the capacity of transferrin to bind all the circulating iron. The sequestering of iron on protein molecules is important because iron can generate potentially damaging free radicals via participation in Haber-Weiss chemical reactions. These chemical reactions generate chemically reactive hydroxyl radicals via the interaction of superoxide anion with ferric (Fe^sup +3^) iron to generate reduced ferrous (Fe^sup +2^) iron. Ferrous iron can then react with hydrogen peroxide, produced during cellular metabolism, to form highly reactive hydroxyl radicals that can cause cellular and tissue damage.
More moderate elevations of body iron stores, reflected by elevated serum ferritin concentrations, can develop throughout the normal course of aging in otherwise healthy individuals. It was recently reported that approximately 10% of elderly men and women have high serum ferritin, whereas approximately 3% have ferritin levels indicative of depleted iron stores and only approximately 1% had iron-deficiency anemia.4 Because high serum ferritin has been associated in some studies with an increased risk of heart disease,5 diabetes,6 and colon cancer,7 more attention needs to be focused on the possible health consequences of moderate iron burdens.
Finally, genetic causes of iron overload also exist. Hereditary hemochromatosis is characterized by elevated serum iron, transferrin saturation, and ferritin, and elevated total-body iron burden. Clinically, excessive iron burdens in patients with hemochromatosis can result in darkening of the skin, arrhythmias, loss of body hair, and impotence in men. In addition, pathologic changes can develop, including fibrosis of the liver, abnormalities in liver function tests, and raised blood sugar levels. The primary cause of iron overload in hereditary hemochromatosis is inappropriately high intestinal iron absorption efficiency in the face of increased body iron burden. In simplified terms, in regards to iron absorption efficiency, the intestine of the person with hereditary hemochromatosis acts like the intestine of a person with iron-deficiency anemia.
But, why do people with hereditary hemochromatosis absorb so much iron when they clearly don't need it? Additional insights into the pathology of hereditary hemochromatosis could provide clues to the normal molecular control of iron absorption. An important breakthrough in the understanding of hereditary hemochromatosis came in 1996 with the publication of a landmark paper by Feder and colleagues8 proclaiming the discovery of the gene mutation (C282Y HFE) that is the cause of hereditary hemochromatosis in the vast majority of cases. In the United States, approximately five people in 1000 are homozygous for a C282Y mutation in the HFE gene, and approximately 10% of the Caucasian population in the United States is heterozygous carriers of the HFE mutation. But, before we can explain the molecular workings of HFE in terms of cellular iron metabolism, we must first understand some additional details about the amazing intricacies of cellular iron nutrition.
Normally, ferrous iron exiting the enterocyte is oxidized to ferric iron and picked up in the circulation by the iron-binding protein transferrin, which in turn delivers iron throughout the body. The transport of iron out of the enterocyte is influenced by copper status, which regulates the activity of hephaestin-a novel copper-- containing ceruloplasmin-like ferroxidase found on the basolateral membrane of the enterocyte-and governs the exit of iron from the enterocyte. The iron requirement of each cell is provided dynamically by iron derived from circulating diferric transferrin. Each cell in the body can act as a separate unit and exert decentralized control over the uptake of iron from the circulation. Controlling the number of transferrin receptors on the cell surface regulates this decentralized control of cellular iron uptake. The synthesis of transferrin receptors is regulated by a unique post-transcriptional mechanism that operates by controlling the degradation of transferrin receptor mRNA and therefore the size of the available pool of transferrin receptor mRNA in the cell. An in-depth discussion of the interesting details of this post-transcriptionally regulatory mechanism of cellular iron homeostasis can be found in various excellent reviews of the topic.9,10 A simplified version of these complex cellular events is as follows.
Cellular iron demand is sensed by an iron-binding cytosolic protein (iron regulatory protein, IRP), which acts as either an iron-binding protein or as an RNA-binding protein. There is a specific 28-nucleotide binding site for the IRP found in the non-translated region on certain messenger RNA molecules that code for proteins involved in iron metabolism. It is important to note that the affinity of IRP for its recognition site on mRNA is determined by the iron status of IRP, although other factors are also important.10 The IRP acts effectively as an RNA-binding protein when it is devoid of iron. This iron-dependent RNA-binding characteristic is the chemical basis of IRP as an effective cellular iron sensor, and permits the IRP molecule to act as a molecular switch controlling the level of proteins involved in cellular iron homeostasis.
The cellular iron homeostatic system works as follows. When the cellular iron pool is low, the iron content of IRP is low, which increases the affinity of IRP for its recognition site on the mRNA and allows IRP to act as an mRNA-binding protein. At this point, things get a bit more complicated. The complication-and wonderful elegance of this molecular control mechanism-is that the ultimate effect of IRP binding to a given mRNA on cellular iron metabolism now depends on the location of this mRNA stem-loop recognition structure (the socalled iron regulatory element [IRE]) on the mRNA molecule. Some mRNAs have the IRE in the 5'-end of the RNA, whereas some others have the IRE motif placed at the 3'-end of the mRNA. As it turns out, this makes a big difference and provides an important coordination to the regulatory control process. Namely, the binding of IRP to an IRE sequence that is in the 3'-end of the mRNA acts to slow the degradation rate of that mRNA. This action leads to an increase in the size of the mRNA pool available for translation, and thereby augments the level of the protein in the cell. By contrast, if the IRE is coded in a given gene in the 5'-end of the mRNA, then the binding of the IRP to the IRE when cellular iron stores are low results in an obstruction to the introduction of that mRNA into the ribosomal translational machinery, and therein prevents the synthesis of the protein. Thus, through the singular mechanism of the IRP-IRE association reciprocal iron-dependent control can be achieved over a set of proteins that are involved in cellular iron metabolism. A specific example of these effects is provided below.
When cellular iron levels are low, this is "sensed" by IRP and is reflected in its increased ability to bind to the IRE in the 3'-end of the transferrin receptor mRNA. IRP binding in this case stabilizes the transferrin receptor mRNA allowing an increase in the cytosolic levels of transferrin receptor mRNA, which causes an increased synthesis of transferrin receptor protein. More transferrin receptor protein is then available for insertion on the cell surface, imparting a greater functional capacity of the cell to internalize circulating diferric transferrin and its iron cargo, and cellular iron levels begin to rise. Concomitantly, opposite effects are occurring with ferritin. Ferritin is a large protein that self-assembles in the cytosol into a spherical protein from many smaller ferritin protein subunits. A ferritin molecule has a large capacity to sequester available cellular iron within its core. Because ferritin subunits have their IRE located on the 5'-end of the mRNA, the binding of IRP to these IREs decreases the synthesis of ferritin protein subunits by blocking translation of the mRNA. Thus, the net physiologic affect of the molecular actions of iron-poor IRP is that more iron is taken up by the cell from circulating diferric transferrin and this iron becomes available in the intracellular iron pool for various cell functions, such as the synthesis of hemoglobin found in developing red blood cells. The reverse of this cellular iron regulatory loop occurs when free intracellular iron levels increase. In this case, the iron-laden IRP molecule has lower affinity for RNA binding and more readily dissociates from the IRE on both ferritin subunit mRNA and transferrin receptor mRNA. The net cellular effect of this action is that more ferritin protein and less transferrin receptor protein are synthesized. Overall, the rate of iron uptake into the cell through the transferrin receptor-mediated membrane portal is decreased and the elevated free iron in the cytosol is lowered to normal by being sequestered into an increased number of cytosolic ferritin molecules. The cell is thus protected from the potentially damaging effects of elevated free iron concentrations.
The cloning of the HFE gene8 was a significant development not only in the development of a genetic marker of hemochromatosis risk, but also by providing a novel protein that was apparently involved in the regulation of transport of iron across the enterocyte.11 In the past several years, a series of papers have appeared from William Sly's laboratory at the Saint Louis University School of Medicine that have provided a greater understanding of the role of the HFE protein in the maintenance of iron homeostasis.11-15 A recent paper from this group16 has provided insightful observations on the regulation of cellular transferrin-mediated iron uptake by HFE, the protein defective in hereditary hemochromatosis. It had been previously demonstrated that the C282Y HFE mutation disrupts a disulfide bond in the alpha3 domain of the HFE protein, and the consequence of this disruption is that the mutated HFE does not associate with its normal cellular partner, the beta2-microglobulin protein.17 This lack of protein partnering prevents the normal cell surface expression of HFE. Previous studies did not however reveal how HFE functions to regulate iron absorption, and why the mutation in HFE results in increased iron absorption. These insights were hinted at by the previous report that HFE interacts with the transferrin receptor. However, making physiologic sense of the functional role of the interaction of HFE with transferrin receptor has been difficult because previous cell culture studies where HFE levels were increased indicated that higher HFE protein levels resulted in the development of an iron deficiency-type phenotype in these cells. In other words, when HFE was elevated, ferritin levels in the cell declined, and transferrin receptor and iron regulatory protein activity went up-all indications that the cellular iron level had been lowered. This was a curious finding because in hereditary hemochromatosis HFE levels are down, and the enterocyte displays characteristics of the low-iron condition. In other words, because lIFE and enterocyte iron status is low in hereditary hemochromatosis, one would expect that in transfected cells overexpressing HFE the cell would become loaded with iron.
Waheed and colleagues16 speculated that the level of endogenous beta-2 microglobulin might influence the apparently anomalous findings in cell culture studies. Therefore, they investigated what effect overexpressing both HFE and beta-2 microglobulin had on cellular iron status versus expressing HFE alone. They chose CHO (Chinese hamster ovary) cells as their experimental cell culture model. In these cells, overexpressing HFE alone resulted in the lack of maturation of the expressed protein into a higher molecular weight form and the rapid degradation of HFE. In addition, these cells displayed a low-iron cellular phenotype with increased uptake of transferrin-bound iron, as other groups had noted in HeLa cells transfected with HFE. By contrast, however, overexpressing both HFE and beta-2 microglobulin in CHO cells reversed this phenotype. Cells expressing both HFE and beta-2 microglobulin demonstrated an increased transferrin-bound iron uptake, and high ferrifin levels-a picture expected if cellular iron stores had been increased. These observations suggest a model of cellular iron control wherein HFE normally is found in association with beta-2 microglobulin and functions to augment the uptake of iron into the cell via a transferrin receptor-mediated route.
But, how exactly does the HFE-beta-2 microglobulin protein complex influence the iron status of the cell? To answer this question, Waheed et al.16 addressed several possibilities including a change in transferrin receptor protein levels in the cell, altered affinity of the transferrin receptor for transferrin, differences in internalization rate of the transferrin receptor-transferrin complex during endocytosis, as well as an augmented recycling rate of endocytosed transferrin receptor back to the cell surface. As it turned out, the transferrin receptor concentration in cells overexpressing the HFE-beta-2 microglobulin complex was actually somewhat lower than in the control cells; there was no effect of HFE-beta-2 microglobulin expression on the affinity of transferrin for the transferrin receptor or the internalization rate of the transferrin receptor complex. What was different in the CHO cells expressing HFE and beta-2 microglobulin was the surface binding capacity of transferrin, which could explain the increased uptake of transferrin-bound iron in CHO cells overexpressing HFE and beta-2 microglobulin. Interestingly, the greater availability of transferrin receptor on the cell surface was due to increased recycling of the endocytosed transferrin-transferrin receptor complex in the transfected CHO cells.
Thus, collectively, studies of the molecular function of HFE have revealed important new information about the likely control of cellular iron status of the enterocyte and intestinal iron absorption. Under normal conditions, it appears that HFE acting in association with beta-2 microglobulin and transferrin receptor governs the rate of iron uptake into the enterocyte by increasing the rate of recycling of the transferrin receptor-transferrin complex that feeds circulating diferric transferrin-bound iron to cells and thereby controls cellular iron stores. The amount of cellular iron in turn regulates the level of expression of proteins that control intestinal iron absorption, such as the iron import transporter on the apical membrane and the iron export transporter on the basolateral membrane.18 In the enterocyte, low iron status stimulates an increase in the expression of both membrane transporters19,20 leading to an increase in the rate of intestinal iron absorption. By contrast, when cellular iron accumulates and enterocyte iron stores are high, the expression of the membrane iron transporters declines and intestinal iron absorption decreases.
In hereditary hemochromatosis, the cysteine-to-tyrosine amino acid substitution caused by the C282Y HFE mutation disrupts the binding of HFE to beta-2 microglobulin leading to the premature degradation of HFE and reduction in its cell surface expression.17 As a consequence, less HFE is available for association with transferrin receptor, turnover of the transferrin receptor-transferrin complex decreases, and transferrin receptor-- mediated iron uptake from circulating transferrin is decreased. This leads to relative iron starvation in the enterocyte leading paradoxically to the development of an "anemic" enterocyte phenotype in the midst of bountiful body iron stores. Thus, despite ever-increasing stores of body iron, the inappropriately low iron status of the hereditary hemochromatosis enterocyte continues to drive the hyper-absorption of dietary iron. The apparent persistence of this iron-starved state in the enterocyte leads eventually to the development of significant systemic pathology from iron toxicity if phlebotomy therapy is not initiated and the body's compensatory iron storage capacity becomes overwhelmed.
1. Hallberg L. Bioavailability of dietary iron in man. Annu Rev Nutr 1981;1:123-47
2. Green R, Charlton R, Seftel H, Bothwell T. Body iron excretion in man. Am J Med 1968;45:336-53
3. Gordeuk VR, Boyd RD, Brittenham GM. Dietary iron overload persists in rural sub-Saharan Africa. Lancet 1986;1:1310-3
4. Fleming DJ, Jacques PF, Tucker KL, et al. Iron status of the free-living, elderly Framingham Heart Study cohort: an iron-replete population with a high prevalence of elevated iron stores. Am J Clin Nutr 2001;73:638-46
5. Salonen JT, Nyyssonen K, Korpela H, et al. High stored iron levels are associated with excess risk of myocardial infarction in eastern Finnish men. Circulation 1992;86:803-11
6. Ford ES, Cogswell ME. Diabetes and serum ferritin concentration among U.S. adults. Diabetes Care 1999;22:1978-83
7. Nelson RL, Davis FG, Sutter E, et al. Body iron stores and risk of colonic neoplasia. J Natl Cancer Inst 1994;86:455-60
8. Feder JN, Gnirke A, Thomas W, et al. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat Genet 1996;13:399-408
9. Eisenstein RS. Iron regulatory proteins and the mo
lecular control of mammalian iron metabolism. Annu Rev Nutr 2000;20:627-62
10. Theil EC, Eisenstein RS. Combinatorial mRNA regulation: iron regulatory proteins and iso-iron-responsive elements (Iso-IREs). J Biol Chem 2000; 275:40659-62
11. Zhou XY, Tomatsu S, Fleming RE, et al. HFE gene knockout produces mouse model of hereditary hemochromatosis. Proc Natl Acad Sci U S A 1998; 95:2492-7
12. Parkkila S, Waheed A, Britton RS, et al. Association of the transferrin receptor in human placenta with HFE, the protein defective in hereditary hemochromatosis. Proc Natl Acad Sci U S A 1997;94:13198-202
13. Waheed A, Parkkila S, Zhou XY, et al. Hereditary hemochromatosis: effects of C282Y and H63D mutations on association with beta2-microglobulin, intracellular processing, and cell surface expression of the HFE protein in COS-7 cells. Proc Natl Acad Sci U S A 1997;94:12384-9
14. Griffiths WJ, Sly WS, Cox TM. Intestinal iron uptake determined by divalent metal transporter is enhanced in HFE-deficient mice with hemochromatosis. Gastroenterology 2001;120:1420-9
15. Waheed A, Parkkila S, Saarnio J, et al. Association of HFE protein with transferrin receptor in crypt enterocytes of human duodenum. Proc Natl Acad Sci U S A 1999;96:1579-84
16. Waheed A, Grubb JH, Zhou XY, et al. Regulation of transferrin-mediated iron uptake by HFE, the protein defective in hereditary hemochromatosis. Proc Natl Acad Sci U S A 2002;99:3117-22
17. Feder JN, Tsuchihashi Z, Irrinki A, et al. The hemochromatosis founder mutation in HLA-H disrupts beta-2 microglobulin interaction and cell surface expression. J Biol Chem 1997;272:14025-8
18. Wessling-Resnick M. Iron transport. Annu Rev Nutr 2000;20:129-51
19. Gunshin H, Mackenzie B, Berger UV, et al. Cloning and characterization of a mammalian proton-coupled metal-ion transporter. Nature 1997;388:482-8
20. McKie AT, Marciani P, Rolfs A, et al. A novel duodenal iron-regulated transporter, IREG1, implicated in the basolateral transfer of iron to the circulation. Mol Cell 2000;5:299-309
This review was prepared by Richard J Wood, Ph.D., Chief, Mineral Bioavailability Laboratory, Jean Mayer USDA Human Nutrition Research Center on Aging at Tufts University, 711 Washington Street, Boston, MA 02111, USA,
Copyright International Life Sciences Institute and Nutrition Foundation May 2002
Provided by ProQuest Information and Learning Company. All rights Reserved