A 31-year-old woman presented at a community hospital with an episode of hemoptysis at the 22nd week of pregnancy. She had experienced progressive exertional dyspnea since the first trimester of her pregnancy. Her medical history was notable for a "heart condition" diagnosed at birth for which the patient had never sought follow-up care. In the evaluation of her hemoptysis, her physicians performed an echocardiogram that demonstrated pulmonary hypertension. She was referred to the National Taiwan University Hospital for the management of high-risk pregnancy. An admiring cardiologist prescribed diltiazem and indapamide for pulmonary hypertension, but her dyspnea did not improve. She was discharged from the hospital for outpatient care, and was noted to have a breech presentation and intrauterine growth retardation at the 27th week of pregnancy. Early delivery was recommended, and corticosteroids were administered to enhance fetal lung maturity. Subsequently, she was admitted for elective cesarean section at the 31st week of pregnancy.
Physical Examination
The patient's body temperature was 36[degrees]C, BP was 110/70 mm Hg, pulse was 96 beats/min, and respiratory rate was 22 breaths/min. The sclerae were not icteric. The neck was supple without jugular vein distension or lymphadenopathy. Chest auscultation revealed fine crackles over bilateral basal lung fields. A grade II/VI systolic murmur along the left sternal border without radiation was noticed. The abdomen was soft and flat without tenderness. The liver and spleen were not palpable. Digital clubbing and differential cyanosis were detected. When breathing room air, the pulse oximetry oxygen saturation in the fingers was around 85% to approximately 88%, while saturations in the toes were around 80% to approximately 82%.
Laboratory Findings
The arterial blood gas levels while breathing 15 L/min oxygen via a nonrebreathing mask showed a pH of 7.36, a Pac[0.sub.2] of 35 mm Hg, and a Pa[O.sub.2] of 61.6 mm Hg. There was marked polycythemia, with a hemoglobin concentration of 19.5 g/dL and a hematocrit of 56.7%. The serum urea, creatinine, and electrolyte levels were within normal limits. The ECG showed right-axis deviation and signs of right ventricular hypertrophy. An echocardiography demonstrated a type I ventricular septal defect with a bidirectional shunt. The pressure gradient of tricuspid valve regurgitation was 123 mm Hg. There was no hypokinesia in the left ventricle. The chest radiograph on hospital admission (Fig 1) and CT scans of the chest taken during hospitalization (Fig 2) are shown.
[FIGURES 1-2 OMITTED]
What is the most likely diagnosis?
Diagnosis: Pregnancy complicated by Eisenmenger syndrome due to interrupted aortic arch with ventricular septal defect and patent ductus arteriosus.
DISCUSSION
Both "simple" and "complex" congenital heart diseases can lead to Eisenmenger syndrome. Interrupted aortic arch, a complex congenital heart disease, is defined as the absence or discontinuation of a portion of the aortic arch and has been attributed to the faulty development of the aortic arch system during fetal development. Common manifestations are weakness, fatigue, tachycardia, tachypnea, increased work of breathing, and low oxygen saturations, with lower oxygen saturations measured in the legs and feet. This latter finding results in differential cyanosis. If the condition is left untreated, 90% of affected infants will die in the first year of life. Interrupted aortic arch is rarely encountered in adults, and presentation ranges from an asymptomatic incidental finding to Eisenmenger syndrome with severe pulmonary hypertension. Surgical intervention may be effective before the development of congestive heart failure. The development of pulmonary hypertension, however, requires medical intervention aimed at controlling symptoms and preventing complications.
The clinical course of pregnancy complicated by severe pulmonary hypertension still carries substantial maternal mortality. Several factors have been implicated as potential risk factors for maternal death, including high pulmonary artery pressure, elevated central venous pressure values, mode of delivery, type and technique of anesthesia, and manner of maternal monitoring. Under normal circumstances, increases in cardiac output in the range of 30 to 50%, blood volume in the range of 40 to 50%, and oxygen consumption of 20% are observed during pregnancy. The pain and valsalva maneuvers associated with labor increase right atrial pressure, BP, and cardiac output. These physiologic events can precipitate the signs and symptoms of pulmonary hypertension, such as dyspnea, cyanosis, hemoptysis, early fatigue, and syncope. Moreover, the large volume shifts at delivery and in the postpartum period place a great demand on the cardiovascular system, magnify time pulmonary resistance leading to right ventricular enlargement and right heart failure, resulting in a high maternal mortality. The reported maternal mortality rates are 36% in association with Eisenmenger syndrome, 30% with primary pulmonary hypertension, and 56% with secondary pulmonary hypertension.
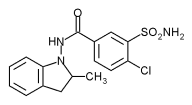
Management during the course of labor for women with Eisenmenger syndrome focuses primarily on the aggressive correction of the fluid and electrolyte imbalance, acidosis, hypoxemia, and arhythmia to prevent pulmonary vasoconstriction and thrombosis. In 1999, Robinson et al first reported the use of inhaled nitric oxide (NO) to reduce pulmonary artery pressure in a pregnancy complicated by pulmonary hypertension. This therapy was reported to reduce pulmonary vascular resistance and enable the right ventricle to better compensate for the physiologic changes of pregnancy. Inhaled NO, however, was less effective than other selective pulmonary vasodilators such as prostacycline in reducing pulmonary vascular resistance. Sildenafil, a type 5 phosphodiesterase inhibitor, can increase the levels of" cyclic guanosine monophosphate (cGMP) indirectly by decreasing its degradation. Previous studies have suggested that inhaled NO and sildenafil might have additive vasodilatory effects in the pulmonary circulation through actions on cGMP levels. Oral sildenafil at a dose of up to 50 mg four times per day has been shown to improve both hemodynamics and oxygenation in patients with pulmonary arterial hypertension. Oral sildenafil also has been shown to maintain ventilation-perfusion matching in patients with secondary pulmonary hypertension.
The present patient's chest radiograph (Fig 1) demonstrated a prominent pulmonary conus and engorged bilateral pulmonary arteries. The spiral CT scans of the chest (Fig 2) revealed discontinuity of the aortic arch just beyond the left subclavian artery (white arrows, Fig 2, top) and the existence of a patent ductus arteriosus (white arrowheads, Fig 2A). The absence of an interventricular septum indicated a large ventricular septal defect (black arrows, Fig 2, bottom), and the extremely engorged pulmonary arteries (black star mark, Fig 2, top) were compatible with pulmonary hypertension. The clinical symptoms, in conjunction with radiologic and echocardiographic findings, were diagnostic of Eisenmenger syndrome resulting from interrupted aortic arch, type A, with ventricular septal defect and patent ductus arteriosus.
The patient underwent a cesarean section on the fourth day of hospitalization. Time attempt at Swan-Ganz catheterization failed because of recurrent ventricular tachycardia with hypotension when the catheter was inserted into the right ventricle. Inhaled NO was administered to the patient at 20 ppm throughout the cesarean section, and she sustained the surgical procedure well. A live baby weighing 916 g was delivered, with Apgar scores of 7 and 9, respectively, at 1 and 5 rain. Unfortunately, the postpartum period was complicated by right ventricular overload and failure, resulting in a low cardiac output and hypotension (systolic BP, < 75 mm Hg) and oliguria (urine output, < 20 mL/h). She required therapy with high-dose inotropic agents (ie, dopamine and norepinephrine). The concentration of inhaled NO was increased to 40 ppm, and the patient's hemodynamics gradually stabilized. She was extubated 2 days after undergoing cesarean section, and the inhalation of NO was discontinued 18 h after extubation. Nevertheless, her respiratory distress persisted, and the pulse oximetry oxygen saturation of the fingers when breathing through a nonrebreathing mask was around 75 to 82%. Inhaled NO was administered again on the 11th day of hospitalization. However, increasing the inhaled NO to 60 ppm failed to improve her oxygenation and dyspnea. Because inhaled prostacycline and iloprost were not available for this patient, oral sildenafil was administered at an initial dose of 50 mg and was gradually increased to 100 mg twice per day. Figure 3 shows the time course of Pa[O.sub.2]/fraction of inspired oxygen throughout the course of hospitalization. Her oxygenation improved gradually, and respiratory distress also subsided. There were no significant side effects, and the systolic BP remained at > 90 mm Hg. She was successfully discharged from the ICU in stable condition on the 17th day of hospitalization. The patient rejected the suggestion of surgical intervention, opting to receive long-term oxygen therapy at home.
[FIGURE 3 OMITTED]
CLINICAL PEARLS
1. Interrupted aortic arch, a complex congenital heart disease, is rarely encountered in adults, and presentation ranges from asymptomatic to Eisenmenger syndrome with severe pulmonary hypertension.
2. The clinical course of a pregnancy complicated by Eisenmenger syndrome still carries substantial maternal mortality, and physiologic changes after delivery can precipitate the symptoms of pulmonary hypertension and right heart failure.
3. The maternal prognosis of pregnancy complicated by Eisenmenger syndrome depends on early diagnosis, early hospital admission, individually tailored treatment, and care focused on the postpartum period.
4. Inhaled NO can reduce pulmonary vascular resistance, and therefore can enable the right ventricle to better compensate for the physiologic changes of pregnancy and delivery in parturients with primary and secondary pulmonary hypertension.
5. Oral sildenafil, a type 5 phosphodiesterase inhibitor, can increase the levels of cGMP and may be an alternative to inhaled NO and other selective vasodilators in the management of pulmonary hypertension.
SELECTED READINGS
Bigatello LM, Hess D, Dennehy KC, et al. Sildenafil can increase the response to inhaled nitric oxide. Anesthesiology 2000; 92:1827-1829
Ghofrani HA, Schermuly RT, Rose F, et al. Sildenafil for long-term treatment of nonoperable chronic thromboembolic pulmonary hypertension. Am J Respir Crit Care Med 2003; 167:1139-1141
Ghofrani HA, Wiedemann R, Rose F, et al. sildenafil for treatment of lung fibrosis and pulmonary hypertension: a randomized controlled trial. Lancet 2902; 360:895-900
Messner G, Reul GJ, Flamm SD, et al. Interrupted aortic arch in an adult single-stage extra-anatomic repair. Tex Heart lnst J 2002; 29:118-121
Michelakis E, Tymchak W, Lien D, et al. Oral sildenafil is an effective and specific pulmonary vasodilator in patients with pulmonary arterial hypertension: comparison with inhaled nitric oxide. Circulation 2002; 105:2398-2403
Monnery L, Nanson J, Charlton G. Primary pulmonary hypertension in pregnancy: a role for novel vasodilators. Br J Anaesth 2001; 87:295 298
Stewart R, Tuazon D, Olson G. Pregnancy and primary pulmonary hypertension: successfull outcome with epoprostenol therapy. Chest 2001; 119:973-975
Robinson JN, Banerjee R, Landzberg MJ, et al. Inhaled nitric oxide therapy in pregnancy complicated by pulmonary hypertension. Am J Obstet Gynecol 1999; 180:1045-1046
Vongpatanasin W, Brickner ME, Hillis LD, et al. The Eisenmenger syndrome in adults. Ann Intern Med 1998; 128:745-755
Weiss BM, Zemp L, Seifert B, et al. Outcome of pulmonary vascular disease in pregnancy: a systematic overview from 1978 through 1996. J Am Coil Cardiol 1998; 31:1650-1657
* From the Departments of Internal Medicine (Drs. Chou, Kuo, and Yang) and Obstetrics (Dr. Shin), National Taiwan University Hospital, Taipei, Taiwan.
Manuscript received July 29, 2003; revision accepted October 3, 2003.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@ehestnet.org).
Correspondence to: Ping-Hung Kuo, MD, Department of the Internal Medicine, National Taiwan University Hospital, No. 7 Chung-Shan South Rd, Taipei, Taiwan, Republic of China; e-mail: kph@ntumc.org
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group