Study objectives: Different vasodilators and different routes of application are used for the treatment of primary pulmonary hypertension (PPH). Recently, sildenafil, a phosphodiesterase-V inhibitor, has been shown to have beneficial hemodynamic effects in PPH. However, the hemodynamic effects of sildenafil have not been characterized and compared to other vasodilators such as inhaled nitric oxide (iNO) or iloprost in PPH in the same group of patients.
Study design: We investigated prospectively 10 consecutive patients with PPH using iNO, iloprost aerosol, and oral sildenafil to test acute hemodynamic response during right-heart catheterization.
Results: iNO, iloprost aerosol, and sildenafil caused a significant fall of mean pulmonary artery pressure and pulmonary vascular resistance (PVR) [p < 0.05]. Correspondingly, cardiac output and mixed venous saturation increased slightly in all groups. Systemic arterial pressure and vascular resistance were mainly unaltered. Using a PVR reduction of [greater than or equal to] 20% to define a significant response, 7 of 10 patients were responders to iloprost aerosol, whereas 4 of 10 patients responded to iNO and oral sildenafil. Improvement of oxygenation as indicated by an increase of arterial oxygen tension was observed with iloprost aerosol (p < 0.01).
Conclusion: All of the three substances, iNO, iloprost aerosol, and oral sildenafil, significantly improved pulmonary hemodynamics in patients with PPH. The most prominent hemodynamic effects and improvement of oxygenation were observed with iloprost aerosol.
Key words: hypertension; iloprost; medical subject heading; nitric oxide; pulmonary; sildenafil
Abbreviations: CCB = calcium-channel blocker; cGMP = cyclic guanosine monophosphate; CI = cardiac index; CO = cardiac output; HR = heart rate; iNO = inhaled nitric oxide; NYHA = New York Heart Association; PAP = pulmonal artery, pressure; PAPmean = mean pulmonary artery pressure; PCWP = pulmonal capillary wedge pressure; PHI = primary pulmonary hypertension; PVR = pulmonary vascular resistance; RAP = right atrial pressure; SAP = systemic arterial pressure; SAPmean = mean systemic arterial pressure; Sv[O.sub.2] = mixed venous oxygen saturation; SVR = systemic vascular resistance
**********
Primary pulmonary hypertension (PPH) is a rare disease leading to severe limitations of functional status, and a median survival of 2.8 years (1) without appropriate therapies. Preferentially, young to middle-aged women are affected, although the disease is diagnosed at any age and sex. (2) Features of PPH include vasoconstriction of varying degrees, medial and intimal hypertrophy, (3) and in situ thrombosis. (4) The common medical therapy includes anticoagulation (4,5) and diuretics. Additionally, different vasodilators have been introduced based on the premise that antagonism of vasoconstriction could be of value in the medical therapy. (6)
Different drugs that have the ability to selectively dilate pulmonary vessels are used in the evaluation and treatment of PPH. (6,7) Additionally, antiproliferative properties could be of value in patients with PPH, but there are no controlled studies supporting this theory. However, some of these vasodilators are applied systemically, while others are administered locally as an aerosol or gas. Oral calcium-channel blockers (CCBs) may be used in patients who show significant pulmonary vascular resistance (PVR) reduction in acute hemodynamic testing. (8) In this context, inhaled nitric oxide (iNO) is a pulmonary selective vasodilator that allows prediction of hemodynamic response to CCBs in PPH. (9,10) Inhalation of iloprost, a stable prostacyclin (epoprostenol) analog, has been demonstrated to improve hemodynamics and exercise capacity in patients with PPH. (11-14) However, frequent inhalations (6 to 12/d) of iloprost are required due to the short duration of the hemodynamic effect, lasting approximately 20 to 60 min after inhalation. (15,16) Continuous IV infusion of prostacyclin has proven beneficial effects on hemodynamics, exercise capacity, and survival in patients with PPH. (17-20) However, continuous IV prostacyclin therapy is hampered by line infections, tachyphylaxis, and systemic side effects due to the lack of pulmonary selectivity.
Sildenafil is a selective phosphodiesterase-V inhibitor that leads to stabilization of cyclic guanosine monophosphate (cGMP). cGMP, a second messenger of nitric oxide (NO), promotes vasodilation in pulmonary vessels. (21) Oral application of the cGMP-specific phosphodiesterase-inhibitor sildenafil has been shown to have beneficial effects in patients with PPH, (22,23) even during application of iNO. (24,25) Moreover, sildenafil has been demonstrated to exert additive effects on pulmonary hemodynamics, when applied with inhaled iloprost. (26,27) Thus, oral application of sildenafil may have clinical relevance in patients with PPH.
The acute hemodynamic effects of oral sildenafil have not yet been characterized and compared to the pulmonary vasodilators iNO and iloprost aerosol in patients with PPH. The aim of our study was to evaluate the hemodynamic effects of oral sildenafil in patients with PPH in comparison to the pulmonary selective vasodilatory profiles of iNO and iloprost aerosol.
MATERIALS AND METHODS
Ten consecutive patients with PPH who were scheduled for routine right-heart catheterization were included in our study. Exclusion criteria were secondary pulmonary hypertension, pregnancy, hypotension (systolic BP < 90 mm Hg), or any other significant systemic disease. Underlying causes for pulmonary hypertension were excluded according to the criteria established during the World Health Organization conference of Evian 1998. (28) Vasodilative treatment for pulmonary hypertension included CCBs in one patient, CCBs plus iloprost aerosol in two patients, iloprost aerosol in four patients, and no specific therapy in three patients. CCBs were discontinued 36 to 48 h prior to right-heart catheterization. Treatment with iloprost aerosol was discontinued at least 12 h prior to right-heart catheterization. The study protocol was approved by the local ethics committee. Written informed consent was obtained from every patient.
Right-Heart Catheterization:
A Swan-Ganz catheter (Criti-Cath; Becton Dickinson; Temse, Belgium) and an arterial catheter (Cordis; Johnson & Johnson; Miami, FL) were inserted into the right femoral vein and artery, respectively. Hemodynamic measurements were performed in recumbent position. Continuous hemodynamic monitoring included heart rate (HR), systemic arterial pressure (SAP), pulmonary artery pressure (PAP), and transcutaneous arterial oxygen saturation. Arterial and mixed venous oxygen saturation (Sv[O.sub.2]) blood samples were obtained to measure oxygen saturation (Hemoximeter; Radiometer; Copenhagen, Denmark). Additionally, blood gas analysis was performed in arterial blood samples (ABL 520; Radiometer).
Pulmonary capillary wedge pressure (PCWP) and right atrial pressure (RAP) were measured during each test. Cardiac output (CO) was also obtained during the acute vasoreactivity test of each agent, using triplicate measurements with the thermodilution method (Cardiac Output Computer; Edwards Laboratories; Santa Ana, CA). Cardiac index (CI), PVR, and systemic vascular resistance (SVR) were calculated using standard formulas.
Vasodilator Test
A positive response to acute vasodilator challenge was defined as a reduction in PVR and/or mean PAP (PAPmean) of at least 20%. (9,10,28) Initial baseline values were obtained after a steady-state period of 20 min and additionally after each vasodilator test when all variables had returned to preinhalation levels and remained constant for at least 5 min.
The vasodilators were used in a nonrandomized fashion in the order of iNO, iloprost, and sildenafil. iNO was administered at a dose of 40 ppm, as measured in the expiratory air (NO-Monitor; Micro Medical; Kent, UK). (15) The maximum effect was recorded after 5 min of inhalation.
Iloprost was aerosolized with a jet nebulizer (Ilo-Neb; NebuTec; Elsenfeld, Germany). Fifty micrograms of iloprost were diluted in 4.5 mL of saline solution (NaCl 0.9%; Braun; Melsungen, Germany). One milliliter and 0.5 to 2 mL of this solution were aerosolized over 10 to 15 min, presuming a nebulized dose of 15 to 20 [micro]g. Hemodynamic variables were measured immediately after stopping the iloprost inhalation and 15 to 60 min after the end of the aerosolization period until all parameters had returned to baseline levels.
Oral sildenafil was administered in an initial dose of 50 mg, followed by another 50 mg after 30 min. Hemodynamic parameters were measured 30 min after each dose.
Statistical Analysis
All values are presented as mean [+ or -] SEM. For comparison of test effects, a Students two-sided, paired t test was used; p < 0.05 was considered statistically significant. Data obtained during each vasodilator test (PAPmean, PVR, CO, CI, HB, RAP, mean SAP [SAPmean], systemic vascular resistance [SVR], Pa[O.sub.2], and Sv[O.sub.2]) were compared with the preceding baseline and with results obtained with each of the other vasodilators.
RESULTS
Patient Characteristics
We included seven women and three men (age range, 33 to 59 years). New York Heart Association (NYHA) class was II (n = 4), III (n = 5), or IV (n = 1). The 6-min walk distance measured 250 to 590 m. NYHA class and duration of the disease did not correlate with the degree of pulmonary hypertension. The time to diagnosis was 6 months to 5 years. Patient characteristics are shown in Table 1.
Baselines and Acute Hemodynamic Testing
Initial baseline hemodynamics are shown in Table 2. All patients had significant precapillary pulmonary hypertension. The initial baseline and pretest baselines 2 and 3 showed minor (< 2%) variations, but this did not reach significance.
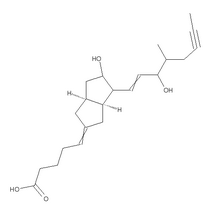
Acute Hemodynamic Effects of iNO
Inhalation of NO produced a decline in PAPmean from 55.2 [+ or -] 3.2 to 47.8 [+ or -] 2.7 mm Hg (p < 0.05). This was paralleled by a slight increase in CO from 3.65 [+ or -] 0.4 to 3.73 [+ or -] 0.5 L/min (p > 0.05), resulting in a reduction of PVR from 1099.1 [+ or -] 128.7 to 959.5 [+ or -] 132.8 dyne**s**[cm.sup.-5] (p < 0.01) [Tables 1, 2; Fig 1]. Pa[O.sub.2], SAPmean, SVR, HR, PCWP, RAP, and Sv[O.sub.2] showed no major changes (Table 2).
[FIGURE 1 OMITTED]
Four of 10 patients were iNO responders based on the criterion of a PVR reduction of [greater than or equal to] 20% (Table 1). Three of 10 patients were responders based on reduction in PAPmean of [greater than or equal to] 20%. All PAPmean responders were also PVR responders.
Acute Hemodynamic Effects of Iloprost Aerosol
Administration of iloprost caused a reduction in PAPmean from 53.4 [+ or -] 3.5 to 44.2 [+ or -] 3.2 mm Hg (p < 0.01; Tables 1, 2; Fig 1). CO increased from 3.43 [+ or -] 0.4 to 3.65 [+ or -] 0.4 L/min (p > 0.05). This resulted in an overall fall of PVR from 1,114.3 [+ or -] 134.6 to 743.84 [+ or -] 138 dyne**s**[cm.sup.-5] (p < 0.01). Pa[O.sub.2] increased from 72.7 [+ or -] 2.7 to 88.4 [+ or -] 4.3 mm Hg (p < 0.01). SAPmean, SVR, PCWP, RAP, HR, and Sv[O.sub.2] did not change significantly.
When the response criteria of a PVR reduction of [greater than or equal to] 20% was applied, 7 of 10 patients were responders to iloprost aerosol (Table 1, Fig 1). According to the reduction of PAPmean of [greater than or equal to] 20%, 5 of 10 patients were responders. All PAPmean responders were also PVR responders.
Acute Hemodynamic Effects of Oral Sildenafil
The cumulative dose of 100 mg of sildenafil caused PAPmean to decline from 52.7 [+ or -] 3.9 to 46.8 [+ or -] 3.6 mm Hg (p < 0.01), CO increased from 3.37 [+ or -] 0.4 to 3.49 [+ or -] 0.3 L/min (p > 0.05), and PVR dropped from 1,119.8 [+ or -] 141.9 to 951.8 [+ or -] 135.4 dyne**s**[cm.sup.-5] (p < 0.01; Tables 1, 2; Fig 1). Pa[O.sub.2], SAPmean, SVR, HR, RAP, PCWP, and Sv[O.sub.2] were mainly unchanged.
Sildenafil resulted in a significant PVR decrease ([greater than or equal to] 20%) in 4 of 10 patients (Table 1, Fig 1) and a reduction of PAPmean ([greater than or equal to] 20%) in 3 of 10 patients. All PAPmean responders were also PVR responders. Three of four patients were responders to 50 mg of sildenafil, and one patient showed a PVR reduction only after the total dose of 100 mg.
Differential Effects of iNO, Iloprost Aerosol, and Oral Sildenafil
Comparison of the acute hemodynamic effects of oral sildenafil with those of iNO revealed a comparable overall reduction in PAPmean and PVR (Tables 1, 2; Fig 1). However, iNO resulted in a paradoxical increase in PAPmean and PVR in two patients, while no patient had a significant increase in PAPmean or PVR with sildenafil (Fig 1). Nevertheless, 40% of patients had a significant PVR reduction of [greater than or equal to] 20% with iNO and with sildenafil. Interestingly, all patients with a positive iNO response also were responders to oral sildenafil.
Although not statistically significant, comparison of the acute hemodynamics after application of oral sildenafil and iloprost aerosol showed a more pronounced fall in PAPmean and increase in CO resulting in a more prominent PVR reduction with iloprost aerosol. A significantly greater response was observed with the use of iloprost aerosol (Table 2) when compared to iNO. Reductions of PVR (p < 0.05) and PAPmean (p < 0.01) were less prominent with iNO, whereas the other parameters did not differ significantly.
The PVR response rate was higher (70%) with iloprost aerosol than with sildenafil or iNO (each 40%). Of the iloprost responders, 57% were also sildenafil and iNO responders. Comparing the influence of different pulmonary vasodilators on arterial oxygen pressure as a possible parameter of ventilation-perfusion mismatch revealed a significant increase of Pa[O.sub.2] after iloprost inhalation and was not significantly affected with iNO or sildenafil. No significant effects on PCWP, SAPmean, and SVR were noted in any of the test substances.
DISCUSSION
In our observational study, we evaluated and compared the acute hemodynamic effects of iNO, iloprost aerosol, and oral sildenafil during right-heart catheterization in patients with PPH. All substances caused significant reduction in PAPmean and PVR in this group of patients. The vasodilative response was restricted to the pulmonary circulation as SAP and SVR showed no significant change. At the doses tested, iloprost aerosol was a more potent pulmonary vasodilator than iNO and sildenafil. Iloprost aerosol caused a positive response (PVR reduction [greater than or equal to] 20%) in 7 of 10 patients, whereas iNO and sildenafil were tested positive in only 4 of 10 patients. Additionally, iloprost aerosol had a positive effect on oxygenation, as a parameter of ventilation-perfusion mismatch after the inhalation. Improvement of arterial oxygen saturation has been previously described during inhalation of iloprost in pulmonary hypertension. (15,16) Preferential distribution of the iloprost aerosol to well-ventilated lung areas and a more homogenous ventilation-perfusion relationship have been suggested as potential mechanisms. An increase of CO may also have contributed to improved oxygenation.
Acute hemodynamic vasodilator tests have repeatedly been used to describe hemodynamic profiles of patients with PPH, (7) and to characterize vasodilating agents. (9,10,15,16,29-31) Even the acute effects of iloprost aerosol have been compared to iNO and sildenafil in previous studies. (26,27) A single study compared IV prostacyclin to iNO and oral sildenafil in pulmonary hypertensive patients with underlying lung fibrosis. (32) None of these investigations differentiated all three acute vasodilators in the same group of patients with PPH. Both iNO and iloprost aerosol are known potent pulmonary vasodilators. (12,13,15,16,30) These substances induce acute vasodilative responses within minutes of inhalation. The vasodilatory effect of iNO is short acting and levels off within 2 to 5 min after discontinuation. (16,30) iNO is used as test substance in pulmonary hypertension, as it has been demonstrated to be predictive with regard to the effectiveness of treatment with CCBs. According to these investigations, patients who show a decrease of > 20% of PVR and PAPmean during NO inhalation can be treated successfully with CCBs. (9,10,31) Inhalation of iloprost is known to cause a more prolonged pulmonary vasodilation, which usually ends 20 to 60 min after discontinuing aerosolization. (15,16) Although defining response according to reduction in PVR of [greater than or equal to] 20% without changes in PAP is controversial, (6) this criterion has been described previously (10) and may be of clinical relevance for the individual patient. An increase in CO that is not accompanied by a further elevation of PAP could alleviate symptoms and is generally accepted as a valuable tool for the difficult task of selecting an effective therapy for an individual patient. (9,10,13,29)
Pulmonary selectivity of the vasodilatory effect of iNO and iloprost aerosol is explained by the inhalation route of application. (13,15,16,30) Additionally, NO rapidly binds to hemoglobin, thus limiting spillover and systemic side effects. Interestingly, oral application of sildenafil in our study also showed a hemodynamic profile comparable to iNO. Selective pulmonary vasodilation without significant systemic hypotension was also achieved with systemic application of sildenafil. We observed only a minor increase of CO, which probably would not explain the maintenance of systemic BP. The effect of selective vasodilation may be due to the different distribution of phosphodiesterase-V in different vascular beds, phosphodiesterase-V is expressed in a relative high amount in the lung vasculature (33,34) and the corpus cavernosum. (35) The latter explains the effects of the phosphodiesterase-V inhibitor sildenafil in erectile dysfunction (35) without major hemodynamic side effects in healthy subjects. (36) High levels of phosphodiesterase-V expression in pulmonary arteries provides a good explanation for the pulmonary selective vasodilative property of sildenafil as observed in our study and reported by other investigators in patients with pulmonary hypertension. (21-27)
In our study, we tested doses of 50 mg and 100 mg of oral sildenafil. The recommended dose range for the therapy of erectile dysfunction is 25 to 100 mg. Data have been published that describe a reduction of systemic BP with an oral dose of 100 mg in healthy men. (36) In patients with severe PPH, doses of 25 mg (25) and 50 mg (27) of sildenafil caused substantial effects on pulmonary circulation. A single case report (23) in a young man with PPH reports a starting dose of 50 mg qd and was titrated up to 500 mg/d. Reviewing these data, we found 50 to 100 mg of oral sildenafil a safe test dose to produce considerable positive effects on pulmonary hemodynamics without significant systemic side effects in patients with PPH. A limitation of our study is that we did not generate complete dose-response curves; we cannot therefore exclude that hemodynamic effects would have been observed with lower or higher doses. Another limitation of our investigation is that only three patients did not receive vasodilative treatment before entering the study. Although patients had a therapy-free interval of 36 to 38 h of CCBs and 12 h of iloprost, respectively, we cannot securely exclude influences of vasodilative therapy on the results. However, we found no significant difference in hemodynamic response between the treatment groups. Based on the strategy to apply short-acting before long-acting substances as reported earlier, (9,15,16) we selected the test substances in a nonrandomized fashion. The influence of the preceding vasodilator on the following test substance should be minimized in this setting.
An additional finding in our study was that every patient who had a PVR reduction of at least 9.0% during iNO testing also had a positive response to sildenafil testing. Only four of seven patients (57%) who showed a positive PVR response to iloprost aerosol were classified as sildenafil responders. Interestingly, we observed a paradoxical increase in PAPmean and PVR in two patients (PVR increased by 10% and 22%, respectively) during iNO application. The mechanism of this phenomenon has not been clarified yet, but NO-induced paradoxical increases in PAP in 23 to 29% of patients, or PVR in 17 to 31% of patients, have been reported before. (15,31) In our study, paradoxical reaction to NO did not lead to clinical symptoms nor was statistically significant; however, potentially harmful consequences during acute vasodilator testing must be taken into consideration.
One possible explanation for the different hemodynamic effects of sildenafil, iNO, and iloprost aerosol is the production of different second messengers that are essential for the vasodilatory effects. Prostacyclin and its stable analog iloprost activate adenylate cyclase that leads to production of cyclic adenosine monophosphate, resulting in relaxation of vascular smooth-muscle cells. The vasorelaxant effect of NO is known to result at least in part from activation of soluble guanylate cyclase that leads to an increase of the second messenger cGMP in the vascular smooth-muscle cells. (37-39) However, different phosphodiesterases in the lung that hydrolyze cGMP and cyclic adenosine monophosphate may terminate their vasodilatory effects. (33) Sildenafil leads to increased cGMP content via inhibition of phosphodiesterase-V. The introduction of different phosphodiesterase inhibitors in experimental pulmonary hypertension was based on the consideration that inhibiting degradation of second messengers in the pulmonary vasculature may lead to prolonged vasodilation. (40,41) This was also the rationale for using sildenafil as a pulmonary vasodilator in some case reports and small clinical trials. (22-27) Our observation of differential hemodynamic effects of sildenafil and iNO vs iloprost aerosol are in concordance with the concept that these substances activate different regulatory systems of vascular tone, and therefore combination of these substances may prove beneficial in the treatment of pulmonary hypertension.
REFERENCES
(1) D'Alonzo GE, Bart RJ, Ayres SM, et al. Survival in patients with primary pulmonary hypertension: results from a national prospective study. Ann Intern Med 1991; 115:343-349
(2) Rubin LJ. Pathology and pathophysiology of primary pulmonary hypertension. Am J Cardiol 1995; 75:51A-54A
(3) Wagenvoort C, Wagenvoort N. Primary pulmonary hypertension: a pathological study of the lung vessels in 156 clinically diagnosed cases. Circulation 1970; 42:1163-1184
(4) Fuster V, Steele P, Edwards W, et al. Primary pulmonary hypertension: natural history and the importance of thrombosis. Circulation 1984; 70:580-587
(5) Frank H, Mlczoch J, Huber K, et al. The effect of anticoagulant therapy in primary and anorectic drug-induced pulmonary hypertension. Chest 1997; 112:714-721
(6) Gaine SP, Rubin LJ. Primary pulmonary hypertension. Lancet 1998; 352:719-725
(7) Weir EK, Rubin LJ, Ayres SM, et al. The acute administration of vasodilators in primary pulmonary hypertension: experience from the National Institutes of Health Registration Primary Pulmonary Hypertension. Am Rev Respir Dis 1989; 140:1623-1630
(8) Rich S, Kaufmann E, Levy PS. The effect of high doses of calcium-channel blockers on survival in primary pulmonary hypertension. N Engl J Med 1992; 327:117-119
(9) Sitbon O, Humbert M, Jagot LJ, et al. Inhaled nitric oxide as a screening agent for safely identifying responders to oral calcium channel blockers in primary pulmonary hypertension. Eur Respir J 1998; 12:265-270
(10) Ricciardi MJ, Knight BP, Martinez FJ, et al. Inhaled nitric oxide in primary pulmonary hypertension: a safe and effective agent for predicting response to nifedipine. J Am Coll Cardiol 1998; 32:1068-1073
(11) Olschewski H, Simonneau G, Galie N, et al. Inhaled iloprost for severe pulmonary hypertension. N Engl J Med 2002; 347:322-329
(12) Hoeper M, Schwarze M, Ehlerding S, et al. Long term treatment of primary pulmonary hypertension with aerosolized iloprost, a prostacyclin analogue. N Engl J Med 2000; 342:1866-1870
(13) Olschewski H, Ghofrani, Schmehl T, et al. Inhaled iloprost to treat severe pulmonary hypertension (an uncontrolled trial). Ann Intern Med 2000; 132:435-443
(14) Wensel R, Opitz Ch, Ewert, et al. Effects of iloprost inhalation on exercise capacity and ventilatory efficiency in patients with primary pulmonary hypertension; Circulation 2000; 101: 2388-2392
(15) Hoeper M, Olschewski H, Ghofrani A, et al. A comparison of the acute hemodynamic effects of inhaled nitric oxide and aerosolized iloprost in primary pulmonary hypertension. J Am Coll Cardiol 2000; 35:176-181
(16) Olschewski H, Walmrath D, Schermuly R, et al. Aerosolized prostacyclin and iloprost in severe pulmonary hypertension. Ann Intern Med 1996; 124:820-824
(17) Higgenbottam T, Wheeldon D, Wells F, et al. Long-term treatment with continuous intravenous epoprostenol (prostacyclin) in primary pulmonary hypertension. Lancet 1984; 1:1046-1047
(18) Mc Laughlin VV, Genthner DE, Panella MM, et al. Reduction in pulmonary vascular resistance with king-term epoprostenol (prostacyclin) therapy in primary pulmonary hypertension; N Engl J Med 1998; 338:273-277
(19) Barst RJ, Rubin LJ, Long WA, et al. A comparison of continuos intravenous epoprostenol with conventional therapy for primary pulmonary hypertension; N Engl J Med 1996; 334:296-301
(20) Rubin LJ, Mendoza M, Hood M, et al. Treatment of primary pulmonary hypertension with continuos intravenous prostacyclin (epoprostenol): results of randomised trial. Ann Intern Med 1990; 112:485-491
(21) Kleinsasser A, Loeckinger A, Hoermann C, et al. Sildenafil modulates hemodynamic and pulmonary gas exchange. Am J Respir Crit Care Med 2001; 163:339-343
(22) Abrams D, Schulze-Neick I, Magee AG. Sildenafil: a selective pulmonary vasodilator in childhood primary pulmonary hypertension. Heart 2000; 84:E4
(23) Prasad S, Wilkinson J, Gatzoulis MA. Sildenafil in primary pulmonary hypertension [letter]. N Engl J Med 2000; 343: 1342
(24) Atz AM, Wessel DL. Sildenafil ameliorates effects of nitric oxide withdrawal. Anesthesiology 1999; 91:307-310
(25) Bigatello LM, Hess D, Dennehy KC, et al. Sildenafil can increase the response to nitric oxide. Anesthesiology 2000; 92:1827-1829
(26) Wilkens HW, Guth A, Konig J, et al. Effect of inhaled iloprost plus oral sildenafil in patients with primary pulmonary hypertension. Circulation 2001; 104:1218-1222
(27) Ghofrani HA, Wiedemann R, Rose F, et al. Combination therapy with oral sildenafil and inhaled iloprost for severe pulmonary hypertension. Ann Intern Med 2002; 136:515-522
(28) Rich S, ed. Primary pulmonary hypertension: executive summary from the world symposium--primary pulmonary hypertension Evian 1998. Available at: http://www.aafp.org/afp/ 20010501/1789.html. Accessed January 20, 2004
(29) Raffy O, Azarian R, Brenot F, et al. Clinical significance of the pulmonary vasodilator response during short-term infusion of prostacyclin in primary pulmonary hypertension. Circulation 1996; 93:484-488
(30) Pepke-Zaba J, Higgenbottam TW, Dinh-Xuan AT, et al. Inhaled nitric oxide as a cause of selective pulmonary vasodilation in pulmonary hypertension. Lancet 1991; 338:1173-1174
(31) Sitbon O, Brenot F, Denjean A, et al. Inhaled nitric oxide as a screening vasodilator agent in primary pulmonary hypertension: a dose-response study and comparison with prostacyclin. Am J Respir Crit Care 1995; 151:384-389
(32) Ghofrani HA, Wiedemann R, Rose F, et al. Sildenafil for the treatment of lung fibrosis and pulmonary hypertension: a randomised controlled trial. Lancet 2002; 360:895-900
(33) Rabe KF, Tenor H, Dent G, et al. Identification of PDE isozymes in human pulmonary artery and effect of selective PDE inhibitors. Am J Physiol 1994; 266:L536-L543
(34) Beavo JA. Cyclic nucleotide phosphodiesterases: functional implications of multiple isoforms. Physiol Rev 1995; 75:725-748
(35) Goldstein I, Lue TF, Padma-Nathan H, et al. Oral sildenafil in treatment of erectile dysfunction. N Engl J Med 1998; 338:1397-1404
(36) Jackson G, Benjamin N, Jackson N, et al. Effects of sildenafil citrate on human hemodynamics. Am J Cardiol 1999; 83: 13C-20C
(37) Ignarro LJ. Biological actions and properties of the endothelium-derived nitric oxide formed and released for artery and vein. Circ Res 1989; 65:1-21
(38) Ignarro LJ. Biosynthesis and metabolism of endothelium-derived nitric oxide. Annu Rev Pharmacol Toxicol 1990; 30:535-560
(39) Ignarro LJ. Signal transduction mechanisms involving nitric oxide. Biochem Pharmacol 1991; 41:485-490
(40) Ichinose F, Adrie C, Hurford WE, et al. Prolonged pulmonary vasodilator action of inhaled nitric oxide by zaprinast in awake lambs. J Appl Physiol 1995; 78:1288-1295
(41) Schermuly RT, Roehl A, Weissmann N, et al. Combination of non specific PDE inhibitors with inhaled prostacyclin in experimental pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol 2001; 281:L1361-L1368
* From the Department of Internal Medicine I, Section for Pulmonary Diseases, Klinikum Grosshadern, Ludwig-Maximilians-University Munich, Munich, Germany.
Manuscript received December 17, 2002; revision accepted September 4, 2003.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Hanno H. Leuchte, MD, Department of Internal Medicine I, Section for Pulmonary Diseases, Klinikum Grosshadern, Ludwig-Maximilians-University Munich, Munich, Germany; e-mail: hleuchte@helios.med.uni-muenchen.de
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group