Background: Aerosolized iloprost is used as an alternative to IV prostacyclin in patients with pulmonary hypertension. The desired outcome of this treatment is a reduction of pulmonary pressure, which can be measured by right-heart catheterization or Doppler echocardiography. However, both techniques provide only snapshots of the hemodynamic state.
Patients and methods: The aim of our study was to test the usability of an implantable hemodynamic monitor (IHM) [the Chronicle, model 9520; Medtronic Inc; Minneapolis, MN] in patients with pulmonary hypertension. For this purpose, the device was implanted into five patients (mean [[+ or -] SEM] age, 45 [+ or -] 16 years; all women) with pulmonary hypertension who had received long-term treatment with aerosolized iloprost (100 [micro]g/d). Repeated short-term tests including two standard inhalations of iloprost as well as repeated long-term tests lasting 20 to 26 h, including nighttime, without inhalation were performed on an outpatient basis.
Results: The device provided information that was reproducible and individual for each patient during the entire study period. During short-term tests, pulmonary artery pressure was reduced from a mean (of all patients) of 68 [+ or -] 13 to 49 [+ or -] 11 mm Hg, with a mean total effective treatment time of 49 [+ or -] 8 min. Thereafter, pulmonary pressure returned to preinhalation levels before the next inhalation. Long-term tests showed similar results. During a total recorded time of 15,876 min, the vasodilator effect lasted 2,140 min, corresponding to 13% of the whole time span.
Conclusion: Our study provided new insights into the short-term and long-term effects of treatment with inhaled iloprost in patients with pulmonary hypertension. While there were no signs of tachyphylaxis, the improvement of central hemodynamics was much shorter than expected. Continuous hemodynamic monitoring with the IHM demonstrated the need to improve the treatment modalities of aerosolized iloprost in patients with pulmonary hypertension.
Key words: hemodynamic monitoring; iloprost inhalation; pulmonary hypertension
Abbreviations: [DELTA]p = difference between maxima pressure and minimal pressure; EPR = external pressure reference; IHM = implantable hemodynamic monitor; PA = pulmonary artery; PAH = pulmonary arterial hypertension; Pmax = maximal pressure; Pmin = minimal pressure. PVH = pulmonary venous hypertension; RV = right ventricle, ventricular
**********
Pulmonary arterial hypertension is a rare disease with a progressive course and a poor prognosis. (1) It is characterized by elevated pulmonary artery (PA) pressures and an increased pulmonary vascular resistance. Data from a large National Institutes of Health registry showed that the median survival time after diagnosis is < 3 years, (2) and that death is closely associated with progressive hemodynamic deterioration in these patients. Therefore, the therapeutic aim is to reduce PA pressure and pulmonary vascular resistance, and in turn to improve survival. Modern therapeutic options include oral anticoagulation, (3) calcium channel blockers, (3) and prostanoids, (1,4,5) including prostaglandin and prostacyclin and its derivatives. Prostacyclin has pharmacologic properties that bear some disadvantages for the patient. Among these, is the need of a continuous IV infusion with a portable pump and a central venous line with all the potential complications that pertain to such therapy. These shortcomings prompted efforts to develop a more convenient therapy for these patients.
Aiming to overcome the inconvenience of continuous IV infusion, Olschewski et al (6) first tested the application of inhaled iloprost in patients with severe pulmonary hypertension. The effect of inhaled iloprost (ie, reduction of pulmonary pressures) in this study lasted for 60 to 120 min, making the management of pulmonary hypertensive patients in an outpatient setting feasible. It has been shown that prostacyclin and iloprost have similar effects when administered IV or as an aerosol. (7) While inhaled iloprost still is considered to be an experimental approach, several investigators have tested it. The long-term application of inhaled iloprost is safe and has beneficial effects on PA pressure, pulmonary vascular resistance, cardiac output, and exercise capacity. (8-10) Thus, inhaled iloprost is considered to be an effective and convenient treatment for patients with pulmonary hypertension. Very recently, it has been shown (10) that inhaled iloprost improves exercise capacity after 12 weeks of treatment compared with placebo.
The vasodilator effect of prostanoids in patients with pulmonary hypertension has been measured either by Swan-Ganz catheter or noninvasively by Doppler echocardiography. While both methods are accurate, they provide only momentary information about the hemodynamic state. Catheter investigations can be carried out only in the catheter laboratory or in the ICU and, therefore, do not reflect daily life conditions. This is of particular relevance for aerosol therapy, as its discontinuous application over a 24-h period makes continuous hemodynamic surveillance desirable.
Recently, an implantable hemodynamic monitor (IHM) [model 1; Medtronic Inc; Minneapolis, MN] has been introduced for the care of patients with congestive heart failure. In a 1-year feasibility study, (11) the accuracy and stability of its sensors, which are mounted on a lead implanted in the right ventricle (RV), was reported. The successor of this IHM (the Chronicle, model 9520; Medtronic Inc) has been tested and validated in a 12-month multicenter study. (12) The device showed excellent longterm accuracy for all pressure parameters over time. Furthermore, it has been tested in patients with congestive heart failure and has provided new insights into central hemodynamics during the withdrawal of diuretics. (13)
In the current study, which has been part of a multicenter investigation of this new implantable hemodynamic monitor (IHM), we report on the findings in patients with pulmonary hypertension who were undergoing long-term treatment with inhaled iloprost. We were interested in the feasibility of the five implantable hemodynamic monitor devices that were available for our center in these patients and tried to collect new information about the therapeutic efficacy of aerosolized iloprost in patients with pulmonary hypertension.
MATERIALS AND METHODS
Study Patients
We studied five patients (mean [[+ or -] SEM] age, 45 [+ or -] 16 years; all women) with known pulmonary hypertension that had been diagnosed by right heart catheterization. Four patients were experiencing pulmonary arterial hypertension (PAH), and one patient was experiencing pulmonary venous hypertension (PVH).
All patients were receiving treatment with inhaled iloprost (Schering; Berlin, Germany). This treatment regimen had been started prior to the inclusion of the patients into this study. The response to aerosolized iloprost had been demonstrated previously by right-heart catheterization. A positive response to inhaled treatment was defined as a reduction in PA pressure of at least 20% from baseline levels. (5) All patients were treated with a daily close of 100 [micro]g iloprost, which was divided into five or six inhalations given every 4 h without disruption of sleep at night. Iloprost was diluted in 0.9% NaCl and was inhaled using a standard jet-nebulizer (Master Drop; MPV Truma; Munich, Germany). The nebulizer provided an aerosol with a particle size of 3 [micro]m. All patients were in stable condition when entering the study.
Patients with pulmonary or tricuspid stenosis, or ventricular septal defect, or patients with a high probability for the need for a permanent pacemaker (AV block of > 1 [degrees]) were not included. The local ethics committee approved the stud), protocol, and written informed consent was obtained from all study participants.
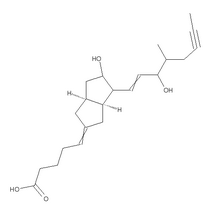
Device Description
The IHM (Fig 1) contained a random access memory (128 kB RAM) that continuously stored heart rate, patient activity, and RV pressure variables. Among others, RV systolic pressure (which is, in the absence of pulmonary stenosis, equivalent to PA systolic pressure), RV diastolic pressure, pulse pressure, and peak positive time derivative of the pressure curve were collected. The latter was used to determine an estimate of the PA diastolic pressure (defined as the RV pressure at the time of pulmonary valve opening), which is associated with the time of the peak positive time derivative of the pressure curve. (14) Data storage intervals ranged from 2 s (for a data set obtained during 4 h of monitoring) to 1 h (for 3 months of data). A variation of settings between those two intervals could be selected (ie, 52 s for a data set obtained during 1 full day). During each interval, hemodynamic variables were measured for each heart cycle. The values of each measurement were placed in a temporary histogram that was constructed over the entire storage interval. At the end of the storage interval, the values for the median and the 5th to 95th percentile range were saved, and the collection of values for the next storage interval were started. The memory allotted for data storage was the same for all storage intervals. When the data were not retrieved and the memory was not cleared, the data were overwritten starting with the oldest data sets.
[FIGURE 1 OMITTED]
The RV lead (model 4328A; Medtronic Inc) contained a pressure sensor located 30 mm proximally from the lead tip. The tip had a platinum unipolar electrode for sensing myocardial depolarization with tines for passive fixation. To correct the cardiac pressures for changing ambient pressures, an external pressure reference (EPR) device (model 2955 HF; Medtronic Inc) continuously measured and stored the barometric pressure once every minute. The EPR records were synchronized in time with the IHM. A programmer (model 9790; Medtronic Inc) retrieved data from both the IHM and EPR, and, in doing so, the barometric pressures recorded were automatically subtracted from the absolute cardiac pressure levels measured by the IHM, thereby providing the corrected physiologic readings. Data retrieval using the programmer was fully automated. The programmer also displayed real-time pressure waveforms and allowed for the adjustment of the IHM settings. Finally, the EPR contained a magnet that, in our study, allowed the patients to precisely mark the beginning and the end of an inhalation cycle.
The IHM and the lead connected were implanted using the same techniques as those for a standard pacemaker implantation. The lead was placed transvenously in the RV, and the preferred position of the tip was the RV outflow tract or a high septal location (Fig 2). The IHM typically was placed in the subclavian position.
[FIGURE 2 OMITTED]
Study Protocol
All patients underwent the following two protocols: the shortterm and the long-term.
The aims of the short-term protocol were the documentation of the vasodilator capacity of inhaled iloprost in an outpatient setting and the measurement of the timespan of this effect. For this protocol, the storage interval of the IHM was set to 2 s. Each test of the short-term protocol started at least 20 min before a standard inhalation of iloprost and ended approximately half an hour after the second inhalation, which gave us one full inhalation cycle (4 h) for analysis. The short-term protocol tests were performed the day before patients were discharged from the hospital (ie, one day after the implantation of the device) and after 1, 2, and 3 months during regular outpatient checkups.
The aims of the long-term protocol were the documentation of the vasodilator capacity of inhaled iloprost in ambulatory patients during an entire day at home. For this protocol, the storage interval of the IHM was set to 52 s. This setting usually provided between 20 and 26 h of pressure tracings to analyze including four to six inhalations. The long-term protocol tests were performed the day after the implantation of the device and after 2 and 5 months during regular outpatient checkups. At these outpatient visits, the device was programmed as described above. The following day, patients came back so that data could be collected from the memory of the device.
For both the short-term and the long-term protocols, patients were asked to use the magnet in the EPR to mark the start of each inhalation cycle.
Analysis of the Pressure Tracings
The data retrieved from the IHM were copied into a spreadsheet (Excel; Microsoft; Redmond, WA). For further analysis, the data were converted into line graphs using the same spreadsheet program.
The principals of the expected pressure changes after the inhalation of iloprost are depicted in Figure 3. A stable pressure plateau was found before the start of each inhalation, followed by a rapid drop in pressures after the inhalation of iloprost. As reported earlier by Olschewski et al, (6) this effect should last for 60 to 120 min. Thereafter, a rise to preinhalation pressures was seen before a new cycle started with a second inhalation.
[FIGURE 3 OMITTED]
Since no automatic evaluation was available, we used a semi-quantitative analysis of the line graphs. A flat, straight line was drawn parallel to the x-axis through the last 10 min of RV systolic pressure before the start of an inhalation. The value at which this line crossed the y-axis provided the value of the maximal stable pressure before inhalation (Pmax). After starting inhalation, the pressure tracing showed a rapid reduction of pressure to a lower level, called the minimal stable pressure after inhalation (Pmin). In a similar manner, we put a flat, straight line parallel to the x-axis through the line graph and used the value at which this line crossed the y-axis as the Pmin (Fig 4).
[FIGURE 4 OMITTED]
The time of effective pulmonary vasodilatation was arbitrarily defined as the sum of the time at Pmin plus the time from the end of Pmin until 50% of the initial pressure decrease had vanished and pressure levels were rising again to preinhalation levels (Fig 3).
Statistical Analysis
Since our study population consisted of only five individuals, only descriptive statistical analysis was performed. The data from the short-term protocol were averaged for each patient (four time points, as follows: prehospital discharge; month 1, month 2, and month 3) and were given as the mean [+ or -] SEM. Data from the long-term protocol were averaged for each patient (three time points, as follows: prehospital discharge, month 2, and month 5) and were given as the mean [+ or -] SEM.
RESULTS
The implantation of the device was performed at first attempt in all patients without complications. All patients left the hospital within 2 days after undergoing the procedure and completed the study period without adverse events.
Within minutes after the implantation of the device, pressure data were available. These data were compared with those from the invasive measurements obtained during right-heart catheterization at the beginning of iloprost inhalation, which took place between 6 and 25 months prior to the implantation of the IHM, as follows: patient 1, 16 months; patient 2, 19 months; patient 3, 25 months; patient 4, 6 months; and patient 5, 19 months. We observed that in patients 1 and 2 the Pmax was comparable with those from the results of the Swan-Ganz catheterization, in patients 3 and 4 there was an increase in Pmax between these two time points, and in patient 5 there was a marked decrease in pulmonary pressure from the time of the Swan-Ganz catheter until inclusion in this study.
Short-term Protocol
For each patient, the mean data from all shortterm recordings are given in Table 1. We found all degrees of pulmonary hypertension, varying from mild (mean systolic PA pressure, 45 mm Hg) to severe (mean systolic PA pressure, 119 mm Hg).
All patients responded favorably to therapy with inhaled iloprost, which is expressed by a reduction of PA systolic pressure after inhalation (Pmin). Again, the pressure response varied considerably between patients. While one patient had nearly normal pressure levels after iloprost inhalation (patient 2, 27 mm Hg), other patients had markedly elevated pressures, ranging from 36 to 92 mm Hg.
Surprisingly, the time at Pmin levels was rather short, varying between 17 and 48 min. This was followed by a steady return to preinhalation pressure levels. The end of effective vasodilatation was defined by RV systolic pressures crossing the line of 50% of the difference between Pmax and Pmin ([DELTA]p). The total effective treatment time varied from 29 to 80 min.
Figure 4 shows a pressure tracing from a shortterm test (patient 1). The shape of each patient's tracings was consistent over the course of the study period.
Long-term Protocol
The mean data from all long-term recordings are given in Table 2.
All patients showed long-term Pmax and Pmin responses to inhaled iloprost, with a reduction of PAP comparable to the short-term protocol responses.
Interestingly, the mean time at Pmin was longer in the short-term protocol than in the long-term protocol. In the latter, the stable time spent at lower pressure levels was only 19 min (the average of all patients), while in the short-term protocol this time was considerably longer (31 min for all patients). As a consequence of this, the total effective treatment time was shorter in the long-term protocol than in the short-term protocol.
During long-term protocol, 15,876 min of data were recorded. According to the definition of loss of vasodilator capacity after the inhalation of iloprost, we found a total duration of effective pulmonary vasodilatation of 2,140 min, representing 13% of the total recorded time.
Figure 5 shows a pressure tracing from a longterm test (patient 2). Again the shape of each patient's tracings was consistent over the course of the study period.
[FIGURE 5 OMITTED]
DISCUSSION
Our study clearly has shown that the IHM provided unique short-term and long-term information when used in patients with pulmonary hypertension. For iloprost inhalation, the total effective pulmonary vasodilatation time was much shorter than that anticipated from previous reports.
Inhaled Iloprost in Pulmonary Hypertension
For > 10 years, prostacyclin infusion has been the standard treatment for patients with pulmonary hypertension. (1) The continuous infusion of prostacyclin has been used successfully to improve pulmonary hemodynamics, and, consequently, the long-term prognosis in these patients has improved. (1,3-5) However, this treatment has several serious drawbacks, most importantly the need for a central venous line to administer the drug by continuous infusion. Furthermore, many patients develop tolerance to this form of treatment, resulting in the need to increase the dose of prostacyclin progressively. Consequently, new therapeutic options have been investigated, such as the IV application of the stable prostacyclin analog iloprost (5) and, much more conveniently, the application of aerosolized iloprost. (6,7)
The results of iloprost inhalation are highly promising. The route of application is convenient and without major risks for the patients, while the duration of pulmonary vasodilation is long enough to be applied discontinuously (ie, 60 to 120 min). (6) Consequently, many investigators have focused on therapy with inhaled iloprost. They have found (15) that the inhalation of iloprost causes an improvement of pulmonary hemodynamics and of oxygen uptake during exercise. Furthermore, the acute hemodynamic improvement of inhaled iloprost lasts for 3 months and is accompanied by an improvement of the distance walked in 6 min. (9,10) Moreover, the long-term application of aerosolized iloprost leads to a permanent reduction of PA pressures after 12 months of treatment. (8)
In contrast to these investigations, a series of eases published recently (16) has raised doubts about the potential of inhaled iloprost to replace IV prostacyclin in the treatment of patients with pulmonary hypertension. The vasodilatation caused by aerosolized iloprost lasted < 30 min and had, therefore, no potential to replace prostacyclin as therapy in patients with severe pulmonary hypertension. (16)
The results of our study are in line with these observations. While no patient has shown signs of tachyphylaxis, the duration of the response to iloprost has been much shorter than expected. In contrast to a time span of 60 to 120 min that had been reported earlier, (6) the duration of pulmonary vasodilatation in our study varied from 17 to 48 min. Although we have defined the end of pulmonary vasodilatation arbitrarily, the pressure tracings are very similar to those published by the Vienna group. (16) Furthermore, the lack of prolonged treatment effects is reflected by the rather short time of effective treatment that was seen in only 13% of the total recorded time.
We can speculate about the possible reasons for these findings. Since iloprost causes a marked reduction of pulmonary pressures, it is undoubtedly effective when administered as an aerosol. Hence, the explanations for the short time of therapeutic effects must include the possibility that, first, the currently used dosage of iloprost is not high enough and, second, that the jet nebulizer could be more effective in providing smaller aerosolized particles.
The IHM in Pulmonary Hypertension
The IHM was introduced initially to monitor RV hemodynamics in patients with heart failure. The accuracy of the system has been demonstrated recently. (11) Data from the IHM and from invasive pressure measurements using a Swan-Ganz-catheter show highly significant correlations, making the IHM data a reliable noninvasive tool for measuring RV pressures. Furthermore, the successor to the first IHM (the Chronicle) has very recently been validated for use in patients with heart failure. (12) The system, which was the same as that used in our study, provided useful information in patients undergoing a stepwise withdrawal from therapy with diuretics. (13)
Our current study demonstrates the feasibility of the IHM to monitor RV pressures in patients with pulmonary hypertension who were undergoing treatment with inhaled iloprost. For the first time, this approach has provided information about RV hemodynamics in patients who have been treated on an outpatient basis. Up to now, information about pulmonary pressures has been available either by performing Swan-Ganz catheterization or by using Doppler echocardiography. While both methods are accurate and, therefore, have been used frequently in patients with pulmonary hypertension, they usually provide snapshots of hemodynamic information. The IHM could expand our knowledge in these patients by providing new insights into central hemodynamics, as was seen in our patient population. Therefore, new parameters need to be defined such as the duration of pulmonary vasodilatation in response to specific treatment.
It is interesting to note that in four of five patients the duration of effective pulmonary vasodilatation was longer when it was performed in the hospital environment (ie, the short-term protocol in which patients could move around but were not allowed to leave the hospital) compared to the outpatient observations in the long-term protocol in which patients went back home after receiving treatment.
We can only speculate about possible causes. One possible explanation is the different resolutions of the IHM during short-term tests (2 s) and long-term tests (52 s). For ideal comparison, the long-term test should be performed using the 2-s resolution. Unfortunately, the memory of the device is limited, and tests taking a whole day cannot be performed with the 2-s resolution because the patient would be interrupted during the night to retrieve data and to clear the memory of the IHM (otherwise the oldest data would get lost).
Another explanation for the difference in pulmonary vasodilatation could be that patients were less active during the short-term tests in the hospital environment than they were during longterm tests at home. A third explanation could be that the inhalation technique used could be better performed while in the hospital environment than at home.
Currently, we can only speculate about possible explanations until we have a device available that has a larger amount of memory.
Limitations of the Study
Several limitations apply to our study, as follows:
1. The duration of pulmonary vasodilation was defined arbitrarily. While the hemodynamic response itself was defined earlier and was used by most investigators there is no clear definition of how long pulmonary vasodilation should last. Nevertheless, the length of this response should be defined more accurately, but continuous recording with a device that has more memory than is currently available will be necessary for this purpose.
2. The number of patients in our study is rather small and the degree of pulmonary hypertension was mild to moderate with a considerable variation in the response to the inhaled iloprost. Furthermore, the duration of this pulmonary vasodilation varied to a great extent.
3. Our patient population was highly selected. All patients showed a vasodilator response to inhaled iloprost. However, cardiac output may be a more important marker of drug response than pressure alone. Therefore, one should be careful in generalizing our findings to all patients treated with inhaled iloprost.
4. No information is available that would enable a comparison of our results with those from patients with severe forms of pulmonary hypertension. In the absence of relevant studies, we refrain from speculating on the possible differences.
CONCLUSION
Despite the limitations discussed, the IHM represents an important advance for monitoring patients with pulmonary hypertension. This study also shows that the duration of effectiveness of aerosolized vasodilator treatment with iloprost is shorter than that reported earlier. The 4-h inhalation interval especially does not seem to offer patients a permanent reduction of PA pressures with the equipment currently in use. Further studies are warranted to test better therapeutic options for these patients. These could include optimized inhalation equipment and the adaptation of iloprost dosing and/or inhalation intervals.
ACKNOWLEDGMENTS: We thank Helmut Mueller, MD, for implanting the IHM in our patients. We are indebted to Gabriele Pendl for her expert technical advice and to Jane Neuda for editorial review of the manuscript. Furthermore, we would like to acknowledge the help of Sabine Heintz, MD, and Stefan Mestel, MD, in analyzing the data.
REFERENCES
(1) Rubin LJ, Mendoza J, Hood M, et al. Treatment of primary pulmonary hypertension with continuous intravenous prostacyclin (epoprostenol): results of a randomized trial. Ann Intern Med 1990; 112:485-491
(2) Dacono GE, Barst RJ, Ayres SM, et al. Survival in patients with primary pulmonary hypertension: results from a National Prospective Registry. Ann Intern Med 1991; 115:343-349
(3) Rich S, Kaufmann E, Levy PS. The effect of high doses of calcium-channel blockers on survival in primary pulmonary hypertension. N Engl J Med 1992; 327:76-81
(4) Barst RJ, Rubin LJ, Long WA, et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. N Engl J Med 1996; 334:296-301
(5) Higenbottam TW, Butt AY, Dinh-Xaun AT, et al. Treatment of pulmonary hypertension with the continuous infusion of a prostacyclin analogue, iloprost. Heart 1998; 79:175-179
(6) Olschewski H, Walmrath D, Schermuly R, et al. Aerosolized prostacyclin and iloprost in severe pulmonary hypertension. Ann Intern Med 1996; 124:820-824
(7) Mikhail G, Gibbs JSR, Richardson M, et al. An evaluation of nebulized prostacyclin in patients with primary and secondary pulmonary hypertension. Eur Heart J 1997; 18:1499-1504
(8) Hoeper MM, Schwarze M, Ehlerding S, et al. Long-term treatment of pulmonary hypertension with aerosolized iloprost, a prostacyclin analogue. N Engl J Med 2000; 342: 1866-1870
(9) Olschewski H, Ghofrani A, Schmehl T, et al. Inhaled iloprost to treat severe pulmonary hypertension: an uncontrolled trial; the German PPH Study Group. Ann Intern Med 2000; 132:435-443
(10) Olschewski H, Simonneau G, Galie N, et al. Inhaled iloprost for severe pulmonary hypertension. N Engl J Med 2002; 347:322-329
(11) Ohlsson A, Kubo SH, Steinhaus D, et al. Continuous ambulatory monitoring of absolute right ventricular pressure and mixed venous oxygen saturation in patients with heart failure using an implantable haemodynamic monitor: results of a 1 year feasibility study. Eur Heart J 2001; 22:942-954
(12) Magalski A, Adamson P, Gadler F, et al. Continuous ambulatory right heart pressure measurements with an implantable hemodynamic monitor: a multicenter, 12-month follow-up study of patients with chronic heart failure. J Card Fail 2002; 8:63-70
(13) Braunschweig F, Linde C, Eriksson MJ, et al. Continuous haemodynamic monitoring during withdrawal of diuretics in patients with congestive heart failure. Eur Heart J 2002; 23:59-69
(14) Reynolds DW, Bartelt N, Raepke R, et al. Measurement of pulmonary artery diastolic pressure from the right ventricle. J Am Coll Cardiol 1995; 25:1176-1182
(15) Wensel R, Opitz DF, Ewert R, et al. Effects of iloprost inhalation on exercise capacity and ventilatory efficiency in patients with primary pulmonary hypertension. Circulation 2000; 101:2388-2392
(16) Schenk P, Petkov V, Madl C, et al. Aerosolized iloprost therapy could not replace long-term IV epoprostenol (prostacyclin) administration in severe pulmonary hypertension. Chest 2001; 119:296-300
* From the Department of Medicine (Drs. Fruhwald, Watzinger, Maier, and Klein), Division of Cardiology, Karl-Franzens University, Graz, Austria; Medtronic Bakken Research Center (Ms. Kjellstrom and Mr. Grandjean), Maastricht, the Netherlands; and Medtronic Austria (Dr. Perthold), Vienna, Austria.
Ms. Kjellstrom, Mr. Perthold, and Dr. Grandjean are employees of Medtronic.
Manuscript received April 23, 2002; revision accepted October 9, 2002.
Correspondence to: Friedrich M. Fruhwald, MD, Department of Medicine, Division of Cardiology, Auenbruggerplatz 15, A-8036 Graz, Austria; e-mail: friedrich.fruhwald@uni-graz.at
COPYRIGHT 2003 American College of Chest Physicians
COPYRIGHT 2003 Gale Group