If you want to know why migraine headaches are three times more prevalent in women than men, affecting an estimated one in five women, think hormones. (20)
**********
Researchers don't know for sure why reproductive hormones and migraines are so intertwined, says migraine expert Sarah DeRossett, MD, PhD, an assistant clinical professor of neurology at Emory University in Atlanta. She suspects it may be that the rise and fall of estrogen levels serves as a trigger for migraines in much the same way as red wine, aged cheese and flashing lights.
Consider these examples of a possible hormone-migraine link:
* Migraines are more common in boys before puberty.
* Migraines occur less often during the first trimester of pregnancy.
* While about 10 to 15 percent of female migraine sufferers have migraines only during their periods, the majority of women who have migraines experience them during their periods.
* The number of migraines usually declines and may cease altogether after menopause.
Under Diagnosed and Under Treated
Fewer than half of all patients who suffer from migraines receive the proper diagnosis. (21) The result? Significant disability for migraine sufferers, with the American Migraine Study II finding that 92 percent of women with severe migraine had some headache-related disability, and about half were severely disabled during an episode, requiring bed rest. (22)
The irony is that excellent treatments are available these days to not only relieve the migraine, but prevent it in the first place. Yet one 1999 study found that only four out of 10 people with migraines used prescription medication for their headaches. (21)
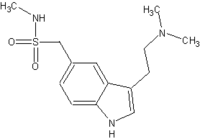
The most commonly prescribed medications for migraine are the triptans, a class of drugs first approved in the early 1990s. Today, there are seven triptans, including sumatriptan (Imitrex), zolmitriptan (Zomig) and eletriptan (Relpax). They work on serotonin receptors in the membranes covering the brain, constricting blood vessels to prevent the sensation of pain.
One thing many patients don't realize, says Dr. DeRossett, is that the triptans work best when taken at the first sign of a migraine. "People fiddle around a lot and under treat their headache (with over-the-counter drugs)," she says. By the time they turn to a stronger medication, it's too late to halt the headache before it hits full strength. So if you're prone to migraines, she recommends taking your prescribed medication at the first sign of pain; don't wait to "prove" that it's a migraine. (23)
For women with two or more headaches a week, a variety of preventive options are available. These include the anti-epileptic drugs topiramate (Topamax) and sodium valproate (Depakote), tricyclic antidepressants such as amitriptyline (Elavil) and nortriptyline (Pamelor), beta blockers such as propranolol (Inderal), calcium blockers such as verapamil, and the antihistamine cyproheptadine (Periactin) in children. (23)
Some headache experts also use Botox injections to prevent migraines, says Dr. DeRossett, with good success. And don't forget complementary and alternative medicine therapies like biofeedback and relaxation therapies. A 1990 meta-analysis comparing the effectiveness of relaxation/biofeedback with drug therapy (propranolol) found both cut the number of headaches by 43 percent. (12)
Certain lifestyle changes can also help prevent migraines. New studies find that obesity is independently associated with migraine, says Dr. DeRossett, so losing weight may help. Other studies find that emotional stress, lack of sleep or oversleeping, skipping meals, certain foods (aged cheese, preserved meats), alcohol (Particularly red wine and beer) and prolonged physical exertion can trigger migraines.
The main message for women, says Dr. DeRossett, is that migraines are very treatable, possibly preventable and almost always improve after menopause. If you've tried at least two preventative medications and are still having frequent headaches, and/or you still have debilitating migraines regardless of prescribed medications, it's time to see a headache specialist. Not only do they have access and knowledge about numerous drugs already on the market, they can often get you into clinical trials for new treatments. "There's more coming in the pipeline," Dr. DeRossett says. "This is going to be more and more of a treatable condition."
COPYRIGHT 2005 National Women's Health Resource Center
COPYRIGHT 2005 Gale Group