Practice recommendations
* Once a stroke patient has stabilized, if there is no contraindication, consider starting an antihypertensive agent regardless of the baseline blood pressure.
* For symptomatic patients with high-grade carotid stenosis (70% to 99%), plan a course of medical management plus carotid endarterectomy (CEA). With moderate carotid stenosis (50% to 69%), CEA offers only moderate stroke risk reduction.
* When aspirin is the antiplatelet drug of choice, it is reasonable to use daily doses between 50 mg and 325 mg.
For patients with atherosclerotic ischemic infarction, 3 steps are needed to achieve the goal of preventing recurrent stroke: address risk factors, clear blocked arteries, and thin the blood.
* Step 1: Address risk factors Risk factors that are non-modifiable put patients at highest risk for recurrent stroke and dictate more aggressive management measures.
Advanced age is the most serious nonmodifiable risk factor for stroke. (1) Risk of stroke in those older than 65 years is 16 to 25 times higher than the risk for younger people. (2)
Sex, family history, race, ethnicity, and geographic location also show a positive correlation with stroke incidence. Men are 1.25 times more likely to suffer stroke than women, (1) although women account for 60% of stroke fatalities (3) The "stroke belt," a cluster of 11 states in the southeastern United States, has considerably higher stroke mortality than the country as a whole. (4) African Americans are at greater risk for primary ischemic stroke and stroke mortality than are whites. (3)
TABLE 1 lists modifiable risk factors. (5) Studies show that even after a stroke, these factors are often not aggressively treated, with most patients falling outside guideline recommendations for treatment of at least 1 risk factor. (6) In risk management, the greatest benefit is in controlling hypertension.
Hypertension
Up to 50% of all strokes are attributable to hypertension, (1,7) making this the most commonly encountered modifiable risk factor. Risk of stroke rises proportionately with increasing blood pressure. Systolic levels of 160 mm Hg or higher, or diastolic levels of 95 mm Hg or higher, carry a relative risk of approximately 4. (1,7)
Even small reductions in blood pressure decrease the risk of stroke substantially. (9)
The Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure recently released its JNC 7 Report, (5) which says that increased risk for cardiovascular disease begins at systolic blood pressure of 115 mm Hg and diastolic blood pressure of 75 mg Hg.
The current recommendation for blood pressure control is <140/90 mm Hg, with tighter control (130/85 mm Hg) being prescribed for patients with diabetes. (8) The JNC 7 report established a new classification: prehypertension (120/80 mm Hg to 130/89). (5) For secondary stroke prevention, studies are under way to investigate the safety and efficacy of more aggressive medical management to target a systolic blood pressure target of 120 to 130 mm Hg.
Clinical trials with antihypertensive agents. Recent trials using various antihypertensive therapies have yielded apparently contradictory data. The only prospective randomized trial of antihypertensive agents focusing on secondary stroke prevention was the Perindopril Protection Against Recurrent Stroke Study (PROGRESS). It enrolled 6105 patients with a history of stroke or transient ischemic attack (TIA) within 5 years of randomization. Patients were randomized to receive placebo or perindopril with or without indapamide (added at the treating doctor's discretion) and were followed for 4 years. (9)
Patients in the treatment arm had a mean blood pressure reduction of 9/4 mm Hg. Relative risk reduction for stroke in the treatment arm was 28%. Stroke rate decreased by 43% (blood pressure reduction 12/5 mm Hg) for patients prescribed perindopril plus indapamide, while monotherapy with perindopril did not significantly reduce stroke rate. Benefit was found for patients not considered hypertensive at entry; the number of nonhypertensive patients needed to treat to prevent 1 major vascular event was 22. (10)
The Heart Outcomes Prevention Evaluation (HOPE) trial studied both primary and secondary stroke prevention, randomizing 9297 patients age 55 or over with high risk for vascular disease (coronary artery disease, stroke, peripheral vascular disease, or diabetes plus at least 1 other cardiovascular risk factor. (11) Patients were treated with ramipril or placebo and followed for 5 years. The ramipril arm had a mean blood pressure reduction of 3/2 mm Hg, and exhibited a statistically significant 31% relative risk reduction in stroke. The risk reduction appears to be out of proportion to the blood pressure reduction, suggesting additional benefit from the angiotensin-converting enzyme inhibitor independent of its antihypertensive effect.
In the Losartan Intervention for Endpoint Reduction (LIFE) trial, addressing primary prevention, 9193 hypertensive patients were randomized to receive losartan or atenolol and were followed for a mean of 4.8 years. (12) In the losartan arm, there was a 13% reduction in the combined endpoint of stroke, myocardial infarction (MI), and vascular death, with a 25% reduction in the rate of stroke despite a similar reduction in blood pressure in each arm.
In the largest of the trials, the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), 33,357 patients with hypertension and at least 1 other vascular risk factor were randomly assigned to receive chlorthalidone, amlodipine, or lisinopril, and were followed for 4.9 years. (15) No differences between treatments were found for the primary outcome (fatal coronary heart disease or nonfatal MI). In a head-to-head comparison of chlorthalidone and lisinopril, chlorthalidone yielded a 15% reduction in the rate of stroke.
Applying the evidence. Although no class of antihypertensive therapy is clearly superior to others for primary or secondary stroke prevention, it is clear that lowering blood pressure is effective.
Since most hypertensive stroke patients will require at least 2 agents to control blood pressure, using a thiazide diuretic or an agent to inhibit the renin-angiotensin system or both appears to be reasonable.
Once a stroke patient has stabilized, if there is no contraindication, consider starting an antihypertensive agent regardless of the baseline blood pressure. (16)
Hypercholesterolemia
In general, higher levels of low-density lipoprotein (LDL) cholesterol increase the risk of vascular disease. Multiple high-quality prospective randomized trials have demonstrated improved vascular outcomes for patients with coronary artery disease. (17) However, the direct link to secondary prevention after stroke is somewhat tenuous. (18)
Clinical trials with statin therapy. Several trials have reported a benefit with statin therapy for primary stroke prevention. The Scandinavian Simvastatin Survival Study (4S) was the first to demonstrate that lowering cholesterol with a statin drug can reduce the risk of stroke by 30% compared with placebo in patients with hypercholesterolemia at high risk for vascular disease. (19)
The Cholesterol And Recurrent Events (CARE) trial confirmed the benefit of statin therapy in reducing the rate of stroke in a population at high vascular risk. (20) In the CARE trial, pravastatin reduced the rate of stroke by 31% compared with placebo.
The Medical Research Council Heart Protection Study (HPS) randomized 20,536 high-risk patients to receive 40 mg simvastatin daily or placebo. (21) Researchers found a statistically significant 25% risk reduction in prespecified endpoint stroke with an even more impressive reduction of 30% in ischemic stroke. However, in the non-prespecified analysis of patients entering the trial with ischemic stroke or TIA, no benefit of statin therapy was found for secondary stroke prevention. (22)
Applying available recommendations. Trials are under way to prospectively test the benefit of statin therapy for secondary stroke prevention. (23) Until the results of those trials are available, guidelines are available to help with decision making. The NCEP III guidelines recommend a target LDL cholesterol level below 100 mg/dL for patients with symptomatic atherosclerotic disease. (24)
Cardiac risk factors
Atrial fibrillation (AF), valvular disease, coronary artery disease, and recent large MI increase the risk for stroke. Of these, AF shows the strongest association. AF increases with age and is found in 5.9% of patients older than 65 years. (4) It is present in more than one third of stroke patients older than 75 and is the most common cause of ischemic stroke in this age group. (25,26) Although much less common than nonvalvular AF, valvular AF poses an even greater risk. (7)
Applying the evidence. Prescribe warfarin for stroke patients with AF (see Anticoagulation, below). While there is a paucity of data on prevention in other causes of cardioembolic stroke, most patients with cardioembolic stroke may benefit from chronic anticoagulation.
Lifestyle risk factors
Cigarette smoking. Early studies on the association between cigarette smoking and stroke reported variable results. The Framingham Study, in a multivariate analysis, found that when hypertension and age are taken into account, smoking is a significant risk factor. (27) In a prospective study of 7735 men, Wannamethee and colleagues found benefit to stopping smoking, with light smokers dropping to the level of nonsmokers and heavy smokers dropping to about a twofold risk of nonsmokers in 5 years. (28) The benefit was greatest for hypertensive patients.
With the data now available, it is clear that cigarette smoking is a modifiable risk factor for ischemic infarction. Patients at risk for stroke should be given assistance in smoking cessation.
Alcohol use and abuse. The relationship between alcohol consumption and stroke risk is complex; risk with heavy use differs from that with light use. There may be racial differences in regard to alcohol risk and stroke.
Palomaki and colleagues found a protective effect of light alcohol use, with [less than or equal to]50 g/wk reducing the risk of ischemic stroke. (29) Data from the Framingham Study failed to show an association between alcohol consumption and ischemic stroke although there was a suggestion of reduced risk with wine. (30) While the data are not completely clear, it is reasonable to recommend avoiding heavy alcohol consumption as a measure of stroke risk reduction.
Physical activity. Regular exercise has been shown to reduce the risk of cardiovascular disease by decreasing blood pressure, reducing obesity, and improving glucose homeostasis, all of which should help reduce stroke risk.
Studies looking for an association between exercise and reduced stroke risk have produced mixed results. An evidence-based recommendation cannot be made. However, in view of the low cost and low risk of the intervention, instituting a program of progressive physical activity as part of a risk reduction program after stroke is a reasonable recommendation.
The American Heart Association's Guidelines for Primary Prevention of Cardiovascular Disease and Stroke from 2002 suggest there is a benefit from vigorous activity for 20 to 40 minutes, 3 to 5 days per week, if no medical contraindications exist. (31)
Diet. There is a paucity of good data regarding the potential protective effects of diet in secondary stroke prevention. Diets high in fruits and vegetables may have a protective effect against ischemic stroke. (32)
Current recommendations from the American Heart Association include 5 or more servings of fruits and vegetables per day, and 6 servings of grain products. (33) They recommend limiting foods with high content of cholesterol raising fatty acids and food high in cholesterol.
* Step 2: Clear blocked arteries Carotid stenosis
Carotid stenosis was recognized as an important risk factor for stroke in the 1950s. Carotid endarterectomy (CEA) was reported as a putative therapy shortly thereafter. The popularity of the surgery increased steadily through the mid-1980s despite an absence of evidence for the operation's safety or efficacy. Trials were organized in North America and Europe to test the surgery's potential risks and benefits. More recently, trials comparing CEA to angioplasty with and without stenting were organized.
Clinical trials with carotid endarterectomy/angioplasty, with or without stenting. Several multicenter trials have explored the benefit of CEA for symptomatic patients with varying degrees of ipsilateral carotid artery stenosis. These trials found a high degree of benefit for best medical management plus CEA compared with medical treatment alone for symptomatic patients with high-grade stenosis (70% to 99%), but only moderate stroke risk reduction with moderate carotid stenosis (50% to 69%). With mild stenosis (<50%), no benefit was found for surgical intervention. (34)
Even for patients with 70% to 99% stenosis, benefit can be eliminated by a high rate of perisurgical complications. (35) Surprisingly, CEA was also of little or no benefit for patients with symptomatic carotid near occlusion. (35)
Other factors influencing the relative benefit of CEA include gender (men benefit more than women), age [greater than or equal to] 75 years (older patients do better), and timing of surgery (maximum benefit when done within 2 weeks of the most recent symptoms). (36)
Devices for performing carotid angioplasty with or without stenting were recently approved by the Food and Drug Administration. However, this is a new technology that has not been proven superior to CEA for most patients with symptomatic stenosis.
Applying the evidence. Be sure all patients with severe or moderate stenosis receive appropriate surgical evaluation for CEA (TABLE 2). For symptomatic patients with very high-grade carotid stenosis and surgical risks so high that the surgeon believes CEA is not an option, carotid angioplasty and stenting can be considered. A recent trial found a trend toward non-inferiority for angioplasty and stenting compared with CEA in a high-risk population. However, widespread application of this technique should await completion of clinical trials testing it in more typical cerebrovascular patients.
Intracranial stenosis
Patients found to have ischemic stroke secondary to intracranial large artery stenosis or occlusion present a difficult therapeutic problem. An attempt to bypass the blocked artery was studied in a large prospective randomized trial of extracranial to intracranial bypass surgery. While the study remains controversial to this day, it failed to show any benefit for surgery compared with best medical management. (37) A study is now underway to examine whether patients selected for the procedure based on results of positron emission tomography will benefit.
Attempts to open stenotic and even occluded intracranial arteries have been reported in anecdotal series. However, the safety, efficacy, and durability of these procedures in this setting are speculative and should only be considered in exceptional circumstances.
Medical management of intracranial stenosis is also controversial. A retrospective study suggested that these patients may do better with anticoagulation compared with aspirin. However, a prospective randomized trial found that warfarin was no more effective than aspirin and increased risk. (38)
Applying the evidence. At this time, patients who have ischemic stroke due to large artery intracranial stenosis should be treated with best medical management including risk reduction and antithrombotic agents (see below). Bypass or angioplasty should be considered only if medical management fails.
* Step 3: Thin the blood Anticoagulation
Warfarin is appropriate for primary stroke prevention in many patients with AF and for secondary prevention in most AF patients with a history of embolic events. (10) For secondary prevention, warfarin is 68% better than placebo and significantly better than aspirin. (7) Appropriate timing of warfarin therapy following ischemic stroke or TIA is controversial. Some trials indicate that the risk without acute anticoagulation is fairly low in the first 2 weeks following an initial stroke, and that the risk of recurrent stroke does not diminish with anticoagulation.
Anticoagulation for secondary stroke prevention in patients with noncardioembolic stroke is an issue still unsettled. The Stroke Prevention In Reversible Ischemia Trial (SPIRIT) compared anticoagulants--phenprocoumon, acenocoumarol, or warfarin--(international normalized ratio [INR] = 3.0-4.5) with aspirin (30 mg daily) in the prevention of death from all vascular causes, nonfatal stroke, nonfatal MI, or nonfatal major bleeding complication. (39) A high rate of major bleeding complications in the anticoagulation arm led to early termination of this study. (39) The hazard ratio associated with the use of anticoagulants was 2.3 (95% confidence interval [CI], 1.6-3.5). Intracranial hemorrhage was the most frequently encountered bleeding complication.
The Warfarin-Aspirin Recurrent Stroke Study (WARSS) was conducted with 2206 patients who had suffered recent noncardioembolic ischemic strokes. (40) Dose-adjusted warfarin (INR = 1.4-2.8) was compared with aspirin 325 mg daily. (40) The primary end point of death or recurrent ischemic stroke occurred in 16.9% of patients. (40) No significant differences in efficacy were found between warfarin and aspirin. Safety profiles were similar as well, although patients taking warfarin had significantly more minor hemorrhages than did those in the aspirin group. (40) The Warfarin-Aspirin in Symptomatic Intracranial Disease trial compared dose-adjusted warfarin (INR = 2-3) with aspirin 1300 mg/d in 569 patients with symptomatic intracranial stenosis. They recently reported a recurrent stroke rate of 11% to 12% for each treatment arm, with a somewhat higher rate of hemorrhage in the patients receiving warfarin. (41)
Applying the evidence. Given the absence of data favoring warfarin for secondary stroke prevention in most ischemic stroke settings apart from cardioembolic stroke, using antiplatelet agents as a first line therapy is reasonable. Based on subset analysis of data from the WARSS trial, prescribing warfarin for patients who have failed aspirin is not a reasonable choice for most patients.
Antiplatelet agents
Aspirin. Aspirin both inhibits and promotes thrombogenesis. In its antithrombotic activity, aspirin inactivates platelet cyclooxygenase irreversibly--which, in turn, inhibits formation of thromboxane A2, a potent stimulator of platelet activation and vasoconstriction. This irreversible inhibition lasts for the lifespan of the platelet (about 7 to 10 days). Aspirin's pro thrombotic action comes from blocking production of endothelial prostacyclin, a prostaglandin that causes vasodilation and deaggregation.
Aspirin is the most commonly prescribed drug for prevention of secondary stroke. Yet, despite 21 randomized clinical trials involving more than 18,000 participants, consensus is lacking on many aspects of using aspirin for stroke prevention. In a meta-analysis of trials enrolling patients with previous TIA or stroke, treatment with antiplatelet agents compared with control reduced the rate of subsequent nonfatal stroke from 10.8% to 8.3%. (42)
Aspirin has significant gastrointestinal (GI) toxicity and causes GI bleeding. (43) The relative risk of developing peptic ulcer is 1.3, and symptoms of upper gastrotoxicity may cause withdrawal from aspirin treatment. (43) Hemorrhagic stroke increases with aspirin use, but for patients at risk for secondary ischemic stroke, aspirin's antithrombotic benefit outweighs the increased risk of hemorrhagic stroke (or GI toxicity). (44)
Aspirin dosing is controversial despite a large number of randomized, controlled trials. Faced with the same published papers and involvement in many of the same studies worldwide, experts fail to reach consensus on an optimal dose between 30 mg and 1500 mg. When aspirin is the antiplatelet drug of choice, absent data to show that higher dosing provides greater benefit, it is reasonable to use daily doses between 50 mg and 325 mg.
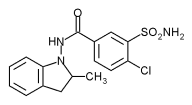
Ticlopidine. Ticlopidine is a thienopyridine derivative that irreversibly inhibits platelet aggregation by blocking the adenosine diphosphate (ADP) receptor, and it requires metabolism in the liver for this activity to take place. Ticlopidine, given 250 mg twice a day, inhibits platelet function within 24 to 48 hours of administration, peaks at 3 to 7 days, and lasts for the lifespan of the platelet.. (45) Bleeding time is doubled and remains prolonged for 4 to 10 days after the last dose.
The Ticlopidine Aspirin Stroke Study (TASS) examined the effects of ticlopidine 500 mg versus aspirin 1300 mg on the risk of stroke or death in 3069 patients with recent ischemic events. Ticlopidine was more effective than aspirin in reducing the risk of death from any cause or nonfatal stroke. (46) The risk of fatal or nonfatal stroke was reduced by 21% compared with aspirin. (46)
Subgroup analysis of TASS suggested a more favorable benefit-to-risk ratio for nonwhite patients compared with white patients. (47) In an attempt to validate this subgroup analysis, a second study, the African American Antiplatelet Stroke Prevention Study (AAASPS), randomized 1809 black patients with recent noncardioembolic stroke to receive ticlopidine 500 mg/d or aspirin 650 mg/d, and followed them for 2 years. The researchers reported no difference between the agents in the prevention of recurrent stroke, MI, or vascular death. (48)
Unfortunately, the clinical usefulness of this compound is limited by side effects. Diarrhea and skin rash, the most common side effects, were usually relieved by a temporary reduction in dose. However, severe reversible neutropenia occurred in nearly 1% of patients. (46) Potentially life threatening thrombotic thrombocytopenic purpura has also been associated with ticlopidine. The potential for a serious adverse event requires that patients be carefully monitored during the first 3 months of treatment. (46) This side effect profile makes ticlopidine a poor choice as a first line drug for secondary stroke prevention.
Clopidogrel. Like ticlopidine, clopidogrel is a thienopyridine derivative and blocks the ADP receptor. Clopidogrel's antiplatelet effect is dose-related, with 75 mg causing prolongation of bleeding time roughly equivalent to 500 mg of ticlopidine. After a loading dose of 300 mg, the onset of action is about 2 to 5 hours, and peak platelet inhibition occurs between 3 and 7 days. Like ticlopidine, bleeding time remains prolonged for 4 to 10 days after the last dose.
The Clopidogrel versus Aspirin in Patients at Risk of Ischemic Events (CAPRIE) trial evaluated clopidogrel (75 mg once daily) versus aspirin (325 mg once daily) in reducing the risk of the combined outcome of ischemic stroke, MI, or vascular death in more than 19,000 patients who entered the trial with recent ischemic stroke, recent MI, or symptomatic peripheral vascular disease. (49) A modest but statistically significant relative risk reduction of 8.7% was found for clopidogrel over aspirin (95% CI, 0.3-16.5; P = .043). For the subgroup of patients entering the trial with stroke, there was a risk reduction of 7.3 % favoring clopidogrel, but this did not reach statistical significance (95% CI,-5.7 to 18.7; P = .26).
The main adverse events experienced by patients taking clopidogrel were diarrhea and rash. Patients taking aspirin experienced gastrointestinal discomfort and, more seriously, a small but statistically significant increase in gastrointestinal hemorrhage. (49)
The Clopiclogrel in Unstable Angina to Prevent Recurrent Events (CURE) trial examined the effects of clopidogrel plus aspirin compared with aspirin alone on the combined end point of: (1) cardiovascular death, MI, or stroke; and (2) cardiovascular death, MI, stroke, or refractory ischemia in 12,562 patients with an acute coronary syndrome without ST segment elevation. (50) Combination antiplatelet therapy demonstrated a relative risk reduction of 20% (95% CI, 0.72-0.90; P<.001; absolute risk reduction [ARR] = 2.1%) and 16% (95% CI, 0.79-0.94; P<.001; ARR = 2.3%) for the 2 primary endpoints compared with aspirin alone. Major bleeding was significantly more common in the clopidogrel plus aspirin group (relative risk increase of 38%; 95% CI, 1.13-1.67; P = .001; absolute risk increase = 1%).
The applicability of the CURE trial findings to a stroke population is questionable, however. This trial addressed neither the efficacy nor the safety of this combination in a stroke population. Results were recently reported by the Management of Atherothrombosis with Clopidogrel in High Risk Patients with Recent Transient Ischemic Attack or Ischemic Stroke (MATCH) trial, which compared clopidogrel alone with clopidogrel plus aspirin in a population of patients with recent stroke or TIA plus 1 vascular risk factor. (51)
Researchers reported no significant difference in prevention of a combined vascular outcome or in preventing ischemic stroke alone. They did find a significant increase in life-threatening bleeding and major bleeding using the combination of aspirin and clopidogrel. Unfortunately, this trial did not address the issue of safety or efficacy of the combination of aspirin plus clopidogrel versus aspirin alone. The Stroke Prevention in Small Subcortical Strokes (SPS3) trial, an NINDS-funded study, will address this question, but the results of that trial are several years away.
Lau and colleagues (52) report that the platelet inhibition activity of clopidogrel was attenuated in patients undergoing coronary artery stent implantation and who were being treated with 10 to 40 mg of atorvastatin. Antiplatelet activity was significantly attenuated for up to 8 days after stent implantation in these patients, compared with clopidogrel alone.
Based on the data, clopidogrel is the first-line drug of choice for secondary stroke prevention for patients unable to take aspirin. The combination of aspirin and clopidogrel has increased risk without increasing efficacy and, therefore, is not a reasonable first-line choice for secondary stroke prevention.
Aspirin plus extended-release dipyridamole (ER-DP). Dipyridamole reversibly inhibits platelet activity by inhibiting both platelet phosphodiesterase and the uptake of adenosine. For the standard release formulation, the time to peak concentration varies from 34 to 75 minutes. (53) Standard-release dipyridamole falls below its therapeutic level about 6 to 8 hours after the last dose. And because its inhibition of platelet function is reversible, 3 to 4 daily doses of the drug are necessary to maintain the desired antiplatelet effect. (54) ER-DP reportedly requires twice daily dosing and achieves a therapeutic steady state after approximately 48 hours. Combining aspirin with ER-DP has the potential for taking advantage of the inhibition of the platelet cyclooxygenase and phosphodiesterase plus the platelet uptake of adenosine.
The second European Stroke Prevention Study (ESPS-2) investigated, in a population at high risk for stroke, the safety and efficacy of 4 antiplatelet strategies: (1) aspirin 25 mg twice daily; (2) extended-release dipyridamole 200 mg twice daily; (3) combination aspirin 25 mg plus extended-release dipyridamole 200 mg twice daily; (4) and placebo. (55)
Compared with placebo, aspirin alone reduced stroke risk by 18.1% (P = .013), dipyridamole alone by 16.3% (P = .039), and the combination agent by 37.0% (P<.001). The relative risk reductions for the combined end point of stroke or death were 13.2% (P = .016) with aspirin, 15.4% (P = .015) with dipyridamole, and 24.4% (P<.001) with the combination agent.
Headache and gastrointestinal disturbances were common adverse events in all treatment groups, but bleeding episodes were more frequent and severe only in the regimens that contained aspirin. (55) In the aspirin group, 8.2% of patients reported bleeding, while in the aspirin plus ER-DP group, 8.7% reported bleeding.
This was the first trial to demonstrate that very-low-dose aspirin is effective in preventing secondary stroke. (55) Efficacy was also found for extended-release dipyridamole as a single agent. The risk reduction achieved with the combination agent was approximately double that of either component alone. (55) Aspirin plus ER-DP reduced stroke risk by 23% over aspirin alone. (56)
In progress now are trials validating ESPS2, comparing clopidogrel plus aspirin with aspirin alone, and comparing combination aspirin plus ER-DP with clopidogrel.
Applying the evidence. Until these trials are complete, reasonable first-line choices for secondary stroke prevention are aspirin alone or in combination with ER-DP. For patients unable to take aspirin, consider giving clopidogrel alone.
DISCLOSURE
Dr Cohen has received grant/research support and has served on speakers' bureaus for Boehringer-Ingelheim Pharmaceuticals.
REFERENCES
(1.) Sacco RL, Benjamin EJ, Broderick JP, et al. American Heart Association prevention conference IV: Prevention and rehabilitation of stroke. Stroke 1997; 28:1507-1517.
(2.) Centers for Disease Control. Fastats. Available at: www.cdc.gov/nchs/fastats.
(3.) American Stroke Association. Heart disease and stroke statistics--2003 update. Dallas, Tex: American Heart Association; 2002.
(4.) Perry HM, Roccella EJ. Conference report on stroke mortality in the southeastern United States. Hypertension 1998; 31 : 1206-1215.
(5.)Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The JNC 7 Report. JAMA 2003; 289:2560-2572.
(6.) Cheng EM, Jolly D, Date L, Cohen SN. Inadequate control of modifiable risk factors a year after a stroke. J Stroke Cerebrovasc Disease, in press.
(7.) Sacco RL. Risk factors, outcomes, and stroke subtypes for ischemic stroke. Neurology 1997; 49(suppl 4):$39-$44.
(8.) Joint National Committee. The sixth report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med 1997; 24:2413-2446.
(9.) PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6105 individuals with previous stroke or transient ischaemic attack. Lancet 2001; 358:1033-1041.
(10.) van Gijn J. The PROGRESS trial: preventing strokes by lowering blood pressure in patients with cerebral ischemia. Stroke 2002; 33:319-320.
(11.) Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-convertingenzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med 2000; 342:145-153.
(12.) Dahlof B, Devereux RB, Kjeldsen SE, et al, and the LIFE Study Group. Cardiovascular morbidity and mortality in the losartan intervention for endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet 2002; 359:995-1003.
(13.) Vickrey BG, Rector TS, Wickstrom SL, et al. Occurrence of secondary ischemic events among persons with atherosclerotic vascular disease. Stroke 2002; 33:901-906.
(14.) American Heart Association. Heart Disease and Stroke Statistics--2005 Update. Dallas, Tex.: American Heart Association; 2005. Available at: www.americanheart.org/downloadable/heart/1105390918119HDSStats2005Update.pdf. Accessed on March 30, 2005.
(15.) ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288:2981-2997.
(16.) Bath P. Blood pressure-lowering for secondary prevention of stroke: ACE inhibition is not the key. Stroke 2003; 34:1334-1335.
(17.) Streja DA. Managing lipids in stroke patients. In Cohen SN (ed): Management of Acute Ischemic Stroke. New York: McGraw-Hill; 2000:119-132.
(18.) Boden-Albala B, Sacco RL. Modifiable risk factors for stroke: hypertension, diabetes mellitus, lipids, tobacco use, physical inactivity, and alcohol. In: Gorelick PB, Alter M (eds). The Prevention of Stroke. New York: Parthenon Publishing Group; 2002:21-37.
(19.) Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994; 344:1383-1389.
(20.) Sacks FM, Pfeffer MA, Moye LA, et al, and the Cholesterol and Recurrent Events Trial Investigators. The effect of pravastatin on coronary events after MI in patients with average cholesterol levels. N Engl J Med 1996; 335:1001-1009.
(21.) Heart Protection Study Collaborative Group. MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002; 360:7-22.
(22.) Coull BM. Statin therapy after acute ischemic stroke in the Heart Protection Study. Stroke 2004; 35:2233-2234.
(23.) The SPARCL Investigators. Design and baseline characteristics of the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Study. Cerebrovasc Dis 2003; 16:389-395.
(24.) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001; 285:2486-2497.
(25.) Hart RG, Sherman DG, Easton JD, Cairns JA. Prevention of stroke in patients with nonvalvular atrial fibrillation. Neurology 1998; 51:674-681.
(26.) Hart RG, Halperin JL. Atrial fibrillation and stroke. Stroke 2001; 32:803-808.
(27.) Wolf PA, D'Agostino B, Kannel WB, et al. Cigarette smoking as a risk factor for stroke. JAMA 1988; 259:1025-1029.
(28.) Wannamethee G, Perry I J, Sharper AG. Haematocfrit, hypertension and risk of stroke. J Intern Med 1994; 235:163-168.
(29.) Palomaki H, Kaste M. Regular light to moderate intake of alcohol and risk of ischemic stroke: is there a beneficial effect? Stroke 1993; 24:1828-1832.
(30.) Djousse L, Ellison RC, Beiser A et al. Alcohol consumption and risk of ischemic stroke: the Framingham Study. Stroke 2002; 33:907-912.
(31.) Pearson TA, Blair SN, Daniels SR, et al. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update: Consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation 2002; 106:388-391.
(32.) Joshipura KJ, Ascherio A, Manson JE, et al. Fruit and vegetable intake in relation to risk of ischemic stroke. JAMA 1999; 282:1233-1239.
(33.) Krauss RM, Eckel RH, Howard B, et al. AHA dietary guidelines: Revision 2000: A statement for healthcare professionals from the nutrition committee of the American Heart Association. Stroke 2000; 31:2751-2766.
(34.) Rothwell PM, Eliasziw M, Gutnikov SA, et al. Analysis of pooled data from the randomized controlled trials of endarterectomy for symptomatic carotid stenosis. Lancet 2003; 361:107-116.
(35.) Rothwell PM. Gutnikov SA, Warlow CP, for the European Carotid Surgry Trialists' Collaboration. Reanalysis of the final results of the European Carotid Surgery Trial. Stroke 2003; 34:514-523.
(36.) Rothwell PM, Eliasziw M, Gutnikov SA, et al. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 2004; 363:915-924.
(37.) EC/IC Bypass Study Group. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke: results of an international randomized trial. N Engl J Med 1985; 313:1191-1200.
(38.) Chimowitz MI., Lynn MJ, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med 2005; 352:1305-1316.
(39.) The Stroke Prevention In Reversible Ischemia Trial (SPIRIT) Study Group. A randomized trial of anticoagulants versus aspirin after cerebral ischemia of presumed arterial origin. Ann Neurol 1997; 42:857-865.
(40.) Mohr JP, Thompson JLP, Lazar RM, et al. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med 2001; 345:1444-1451.
(41.) Chimowitz M, Howell-Smith H, Stern B, et al, and WASID Investigators. Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) trial: final results. Stroke 2004; 35:235.
(42.) Antithrombotic Trialists' Collaboration. Collaborative meta-analysis of randomized trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002; 324:71-86.
(43.) Roderick P J, Wilkes HC, Meade TW. The gastrointestinal toxicity of aspirin: an overview of randomised controlled trials. Br J Clin Pharmacol 1993; 35:219-226. (44.) He J, Whelton PK, Vu B, Klag MJ. Aspirin and risk of hemorrhagic stroke. JAMA 1998; 280:1930-1935.
(45.) Quinn MJ, Fitzgerald DJ. Ticlopidine and clopidogrel. Circulation 1999; 100:1667-1672.
(46.) Hass WK, Easton JD, Adams HP, et al. A randomized trial comparing ticlopidine hydrochloride with aspirin for the prevention of stroke in high-risk patients. N Engl J Med 1989; 321:501-507.
(47.) Weissberg LA, for the Ticlopidine Aspirin Stroke Study Group. The efficacy and safety of ticlopidine and aspirin in non-whites: analysis of a patient subgroup from the Ticlopidine Aspirin Stroke Study. Neurology 1993; 43:27-31.
(48.) Gorelick PB, Richardson D, Kelly M, et al, and African American Antiplatelet Stroke Prevention (AAASPS) Investigators. Aspirin and ticlopidine for prevention of recurrent stroke in black patients. JAMA 2003; 289:2947-2957.
(49.) CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet 1996; 348:1329-1339.
(50.) Mehta SR, Yusuf S; Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) Study Investigators. The Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) trial programme; rationale, design and baseline characteristics including a meta-analysis of the effects of thienopyridines in vascular disease. Eur Heart J 2000; 21:2033-2041.
(51.) Diener HC, Bogousslavsky J, Brass LM, et al; MATCH investigators. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet 2004; 364:331-337.
(52.) Lau WC, Waskell LA, Watkins PB, et al. Atorvastatin reduces the ability of clopidogrel to inhibit platelet aggregation. A new drug-drug interaction. Circulation 2003; 107:32-37.
(53.) Mahony C, Wolfram KM, Cocchetto DM, Bjornsson TD. Dipyridamole kinetics. Clin Pharmacol Ther 1982; 31:330-338.
(54.) Dresse A, Chevolet C, Delapierre D, et al. Pharmacokinetics of oral dipyridamole (Persantine) and its effect on platelet adenosine uptake in man. Eur J Clin Pharmacol 1982; 23:229-234.
(55.) Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci 1996; 143:1-13.
(56.) Wilterdink JL, Easton JD. Dipyridamole plus aspirin in cerebrovascular disease. Arch Neurol 1999; 56:1087-1092.
FAST TRACK In managing risk for stroke, the greatest benefit is in controlling hypertension
The risks and costs of stroke
Stroke is the leading cause of adult disability, the second leading cause of dementia, and the third leading cause of death in the United States. Stroke survivors are at significantly increased risk for subsequent stroke, (13) with more than 75% of secondary vascular events being stroke. (3) Therefore, prevention of secondary stroke saves lives, prevents disability, and is a prudent allocation of medical resources. Direct costs attributable to stroke in the United States are estimated at $28.3 billion a year, with total costs greater than $50 billion. (3,14)
FAST TRACK Once the patient has stabilized, if there is no contraindication, consider starting an antihypertensive agent regardless of the baseline blood pressure
FAST TRACK Cigarette smoking is a modifiable risk factor for ischemic infarction
FAST TRACK Patients with severe or moderate stenosis should be considered for surgical evaluation for carotid endartectomy
FAST TRACK Anticoagulation for secondary stroke prevention in patients with noncardioembolic stroke is an unsettled issue
FAST TRACK When using aspirin as the antiplatelet drug of choice, use daily doses between 50 and 325 mg
FAST TRACK Because of its side-effect profile, ticlopidine is a poor choice as a first-line drug for secondary stroke prevention
FAST TRACK Reasonable first-line choices for secondary stroke prevention are aspirin alone or in combination with extended-release dipyridamole
Stanley N. Cohen, MD Cedars-Sinai Medical Center, Los Angeles, Calif
COPYRIGHT 2005 Dowden Health Media, Inc.
COPYRIGHT 2005 Gale Group