Background: Inhalation of iloprost, a stable prostacyclin analog, is an effective therapy for pulmonary hypertension with few side effects. This approach may, however, be handicapped by limitations of currently available nebulization devices. We assessed whether the physical characterization of a device is sufficient to predict drug deposition and pharmacologic effects.
Methods: We investigated the effects of a standardized iloprost aerosol dose (5 g[micro] inhaled within approximately 10 min) in 12 patients with severe pulmonary hypertension in a crossover design employing three well-characterized nebulizers. The nebulizers use different techniques to increase efficiency and alveolar targeting (Ilo-Neb/Aerotrap [Nebu-Tec; Elsenfeld, Germany], Ventstream [MedicAid; Bognor Regis, UK], and HaloLite [Profile Therapeutics; Bognor Regis, UK]). Measurements were performed using a Swan-Ganz catheter and determination of arterial iloprost plasma levels.
Results: During inhalation of iloprost, the pulmonary vascular resistance decreased substantially (baseline, approximately 1,250 dyne*s*[cm.sup.-5]; decrease, - 35.5 to - 38.0%) and pulmonary artery pressure decreased substantially (baseline, approximately 58 mm Hg; decline, - 18.4 to -21.8%), whereas the systemic arterial pressure was largely unaffected. Cardiac output and mixed venous and arterial oxygen saturation displayed a marked increase. The pharmacodynamic profiles with the three devices were superimposable. Moreover, rapid entry of iloprost into the systemic circulation was noted, peaking immediately after termination of the inhalation maneuver, with very similar maximum serum concentrations (1.58 pg/mL, 155 pg/mL, and 157 pg/mL), and half-lives of serum levels (6.5 min, 9.4 min, and 7.7 min) for the three nebulizers, respectively. Interestingly, the "half-life" of the pharmacodynamic effects in the pulmonary vasculature (eg, decrease in pulmonary vascular resistance, ranging between 21 and 25 min) clearly outlasted this serum level-based pharmacokinetic half-life.
Conclusions: A standardized dose of aerosolized iloprost delivered by different nebulizer types induces comparable pharmacodynamic and pharmacokinetic responses. Pulmonary vasodilation, persisting after disappearance of the drug from the systemic circulation, supports the hypothesis that local drug deposition largely contributes to the preferential pulmonary vasodilation in response to inhaled iloprost.
Key words: iloprost: nebulization device: pulmonary hypertension
Abbreviations: ANOVA = analysis of variance: AUC = area under the serum level-time curve; AUCt0-tlast = area under the serum level-time curve calculated from the start of inhalation to the last sampling time point; Cmax = maximum serum concentration; NO = nitric oxide; PAP pulmonary artery pressure: PPH = primary pulmonary hypertension; PVR = pulmonary vascular resistance: Sa[O.sub.2] = arterial oxygen saturation: SAP systemic artery pressure; SV[O.sub.2] = mixed venous oxygen saturation: SVR = systematic vascular resistance
**********
Primary pulmonary hypertension (PPH) is a severe disabling disease with a poor prognosis. (1) Long-term infusion of prostacyclin was the first therapy shown to be lifesaving in a controlled study, (2) and such efficacy may also exist for patients with the scleroderma spectrum of diseases, (3) and other diseases associated with severe pulmonary arterial hypertension. (4, 5) However, this approach is hampered by the lack of pulmonary selectivity of the vasodilatory effect of prostacyclin causing systemic side effects such as pain and systemic hypotension, (6) by ventilation-perfusion mismatch in predisposed patients, (7-9) as well as by infectious complications due to the continuous use of an IV line. (6) Inhalation of nitric oxide (NO) is selective for the lung vasculature, but its pulmonary vasodilatory potency is lower than that of prostacyclin, (10-12) and interruption of NO inhalation may provoke a rebound hypertensive crisis due to the very short half-life of this agent. (13,14)
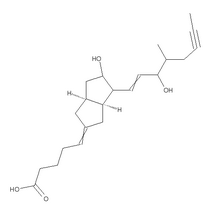
As an alternative approach, repetitive aerosol delivery of iloprost, a stable prostacyclin analog, has been used to treat pulmonary hypertension and proved to be efficacious in a double-blind, placebo-controlled study. (15) In PPH and other forms of precapillary pulmonary hypertension, it was demonstrated that nebulized iloprost decreases pulmonary vascular resistance (PVR) and pulmonary artery pressure (PAP), concomitant with an increase in cardiac output, in the absence of significant systemic arterial pressure drop and ventilation-perfusion mismatch. (9,16,-18) Rescue administration of inhaled iloprost was undertaken in progressive right-heart failure due to severe pulmonary hypertension, (19,20) and currently available data from a 2-year study with iloprost aerosolization suggest beneficial long-term effects with minor side effects. (21)
The aerosol approach is, however, handicapped by limitations of the currently available nebulization devices. Substantial loss of the aerosolized drug in the device is a common finding, resulting in major and possibly variable differences between the dose delivered into the device, the nebulized dose, and the inhaled dose. Droplet size and aerosol concentration during the inhalation phase may determine the extent and the site of pulmonary drug deposition, and thus on delivery of the inhaled agent to the pulmonary vasculature.
In the present study, we investigated the pharmacokinetics and the pharmacodynamic effects of inhaled iloprost in patients with severe pulmonary hypertension. Three different jet nebulizers manufactured for alveolar drug delivery were employed. The first, coupled with a reservoir for alveolar targeting (Ilo-Neb/Aerotrap; Nebu-Tee; Elsenfeld, Germany) has been widely employed in long-term iloprost nebulization including the open-label, 2-year study in Germany. (21) Due to the reservoir, this device is relatively large. Additionally, considerable amounts of aerosol are deposited inside the device, resulting in an efficiency (inhaled dose/filling dose) of only approximately 13%. The second nebulizer uses the Venturi effect to boost aerosol production during inspiration (Ventstream; MedicAid; Bognor Regis, UK) and is much smaller as it does not need a reservoir, but loses efficiency due to internal drug deposition and high filling volumes (efficiency approximately 15%). The third nebulizer employs a microchip technique for delivery of an aerosol pulse during the first half of the inhaled tidal volume, and was used in the pivotal trial showing clinical efficacy of inhaled iloprost. (15) It combines increased efficiency (approximately 25%) with exact aerosol dosing independent of the breathing pattern (HaloLite; Profile Therapeutics; Bognor Regis, UK).
The dosing regimen for each nebulizer was adjusted to deliver a total amount of 5 [micro]g of iloprost to the respiratory tract of the patients (calculated for entry at mouthpiece) during an inhalation maneuver lasting approximately 10 min, based on preceding biophysical characterization of these devices. (22) Following such a standardized procedure, the pharmacodynamic effects of inhaled iloprost were found to be virtually superimposable for all devices tested. Moreover, this was also true for the kinetics of iloprost appearance and disappearance in the systemic circulation in response to its aerosol delivery. Interestingly, the serum levels of inhaled iloprost declined much more rapidly than the pullmonary vasodilatory effect, which suggests prolonged local vasorelaxant potency of the aerosolized agent nut reflected by the time course of serum levels.
MATERIALS AND METHODS
Patients
A total of 12 patients (aged > 18 years) with PPH or secondary pulmonary hypertension were enrolled in the study. The patients had been treated for at least 3 months with six iloprost inhalations per day in three experienced German centers for pulmonary hypertension. Only patients who were known to respond to iloprost inhalation with a decrease of PVR of at least 20% were included. Patients with renal or severe hepatic impairment, thromboembolic disease, bleeding disorders, significant restrictive or osbstructive lung diseases, pulmonary venous hypertension, and diseases directly affecting the pulmonary vessels, according to the new diagnostic World Health Organization classification. (23) were excluded from the study, The patients gave written informed consent before participation in the trial. The study protocol was reviewed and approved by the local ethics committees of the participating centers.
Nebulizing Devices
Three different jet nebulizer systems were used: (1) Ilo-Neb combined with the Aerotrap reservoir, and the Pulmocar Akku compressor (Sanesco Medizintechnik; Vienna, Austria): (2) Ventstream combined with the Freeway Lite compressor (MedicAid); and (3) HaloLite. On the basis of preceding in vitro characterization of the aerosols delivered by each device, (22) the volume of the iloprost solution to be filled into the nebulizer and the concentration of the iloprost solution were adjusted for each device to provide a total dose of 5 [micro]g of iloprost delivered at the mouthpiece within a comparable time span. The physical characteristics of the nebulizers and the dose regimens are depicted in Table 1. Accordingly, the inhalation time was defined to be 12 min and 10 min for the IloNeb and the Ventstream nebulizers, respectively. In contrast, the nebulization time of the HaloLite system is not prefixed, because this device stops automatically when the inhalation of the prescribed dose is completed. The basis of this system is a breath-by-breath measurement and summing up of the total inhaled quantity. Inhalation times for the HaloLite nebulizer were thus variable, depending on the breathing pattern of the patient, with an average of approximately 11 min. The iloprost solution administered with the nebulizer was prepared immediately before use, according to written detailed dosing instructions.
Study Conduct
A randomized, open-label, multicenter, crossover trial design was used with six sequences, three treatments and three periods (also known as Williams design). Each patient was randomly assigned to one of the six possible sequences of treatments. The iloprost aerosol (total dose of 5 [micro]g at the mouthpiece) was administered by three subsequent inhalations using the three different devices in randomized order. Every treatment was followed by a washout time of 2 h. All treatments were administered on a single day during a previously scheduled right-heart catheterization. For safety reasons, the following inhalation stop criteria were defined: (1) decrease of mean systemic BP to < 65 mm Hg or by > 10% of baseline for at least 2 min, (2) decrease of arterial oxygen saturation (Sa[O.sub.2]) by > 5% for at least 2 min, (3) severe headache, and/or (4) local intolerability of the aerosol.
Before inhalations were started, a Swan-Ganz catheter (Baxter Edwards; Deerfield, IL) and an arterial line were inserted. A fiberoptic thermodilution pulmonary artery catheter was used for measuring PAP, pulmonary artery wedge pressure, central venous pressure, and cardiac output. The arterial line was used for continuous measurement of systemic arterial pressure (SAP) and drawing arterial blood samples for blood gas analysis and measurement of iloprost serum levels. For assessment of P[O.sub.2], Pa[O.sub.2], and PaC[O.sub.2], as well as Sa[O.sub.2] and mixed venous oxygen saturation (Sv[O.sub.2), venous and arterial blood samples were withdrawn at baseline, at end of inhalation, and 30 min, 60 min, and 120 min after the end of inhalation. Hemodymics and drug concentrations were measured simultaneously. Additionally, hemodynamics were assessed 5 min and 15 min after the end of inhalation, and drug concentrations were measured 2 min, 5 min, and 15 min after the end of inhalation.
Measurement of Iloprost Concentrations
Serum levels of iloprost were measured using a specific and sensitive radioimmunoassay with a quantitation limit of 25 pg/ mL. The assay was validated using human samples and gas chromatography coupled with mass spectrometer as an alternative analysis procedure. (24)
Pharmacokinetic Evaluation
Pharmacokinetic parameters were obtained from the individual serum level time curves using the TOPFIT program, Version 2.1 (Goedecke AG, Schering AG, Thomae GmbH; Freiburg, Germany). Maximum serum concentration (Cmax) and time to reach Cmax were directly taken from the data. The area under the serum level-time curve (AUC) was calculated according to the linear trapezoidal rule from the start of inhalation to the last sampling time point (AUCt0-tlast), which was calculated with concentrations above the limit of quantitation (AUCt0-flast) and the partial area from the last sampling time point to the respective next sampling time point for which the concentration was set at zero. This method of extrapolating AUC was chosen because AUC measured at the start of inhalation to infinity could not be obtained in all eases due to the rapid decrease of iloprost serum levels after the end of inhalation. In assessments with quantifiable iloprost serum levels in the last blood sample of treatment periods 1 and 2, only AUCt0-tlast could be calculated and was used for subsequent statistical evaluation. Patient 11 was excluded from evaluation of treatment 2 (Ventstream device) because no drug exposure was achieved due to a technical problem during inhalation.
For further characterization if the pharmacokinetics of inhaled iloprost, the half-life ([t.sub.1/2]) of the iloprost serum level decrease was calculated by means of regression analysis of the mean serum level-time curve between the end of inhalation, and 30 min after end of inhalation in a semilogarithmic plot ([lambda] = slope of regression line): [t.sub.1/2] = 2/[lambda]. Accordingly, the "half-life" of the pharmacodynamic effect was calculated, employing the iloprost-induced decrease in PVR. Calculation was performed by means of regression analysis of the time curves of absolute changes of PVR compared to baseline between the time point of maximum effect and 30 min after end of inhalation in a semilogarithmic plot ([lambda] = slope of regression line): [t.sub.1/2] = 2/[lambda],
Statistics
The target variables were the maximum percentage changes in the hemodynamic variables in response to iloprost inhalation and the pharmacokinetic variables Cmax and AUC. Analysis of variance (ANOVA) for a mixed linear model using fixed effects (period, treatment, and first-order carryover) as well as random subject effect was performed to compare the target variables. Two-sided tests and confidence intervals were adjusted for three multiple comparisons according to Turkey-Kramer. The multiple significance (confidence) level was set at 0.05 (0.95) for each target variable. There was no adjustment for multiple end points.
RESULTS
Nine female and four male patients (aged 26 to 71 years) were included in the study. Twelve of them completed the trial. One male patient was prematurely withdrawn due to an exclusion criterion that became evident immediately after start of the first treatment (mean SAP < 65 mm Hg). Eleven of the 12 patients had PPH, and 1 patient presented with isolated pulmonary hypertension with CREST syndrome (calcinosis, Raynaud phenomenon, esophageal dysfunction, sclerodactyly, telangiectasia without lung fibrosis or major inner organ involvement). Body weight ranged between 41 kg and 86 kg.
In 33 of 36 inhalation maneuvers, the aerosolization was entirely finished; in three eases, it was stopped prematurely (although close to the pre-defined end of inhalation) due to a decrease in mean systemic BP by > 10% of baseline for > 2 min. The patients did not experience any subjective adverse events.
Iloprost inhalation caused an average PVR decrease of 35.5 to 38.0% compared to baseline, with a maximum effect either immediately at the end of inhalation, or within 5 min (Table 2, Fig 1). The PVR decrease was paralleled by an average decrease in mean PAP of 18.4 to 21.8%, and an average increase in cardiac output of 30.6 to 37.1%. The SAP showed only some marginal decrease, while systemic vascular resistance (SVR) changes were noted in parallel with the changes in cardiac output (Fig 2, top, A, and center, B; Table 2). The PVR/SVR ratio indicated a more pronounced effect of iloprost inhalation on the PVR than on the SVR (Fig 2, bottom, C).
[FIGURES 1-2 OMITTED]
Heart rate was not significantly changed (data not given), and no relevant arrhythmia was noted. The mean Sa[O.sub.2] and mean Sv[O.sub.2] increased in response to iloprost inhalation (Fig 3; Table 2). A critical decrease in Sa[O.sub.2] (> 5% compared to baseline) did not occur in any patient.
[FIGURE 3 OMITTED]
Iloprost serum levels became rapidly detectable with all three devices employed (Fig 4). Serum concentrations reached a maximum either at the end of inhalation or within the following 5 min (Fig 4; Table 2). Beyond 30 min after the end of inhalation, quantifiable serum levels of iloprost were detected in only 3 of the 12 patients. Cmax and AUC values were comparable using the different nebulizers (Table 2). After reaching an early concentration peak, iloprost serum levels rapidly decreased with a half-life of 6.5 to 9.4 min (Table 3). In contrast, the half-life of the pharmacodynamic effect, as calculated from the PVR decrease, ranged between 21 min and 25 min.
[FIGURE 4 OMITTED]
When statistical analysis (ANOVA) was applied to the hemodynamic and pharmacokinetic responses to iloprost inhalations performed with the different devices, no significant differences between the devices were revealed, except for a slightly more pronounced SAP decrease shortly after iloprost inhalation using the HaloLite compared to the IloNeb system (Table 4). However, this was not associated with any typical complaints and not considered clinically significant in any case.
The iloprost aerosol administration was well tolerated by the patients irrespective of the nebulization device employed. Minor adverse events such as transient headache and flush were noted with similar frequencies with all devices: headache occurred in 4 patients, 3 patients, and 4 patients following inhalations using HaloLite, Ventstream, and IloNeb, respectively, and flush was observed in 6 patients, 8 patients, and 10 patients. Both of these adverse events were closely related to the peak iloprost serum levels, starting during or immediately after the end of inhalation and lasting for a few minutes. In three patients, mild cough occurred during inhalation, which did not impair or limit the inhalation. Further adverse events possibly related to study drug occurred only in single cases: ventricular extrasystoles, palpitation, chest pain, sore throat, rash, tinnitus, eye pain, and taste perversion. All adverse events were of mild or moderate intensity and disappeared completely mostly within minutes.
DISCUSSION
In this study, the dosing regimen of three different jet nebulizers was adjusted to deliver a total quantity of 5 [micro]g of iloprost to the respiratory tract of patients with severe pulmonary hypertension during an inhalation maneuver of approximately 10 min. The dose calculation was based on detailed biophysical characterization. Preferential pulmonary vasodilation with concomitant increase in cardiac output was noted, and assessment of iloprost serum levels documented rapid entry of the inhaled agent into the systemic circulation. Both the pharmacodynamic and the phannacokinetic effects were superimposable for all three devices employed. The serum half-life of iloprost was, however, much shorter than the half life of the pulmonary vasodilatory effects exerted by this agent, suggesting that the inhaled iloprost cause prolonged local vasodilation not reflected by the serum levels.
The patients were selected based on a documented acute PVR fall > 20% in response to a previous iloprost inhalation. The rationale behind this was to improve the chance to show differences between the devices. In a previous study (12) comparing NO and inhaled iloprost in nonselected patients with PPH, only approximately 20% had a poor acute vasodilatory response to inhaled iloprost consisting of < 20% PVR decrease, and the mean PVR response to inhaled iloprost was 32%. This suggests that the patient population of the present study represents the majority of patients with PPH.
The devices currently investigated employed different mechanisms for alveolar targeting. In the lloNeb/Aerotrap system, the aerosol is continuously produced, but during expiration it is stored in the Aerotrap reservoir. At the beginning of the next inspiration, the aerosol content of the reservoir together with the continously produced aerosol enters the lung, resulting in enchanced aerosol concentration. In contrast, at the end of the inhalation phase, only the freshly produced (less concentrated) aerosol is carried to the respiratory tract with parts of it filling the dead space of the respiratory tract. The main disadvantages of this device are the dimensions of the reservoir and the drug loss within the apparatus, mainly due to aerosol deposition at the inspiratory value. The Ventstream nebulizer uses a value system to provide an additional inspiratory side flow for enhancing the aerosol output during inhalation by the Venturi principle. Consequently, aerosol formation is reduced while the patient is exhaling, thereby matching aerosol delivery with tidal volume and suppressing drug wastage. Nevertheless, due to continous operation of the nebulizer, there is considerable aerosol loss during expiration. Moreover, there is substantial intradevice drug wastage due to a high minimum filling volume required in the aerosol chamber. The HaloLite is a new electronically controlled device, applying aerosol pulses only in a preset period during early inspiration, with delivery adjusted to the breathing pattern. These aerosol pulses are added up, and the device stops automatically when the target dose has been delivered. The main advantages of the system are the virtual absence of aerosol delivered to the airway dead space, the fact that the predefined drug dose will be applied irrespective of the breathing pattern, and the low volume of inhalation solution necessary for sufficient nebulization. However, a high driving pressure is needed for this device, which requires continous connection to mains, and the filling volume considerably exeeeds the maximum nebulized volume. For clinical practice, it is important to note that the filling volume and the inhaled volume differ considerably and that their ratio critically depends on the device itself and on the mode of use. Therefore, recommendations for devices for use of inhaled iloprost have to consider all these factors.
It is a main finding of the present study that--irrespective of the substantial technical differences of the devices employed--the pharmacodynamic effects of inhaled iloprost were virtually superimposable. As previously described, (9,16,16-20) preferential pulmonary vasodilation was noted, with a decrease in both PVR and PAP, whereas the SAP was largely unaffected. In parallel, the cardiac output and both Sv[O.sub.2] and Sa[O.sub.2] consistently increased, with all effects leveling off within approximately 60 min. Moreover, rapid entry of the inhaled drug into the systemic circulation was observed for all devices employed, a Cmax of approximately 160 pg/mL of iloprost was detected immediately after termination of inhalation, with subsequent rapid disappearance of this agent from the systemic vasculature. Two conclusions may be drawn from these findings: (1) detailed biophysical characterization of the aerosol devices provides a sound basis for reliable calculation of the dosage of a drug delivered by nebulization to the alveolar compartment or even via inhalation to the systemic circulation, and (2) the different technical solutions developed for alveolar drug targeting in the three devices tested do result in comparable hemodynamic and pharmacokinetic effects of the standardized dose of 5 [micro]g of iloprost delivered to the mouthpiece, irrespective of the differences in aerosol concentration during the inhalation cycle discussed above. Moreover, tolerability of the inhalation maneuver was comparable for all devices, with only minor adverse effects such as flush, which is a typical systemic side effect of iloprost.
In the present study, a radioimmunoassay technique was employed for measurement of iloprost serum levels, the sensitivity and specificity of which were calibrated against a gas chromatography coupled with mass spectrometer method used in previous studies of IV iloprost administration. (24) After the inhalation maneuver with delivery of 5 [micro]g of iloprost, 73 ng/kg, in approximately 10 min to the respiratory tract, a mean AUC between 47.8 pg/h/mL and 54.2 pg/h/mL was measured for the different nebulizers. These data may be compared to IV iloprost administration: in healthy volunteers, iloprost, 3 ng/kg/min, was infused over 45 min (total, 135 ng/kg), resulting in a mean AUC value of 119 pg/h/mL. (25) Assuming that the difference in time of administration (45-min infusion vs approximate 10-min inhalation) has no major impact on the AUC, an absolute bioavailability (entrance into the vascular compartment) of the inhaled iloprost of approximately 80% was calculated. This result is much higher than previously estimated and suggests that during inhalation the majority of particles was, indeed, deposited in the respiratory tract, with only a small percentage being exhaled, and that there is ready access of the deposited iloprost aerosol to the vascular space. Nevertheless, there was a major time gap between the pharmacokinetic half-life of iloprost once having entered the blood system (6.5 to 9.4 min for the different devices) and the half-life of the pharmacodynamic effect in the pulmonary vasculature, as calculated from the PVR decrease (21 to 25 min). Several mechanisms may underlie this observation. First, some percentage of iloprost may be retained in the perivascular lung tissue (alveolar lining layer, interstitial space, pulmonary artery cells) after nebulization, and this fraction may possess a much longer half-life than the systemic iloprost, as it is not exposed to the catabolic capacity of the liver on recirculation. This view is supported by the fact that in perfused rabbit lungs--in contrast to intact rabbits--a half-life for recirculating iloprost of > 1 h is noted, independent of the route of administration (inhalation or infusion). (26) As the alveolar lining layer and the interstitium of the lung are very small spaces, even a low total quantity of agent may result in high local concentrations. Second, high local concentrations of iloprost are expected to exist in the perivascular and vascular tissue during passage of this agent from the alveolar into the vascular compartment. As a "memory" effect of these high local concentrations, the vasorelaxation in the pulmonary circulation may by far outlast the kinetics of disappearance of iloprost from the systemic circulation. Third, it might be a general feature of the pulmonary vasculature to respond with prolonged vasorelaxation to even a short iloprost exposure, independent of the route of drug administration.
In conclusion, comparable pharmacokinetic and hemodynamic effects were achieved with a standardized dose of aerosolized iloprost in severe pulmonary hypertension in a controlled clinical setting, irrespective of the different types of nebulization technique employed. Based on detailed biophysical characterization, a reliable delivery and vasodilatory effect of this agent can be achieved. The local vasodilatory effect of inhaled iloprost by far outlasts the disappearance of this agent from the systemic circulation, which supports the hypothesis that local pulmonary drug deposition results in preferential pulmonary as compared to systemic vasodilatory potency of inhaled iloprost.
ACKNOWLEDGMENT: We thank Almut Heuner, MD, and Birgit Hanke, MD, for pharmacodynamic and pharmacokinetic measurements: Werner Seeger, MD PhD, for his contributions to the experimented design and critical discussion of the manuscript; and Mary Kay Steen-Mueller, MD, for reviewing the manuscript.
REFERENCES
(1) D'Alonzo GE, Barst RJ, Ayres SM. et al. Survival in patients with primary pulmonary hypertension: results flora a national prospective registry, Ann Intern Med 1991; 115:343-349
(2) Barst RJ, Rubin LJ, Long WA, et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. The Primary Pulmonary Hypertension Study Group N Engl J Med 1996; 334:296-302
(3) Badesch DB, Tapson VF. McGoon MD, et al. Continuous intravenous epoprostenol for pulmonary hypertension due to the scleroderma spectrum of disease: a randomized, controlled trial. Ann Intern Med 2000:132:425-434
(4) Rosenzweig EB, Kerstein D, Barst RJ. Long-term prostacyclin for pulmonary hypertension with associated congenital heart defects. Circulation 1999; 99:1858-1865
(5) McLaughlin VV, Genthner DE, Panella MM, et al. Compassionate use of continuous prostacyclin in the management of secondary pulmonary hypertension: a case series. Ann Intern Med 1999; 130:740-743
(6) Barst RJ, Rubin LJ, McCoon MD, et al. Survival in primary pulmonary hypertension with long term continuous intravenous prostacyclin. Ann Intern Med 1994; 121:409-415
(7) Agusti AG, Rodriguez-Roisin R. Effect of pulmonary hypertension on gas exchange. Eur Respir J 1993; 6:1371-1377
(8) Walmrath D, Sehneider T, Pilch J, et al. Aerosolised prostacyclin in adult respiratory distress syndrome. Lancet 1993; 342:961-962
(9) Olschewski H, Ghofrani HA, Walmrath D, et al. Inhaled prostacyclin and iloprost in severe pulmonary hypertension secondary to lung fibrosis. Am J Respir Crit Care Med 1999; 160:600-607
(10) Sitbon O, Brenot F. Denjean A, et al. Inhaled nitric oxide as a screening vasodilator agent, in primary pulmonary hypertension: a dose-response study and comparison with prostacyclin. Am J Respir Crit Care Med 1995:151:384-389
(11) Warren JB, Higenbottam T. Caution with use of inhaled nitric oxide, Lancet 1996; 348:629-630
(12) Hoeper MM, Olschewski H, Ghofrani HA, et al. A comparison of the acute hemodynamic effects of inhaled nitric oxide and aerosolized iloprost in primary pulmonary hypertension. German PPH Study Group. J Am Coll Cardiol 2000: 35:176-182
(13) Miller OI, Tang SF, Keech A. et al. Rebound pulmonary hypertension on withdrawal from inhaled nitric oxide. Lancet 1995; 346:51-52
(14) Cueto E, Lopez Herce J, Sanchez A, et al. Life-threatening effects of discontinuing inhaled nitric oxide in children. Acta Paediatr 1997: 86:1337-1339
(15) Olschewski H, Simonneau G, Galie N, et al. Inhaled iloprost for severe pulmonary hypertension. N Engl J Med 2002; 347:322-329
(16) Hoeper MM, Schwarze M, Ehlerding S, et al. Long-term treatment of primary pulmonary hypertension with aerosolized iloprost, a prostacyclin analogue. N EngI J Med 2000: 342:1866-1870
(17) Olschewski H, Walmrath D. Schermuly R, et al. Aerosolized prostacyclin and iloprost in severe pulmonary hypertension, Ann Intern Med 1996; 124:820-824
(18) Wensel R, Opitz CF, Ewert R, et al, Effects of iloprost inhalation on exercise capacity and ventilatory efficiency in patients with primary pulmonary hypertension. Circulation 2000; 101:2388-2392
(19) Olschewski H, Ghofrani HA, Walmrath D. et al. Recovery from circulatory shock in severe primary pulmonary hypertension (PPH) with aerosolization of iloprost. Intensive Care Med 1998; 24:631-634
(20) Olschewski H, Ghofrani HA, Schmehl T, et al. Inhaled iloprost to treat severe pulmonary hypertension: an uncontrolled trial. German PPH Study Group. Ann Intern Med 2000; 132:435-443
(21) Nikkho S, Seeger W, Baumgartner R. et al. One-year observation of iloprost therapy in patients with pulmonary hypertension [abstract]. Eur Respir J 2001; 18(suppl 33):3248
(22) Roth C, Heyder J, Wagner T, et al. In vitro characterization of ilomedin inhalation devices [abstract]. J Aerosol Med 1999; 12:98
(23) Rich S. Primary pulmonary hypertension. Executive Summary from the World Symposium on Primary Pulmonary Hypertension. Evian, France; September 6-10, 1998
(24) Hildebrand M, Krause W, Angeli P, et al. Pharmacokinetics of iloprost in patients with hepatic dysfunction. Int J Clin Pharmacol Ther Toxicol 1990:28:430-434
(25) Krause W, Krais T. Pharmacokinetics and pharmacodynamics of the prostacyclin analogue iloprost in man. Eur J Clin Pharmacol 1986:30:61-68
(26) Schermuly RT, Schulz A, Ghofrani HA, et al. Pharmacokinetics and metabolism of infused versus inhaled iloprost in isolated rabbit lungs. J Pharmacol Exp Ther 2002; 303:741-745
* From the Department of Internal Medicine (Drs. Olschewski, Gessler, Ghofrani, and Schmehl), Justus-Liebig-University, Giessen; Schering AG (Dr. Rohde), Berlin: Ludwig-Maximilians-University (Dr, Behr), Munich; and Deutsches Herzzentrum (Dr. Ewert), Berlin, Germany.
The study was funded by Schering AG, Berlin, Germany. Drs. Olschewski, Gessler, and Schmehl are consultants for Schering AG and NebuTec Company. Dr. Rohde is an employee of Schering AG.
Manuscript received October 18, 2002: revision accepted February 10, 2003.
Correspodence to: Horst Olschewski, MD, PhD. Department of lnternal Medicine II, University Hospital, Klinikstrasse 36, D-35392 Giessen; Germany; e-mail horst.olschewski@innere. med.uni-giessen.de
COPYRIGHT 2003 American College of Chest Physicians
COPYRIGHT 2003 Gale Group