Study objectives: Aerosolized iloprost, a stable prostacyclin analog, improves functional capacity even in patients with pulmonary hypertension who did not show a vigorous hemodynamic response after iloprost inhalation at rest. We therefore speculated that aerosolized iloprost elicits more beneficial effects on pulmonary hemodynamics during exercise than at rest.
Design and setting: A prospective, open, uncontrolled study at a university hospital.
Patients: Sixteen patients with primary or secondary pulmonary hypertension.
Interventions: Right-heart catheterization at rest and during exercise before and after the inhalation iloprost, 14 to 28 [micro]g.
Results: Before iloprost treatment, exercise increased mean ([+ or -] SD) pulmonary artery pressure (PAPm) from 45 [+ or -] 8 to 70 [+ or -] 13 mm Hg, cardiac output from 3.7 [+ or -] 1.0 to 5.8 [+ or -] 2.4 L/min, and pulmonary vascular resistance (PVR) from 904 [+ or -] 322 to 1,013 [+ or -] 432 dyne*s*[cm.sup.-5] (each p < 0.05). After recovery, iloprost reduced PAPm from 44 [+ or -] 8 to 41 [+ or -] 6 mm Hg, increased cardiac output from 3.7 [+ or -] 1.0 to 4.9 [+ or -] 1.4 L/min, and lowered PVR from 902 [+ or -] 350 to 636 [+ or -] 248 dyne*s*[cm.sup.-5] (each p < 0.05). During exercise after iloprost, PAPm increased to 57 [+ or -] 8 mm Hg, cardiac output to 7.0 [+ or -] 3.0 L/min, and PVR to 673 [+ or -] 279 dyne*s*[cm.sup.-5] (each p < 0.05 vs first exercise test). Systemic BP was not altered significantly by iloprost treatment during exercise.
Conclusions: Aerosolized iloprost treatment exerts more favorable effects on pulmonary hemodynamics during exercise than at rest. These findings explain the functional improvement observed in patients with pulmonary hypertension who show only a moderate pulmonary vasodilatory response during iloprost inhalation at rest. Whether these beneficial effects have prognostic significance needs to be elucidated by further study.
Key words: exercise test; hypertension; prostaglandins; pulmonary
Abbreviations: NYHA = New York Heart Association; PAPm = mean pulmonary artery pressure; PPH = primary pulmonary hypertension; PVR = pulmonary vascular resistance
**********
Primary pulmonary hypertension (PPH) is a rare disorder of unknown cause that is characterized by a progressive elevation of pulmonary artery pressure and pulmonary vascular resistance (PVR), often leading to right ventricular failure and death. (1,2) In contrast to PPH, the so-called secondary forms of pulmonary hypertension are related to disorders such as congenital heart disease, thromboembolic disease, chronic lung disease, collagen vascular disease, liver disease, or pulmonary veno-occlusive disease. (3) However, regardless of the etiology, prolonged pulmonary vasoconstriction has been suggested to be an important pathogenetic factor in all forms of pulmonary hypertension, and thus pulmonary vasodilation is a major aim in the treatment of the disease.
Prostacyclin is a potent, short-acting vasodilator with inhibitory effects on platelet aggregation that decreases PVR and increases cardiac output when administered short-term to patients with PPH or secondary pulmonary hypertension. (4,5) Moreover, continuous infusion of prostacyclin has been demonstrated to improve pulmonary hemodynamics and to prolong survival even in patients who did not respond to conventional vasodilator therapy. (6-10) The use of continuous IV prostacyclin, however, is often restricted by its potentially serious side effects and complications such as catheter infection, accidental discontinuation of prostacyclin infusion, systemic hypotension, worsening of ventilation-perfusion mismatch, and its extremely high cost. (6,7)
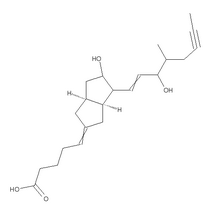
Aerosolized iloprost, a stable prostacyclin analog, seems to overcome some of these limitations inasmuch as it has been shown that short-term as well as long-term treatment improves pulmonary hemodynamics without clinically relevant effects on systemic BP or gas exchange at rest. (11-16) Moreover, short-term treatment with inhaled iloprost has been shown to improve exercise capacity even in patients with pulmonary hypertension who did not show a vigorous hemodynamic response after iloprost inhalation at rest. (16) This is an important observation, since exercise intolerance and dyspnea during exertion are major findings in all forms of pulmonary hypertension, and previous studies (2,6,8,17) have clearly demonstrated that functional capacity and performance on exercise tests have a strong prognostic significance.
However, the effects of aerosolized iloprost on the hemodynamic response to exercise have not yet been investigated. Nevertheless, based on the abovementioned results, we speculated that aerosolized iloprost elicits more favorable effects on pulmonary hemodynamics during exercise than at rest. To test this hypothesis, we performed right-heart catheterization in patients with PPH and various forms of secondary pulmonary hypertension at rest and during consecutive cycle ergometry tests before and after the inhalation of iloprost.
MATERIALS AND METHODS
Patients
We studied eight consecutive patients (six women and two men) who fulfilled the diagnostic criteria of the National Institutes of Health registry for PPH, (1) and eight consecutive patients (three women and five men) with secondary pulmonary hypertension. The underlying causes of secondary pulmonary hypertension included CREST syndrome (calcinosis, the Raynaud phenomenon, esophageal dysfunction, sclerodactyly, and telangiectasia; n = 1), surgically repaired ventricular septal defect (n = 1), pulmonary veno-occlusive disease (n = 1; the diagnosis was confirmed by open-lung biopsy; iloprost inhalation was well tolerated by this patient throughout the study), and peripheral thromboembolic pulmonary hypertension (n = 5). Patients were referred to our institution either for evaluation of pulmonary hypertension (n = 9) or follow-up examination during long-term treatment with aerosolized iloprost (four patients with PPH and three patients with secondary pulmonary hypertension; daily dose, 50 [micro]g to 150 [micro]g; mean treatment period, 15 months; range, 11 to 24 months). Patients were excluded if they had a recent lung embolism, decompensated right-heart failure, left-heart ejection fraction < 50%, hemodynamically significant mitral or aortic valve disease, or pulmonary capillary wedge pressure > 15 mm Hg. Conventional therapy included diuretics, calcium-channel blockers, supplemental oxygen, and warfarin. The study protocol was approved by the local ethics committee, and all patients gave written informed consent.
Study Protocol
Right-heart catheterization was performed using standard techniques. Cardiac output was measured in triplicate by the thermodilution technique. Stroke volume was determined by dividing cardiac output by heart rate. Cuff BP was obtained from the right or left brachial artery. Hemodynamic variables were measured at five points: (1) after the establishment of steady-state conditions at rest (Rest 1); (2) during the last minute of a 5-min, 45 [degrees]-upright cycle ergometry test with a constant external workload of 25 W or 50 W (Exercise 1); (3) at rest after recovery from exercise test 1 when the mean pulmonary artery pressure (PAPm) had stabilized to baseline levels again (Rest 2); (4) at rest 5 min after inhalation of iloprost (Rest 3); and (5) during the last minute of a second exercise test with the same duration and workload as the first test, starting within the first 10 min after cessation of the inhalation of iloprost (Exercise 2). For inhalation, 50 p,g of iloprost was diluted in 5 mL of isotonic saline solution and aerosolized by an ultrasonic nebulization device (Multisonic Compact; Schill GmbH; Probstzella, Germany) for 10 to 20 min, which resulted in a cumulative nominal dose of nebulized iloprost of 14 to 28 [micro]g (mean, 21 [+ or -] 5 [micro]g). Inhalation was stopped when patients experienced discomfort (thoracic oppression, flushing, headache) or until mean arterial pressure decreased to < 75 mm Hg. Supplemental oxygen was provided to all patients throughout the study at a constant flow rate between 2 L/min and 4 L/min.
Statistics
All results are presented as mean [+ or -] SD. Variables from patients with PPH and secondary pulmonary hypertension were compared using the Mann-Whitney test. The individual results at rest and during exercise before and after iloprost inhalation were compared using the Student's paired t test or the Wilcoxon signed-rank test. A p value < 0.05 was considered significant.
RESULTS
Patient Population and Baseline Data
Three patients with PPH were classified as New York Heart Association (NYHA) class II, and five patients with PPH were classified as NYHA class III. Two patients with secondary pulmonary hypertension were classified as NYHA class II, and six patients with secondary pulmonary hypertension were classified as NYHA class III. Patients with secondary pulmonary hypertension were significantly older than patients with PPH (Table 1). However, baseline hemodynamic parameters, as well as the mixed-venous oxygen saturation, were not significantly different between the two groups (Table 1). Moreover, both groups showed principally the same hemodynamic response to exercise and iloprost. Furthermore, there were no differences between the patients receiving iloprost for the first time and those who were already being treated with iloprost. Therefore, we analyzed the data of all study patients collectively.
Effects of Exercise Before Iloprost Inhalation
Table 2 summarizes the findings at rest and during the first exercise test in all study patients. During exercise, heart rate increased by 41 [+ or -] 14% (mean increase, 34.4 [+ or -] 9.6 beats/min; range, 24 to 63 beats/ min) and systemic BP increased by 12 [+ or -] 8% (mean increase, 11.4 [+ or -] 7.3 mm Hg; range, - 1 to 24 mm Hg). As expected, PAPm showed a marked increase of 58 [+ or -] 26% (mean, 25.6 [+ or -] 11.0 mm Hg; range, 13 to 44 mm Hg) during physical exertion. The increase in cardiac output of 54 [+ or -] 33% (mean increase, 2.1 [+ or -] 1.6 L/min; range, 0.3 to 5.4 L/min) was predominantly achieved by an increase in heart rate. Overall stroke volume did not change significantly (Table 2). PVR showed a small, but statistically significant increase of 12 [+ or -] 21% (mean increase, 108 [+ or -] 198 dyne*s*[cm.sup.-5]; range, - 225 to 481 dyne*s*[cm.sup.-5]). Moreover, the ratio of total pulmonary to total systemic resistance increased significantly during exercise from 0.48 [+ or -] 0.08 to 0.67 [+ or -] 0.12, respectively. The mixed-venous oxygen saturation decreased significantly during exercise by 28 [+ or -] 10 percentage points (Table 2).
Effects of Iloprost Inhalation at Rest
As outlined in Table 2, the variables at rest after recovery from the first exercise test (Rest 2) did not significantly differ from the baseline measurements (Rest 1). The effects of iloprost at rest are also shown in Table 2. Aerosolized iloprost induced a small, but significant increase in heart rate (2.7 [+ or -] 4.7 beats/ min; range, - 5 to 10 beats/min) and a slight but significant decrease in mean arterial BP (3.4 [+ or -] 4.4 mm Hg; range, - 11 to 7 mm Hg). PAPm was reduced by 6 [+ or -] 8% (mean, 2.9 [+ or -] 4.3 mm Hg; range, - 12 to 3 mm Hg), whereas cardiac output increased by 33 [+ or -] 21% (mean, 1.2 [+ or -] 0.8 L/min; range, 0.5 to 3.1 L/min), and stroke volume by 30 [+ or -] 23% (mean, 12.2 [+ or -] 9.7 mL; range, 1.3 to 36.1 mL). This resulted in a reduction in PVR of 28 [+ or -] 14% (mean, 266 [+ or -] 188 dyne*s*[cm.sup.-5]; range, 23 to 662 dyne*s*[cm.sup.-5]), and an increase in the mixed-venous oxygen saturation of 7 [+ or -] 5 percentage points (Table 2). However, the ratio of total pulmonary to systemic resistance was not significantly altered by iloprost treatment (Table 2).
Effects of Iloprost Inhalation During Exercise
Table 2 shows the effects of aerosolized iloprost during exercise. The increase in heart rate during exercise after inhalation of iloprost (27 [+ or -] 9%; mean, 23.3 [+ or -] 6.8 beats/min; range, 13 to 33 beats/min) was significantly lower than the increase during exercise without iloprost (p < 0.05). The absolute level of, and the relative rise in systemic BP during exercise (14 [+ or -] 8%; mean, 12.5 [+ or -] 6.6 mm Hg; range, 3 to 26 mm Hg; p < 0.05; Table 2) were not significantly altered compared to the respective results before iloprost inhalation. In contrast, aerosolized iloprost significantly attenuated the exercise-induced increase in PAPm compared to the respective increase observed during the first exercise test without iloprost (40 [+ or -] 19%; mean, 15.6 [+ or -] 6.9 mm Hg; range, 6 to 28 mm Hg after iloprost inhalation vs 58 [+ or -] 26% before iloprost; p < 0.05). Although the relative increase in cardiac output was significantly lower during the exercise test after iloprost inhalation (40 [+ or -] 29%) compared to the test before inhalation (54 [+ or -] 33%; p < 0.05), the absolute values for cardiac output were markedly increased following iloprost inhalation (5.8 [+ or -] 2.4 L/min before vs 7.0 [+ or -] 3.0 L/min after iloprost). In addition, stroke volume showed a significant increase during the exercise test after aerosolized iloprost (10 [+ or -] 20%; mean, 7.2 [+ or -] 13 mL; range, - 7.8 to 37.3 mL; p < 0.05). PVR did not significantly increase during the exercise test after iloprost inhalation. As compared to the exercise test before iloprost inhalation, PVR was significantly lower after aerosolized iloprost (31 [+ or -] 16%; mean, 339 [+ or -] 285 dyne*s*[cm.sup.-5]; range, - 94 to - 1,098 dyne*s*[cm.sup.-5]; Table 2). Moreover, the ratio of total pulmonary to systemic resistance during exercise decreased significantly after iloprost compared to the first exercise test (Table 2). Furthermore, the mixed-venous oxygen saturation during exercise was significantly higher after iloprost inhalation (10 [+ or -] 7 percentage points; Table 2).
Comparison of the Effects of Iloprost Inhalation at Rest and During Exercise
As compared to measurements at rest, aerosolized iloprost showed no significant effects on mean arterial BP during exercise (Table 2). Although the absolute levels for cardiac output were highest during the exercise test after iloprost inhalation (Table 2), the relative increase in cardiac output caused by aerosolized iloprost was not significantly different at rest and during exercise.
However, the relative reduction in PAPm induced by aerosolized iloprost was significantly greater during exercise (6 [+ or -] 8% at rest vs 18 [+ or -] 11% during exercise; p < 0.05), and the relative reduction in PVR tended to be higher during exercise (28 [+ or -] 14% at rest vs 31 [+ or -] 16% during exercise; p < 0.05). The changes in PAPm and PVR at rest and during exercise before and after aerosolized iloprost are summarized in Figures 1, 2.
[FIGURES 1-2 OMITTED]
DISCUSSION
Since its first description by Olschewski et al, (11) several studies (12-16) have demonstrated that short-term aerosolized iloprost elicits favorable effects on pulmonary hemodynamics without a significant decrease in systemic BP in patients with PPH or secondary pulmonary hypertension at rest. In contrast to these studies in which a cumulative dose of 14 to 17 [micro]g was used, we administered iloprost on a symptom-dependent basis, or until mean arterial pressure decreased to < 75 mm Hg. Thus, the cumulative dose of nebulized iloprost in our study was to somewhat higher, ranging from 14 to 28 [micro]g. This may be the reason why we found a slight but significant decrease in mean systemic arterial pressure after iloprost inhalation that was not observed in other studies. (11-16) However, the decline in BP was well tolerated by all patients.
Only limited data exist regarding the hemodynamic response to exercise in patients with pulmonary hypertension. (18) In contrast to normal subjects, patients with pulmonary hypertension exhibit a marked increase in pulmonary artery pressure during exercise, indicating that the capacity of the pulmonary vascular bed to vasodilate in response to an increase in blood flow is impaired under these conditions. (18) Furthermore, the exercise-induced increase in cardiac output in these patients is mediated primarily by an increase in heart rate, while the overall stroke volume remains unchanged. (18)
Calcium-channel blockers have been shown to reduce pulmonary artery pressure and PVR during exercise in selected patients with pulmonary hypertension. (19,20) Unfortunately, calcium-channel blockers produce sustained improvement in only 20 to 30% of patients, thereby limiting their widespread use. (21) Two patients with PPH were receiving concomitant calcium-channel blocker therapy with amlodipine, 5 mg/d, before being referred to our institution. This treatment was continued during the study period. However, we found no obvious differences with respect to the hemodynamic response to exercise and iloprost between these two patients and those without calcium-channel blockers. Thus, the treatment with calcium-channel blockers had no significant impact on the results of our study.
Our data demonstrate for the first time that aerosolized iloprost reduces pulmonary artery pressure and PVR, and increases cardiac output, stroke volume, and mixed-venous oxygen saturation during exercise in patients with PPH and different forms of secondary pulmonary hypertension, without significantly affecting mean arterial BP. As indicated by a marked reduction in both pulmonary artery pressure and PVR, which could not be observed at rest, iloprost-induced pulmonary vasodilation was even more pronounced during exercise. This finding explains why even those patients show an improvement in functional capacity after the inhalation of iloprost who do not exhibit a vigorous hemodynamic response during short-term drug testing at rest. (16)
We included patients with various forms of pulmonary hypertension and with different duration and severity of the disease in our study. Furthermore, some patients were already receiving long-term treatment with aerosolized iloprost while others were not. However, detailed analysis revealed no obvious differences in the response to exercise or iloprost between the different patient groups, indicating that aerosolized iloprost exerts its favorable effects over a large spectrum and wide range of pulmonary hypertension.
A possible limitation of our study is that our patients did not undergo a repeated control exercise test without iloprost, and thus we cannot exclude that the first exercise test may have had some conditioning effect on the second test. However, Muramoto et al (20) described no significant hemodynamic differences between two exercise tests performed 2 h apart in patients with chronic obstructive lung disease and pulmonary hypertension, making such an effect rather unlikely. Furthermore, we cannot rule out that the supplemental oxygen exerts a cumulative effect on the response to exercise. However, neither hemodynamics nor mixed-venous oxygen saturation changed significantly between the measurements Rest 1 and Rest 2, suggesting that such an effect is, again, rather unlikely.
Moreover, our study investigated the acute effects of aerosolized iloprost, and although this therapy has positive features, its practical use might be limited by its relatively short duration of action, lasting only from to 60 to 120 min. (11) Nevertheless, Hoeper et al (15) demonstrated that long-term treatment of patients with PPH with a daily dose of 100 to 150 [micro]g of aerosolized iloprost, divided into five to eight inhalations, is feasible. However, larger controlled clinical trials are needed to determine the role of aerosolized iloprost in the treatment of various forms of pulmonary hypertension. Therefore, inhaled iloprost cannot currently be recommended as a replacement therapy for continuous, infused prostacyclin, and its use should be considered exploratory.
In conclusion, in patients with pulmonary hypertension, aerosolized iloprost elicits more favorable effects on pulmonary hemodynamics during exercise than at rest without significant effects on the systemic circulation. These findings explain the functional improvement even in patients with pulmonary hypertension who do not show a vigorous hemodynamic response during iloprost inhalation at rest. Whether the beneficial effects on the hemodynamic response to physical exertion are accompanied by an improvement in the prognosis of patients with pulmonary hypertension needs to be elucidated by further study.
REFERENCES
(1) Rich S, Dantzker DR, Ayres SM, et al. Primary pulmonary hypertension: a national prospective study. Ann Intern Med 1987; 107:216-223
(2) D'Alonzo GE, Barst RJ, Ayres SM, et al. Survival in patients with primary pulmonary hypertension: results from a national prospective registry. Ann Intern Med 1991; 115:343-349
(3) Rubin LJ. Primary pulmonary hypertension. N Engl J Med 1997; 336:111-117
(4) Rubin LJ, Groves BM, Reeves JT, et al. Prostacyclin-induced acute pulmonary vasodilation in primary pulmonary hypertension. Circulation 1982; 66:334-338
(5) Bush A, Busst C, Booth K, et al. Does prostacyclin enhance the selective pulmonary vasodilator effect of oxygen in children with congenital heart disease? Circulation 1986; 74: 135-144
(6) Barst RJ, Rubin LJ, Long WA, et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension: The Primary Pulmonary Hypertension Study Group. N Engl J Med 1996; 334:296-302
(7) McLaughlin VV, Genthner DE, Panella MM, et al. Reduction in pulmonary vascular resistance with long-term epoprostenol (prostacyclin) therapy in primary pulmonary hypertension. N Engl J Med 1998; 338:273-277
(8) Higenbottam T, Butt AY, McMahon A, et al. Long-term intravenous prostaglandin (epoprostenol or iloprost) for treatment of severe pulmonary hypertension. Heart 1998; 80: 151-155
(9) McLaughlin VV, Genthner DE, Panella MM, et al. Compassionate use of continuous prostacyclin in the management of secondary pulmonary hypertension: a case series. Ann Intern Med 1999; 130:740-743
(10) Rosenzweig EB, Kerstein D, Barst RJ. Long-term prostacyclin for pulmonary hypertension with associated congenital heart defects. Circulation 1999; 99:1858-1865
(11) Olschewski H, Walmrath D, Schermuly R, et al. Aerosolized prostacyclin and iloprost in severe pulmonary hypertension. Ann Intern Med 1996; 124:820-824
(12) Olschewski H, Ghofrani HA, Walmrath D, et al. Inhaled prostacyclin and iloprost in severe pulmonary hypertension secondary to lung fibrosis. Am J Respir Crit Care Med 1999; 160:600- 607
(13) Hoeper MM, Olschewski H, Ghofrani HA, et al. A comparison of the acute hemodynamic effects of inhaled nitric oxide and aerosolized iloprost in primary pulmonary hypertension. German PPH Study Group. J Am Coll Cardiol 2000; 35: 176-182
(14) Olschewski H, Ghofrani HA, Schmehl T, et al. Inhaled iloprost to treat severe pulmonary hypertension: an uncontrolled trial; German PPH Study Group. Ann Intern Med 2000; 132:435-443
(15) Hoeper MM, Schwarze M, Ehlerding S, et al. Long-term treatment of primary pulmonary hypertension with aerosolized iloprost, a prostacyclin analogue. N Engl J Med 2000; 342:1866-1870
(16) Wensel R, Opitz CF, Ewert R, et al. Effects of iloprost inhalation on exercise capacity and ventilatory efficiency in patients with primary pulmonary hypertension. Circulation 2000; 101:2388-2392
(17) Miyamoto S, Nagaya N, Satoh T, et al. Clinical correlates and prognostic significance of six-minute walk test in patients with primary pulmonary hypertension: comparison with cardiopulmonary exercise testing. Am J Respir Crit Care Med 2000; 161:487-492
(18) Laskey WK, Ferrari VA, Palevsky HI, et al. Pulmonary artery hemodynamics in primary pulmonary hypertension. J Am Coll Cardiol 1993; 21:406-412
(19) Olivari MT, Levine TB, Weir EK, et al. Hemodynamic effects of nifedipine at rest and during exercise in primary pulmonary hypertension. Chest 1984; 86:14-19
(20) Muramoto A, Caldwell J, Albert RK, et al. Nifedipine dilates the pulmonary vasculature without producing symptomatic systemic hypotension in upright resting and exercising patients with pulmonary hypertension secondary to chronic obstructive pulmonary disease. Am Rev Respir Dis 1985; 132:963-966
(21) Rich S, Kaufmann E, Levy PS. The effect of high doses of calcium-channel blockers on survival in primary pulmonary hypertension. N Engl J Med 1992; 327:76-81
* From the Department of Internal Medicine II, University of Regensburg, Regensburg, Germany.
Manuscript received May 15, 2001; revision accepted September 28, 2001.
Correspondence to: Friedrich C. Blumberg, MD, Department of Internal Medicine II, University of Regensburg, 93042 Regensburg, Germany; e-mail: friedrich.blumberg@klinik.uni-regensburg.de
COPYRIGHT 2002 American College of Chest Physicians
COPYRIGHT 2002 Gale Group