New data suggest that long-term management of stroke risk factors after a transient ischemic attack (TIA) generally is inadequate. (1) Part II of this two-part article reviews recent information on the management of the more important risk factors for stroke, the use of antiplatelet therapy, and special management issues in patients with TIAs.
Risk Factor Management
BLOOD PRESSURE
Elevated blood pressure (above 140/90 mm Hg) is the most important treatable risk factor for TIA and stroke. Antihypertensive drugs reduce the risk of strokes, regardless of whether patients have hypertension. (2) Currently, however, the American Heart Association (AHA) does not have any recommendations for antihypertensive drug therapy in "nonhypertensive" patients after a TIA or stroke. (3)
Hypertension occurs more frequently and more severely in blacks; therefore, this patient group merits special attention. Patients with diabetes mellitus or chronic renal disease also are at increased risk for hypertension and, thus, TIA or stroke. In patients with diabetes mellitus or chronic renal disease, the treatment goal is to keep blood pressure below 130/80 mm Hg.
Important new guidelines from the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) require lifestyle modifications (weight reduction, sodium restriction, regular aerobic activity, limited alcohol intake) to prevent cardiovascular disease in prehypertensive patients with a systolic blood pressure of 120 to 139 mm Hg or a diastolic blood pressure of 80 to 89 mm Hg. (4) [SOR C, consensus opinion]
Starting Antihypertensive Drug Therapy After a TIA or Stroke. Typically, blood pressure lowers without treatment in the first two weeks after a stroke. Therefore, it is rational to wait two weeks before continuing or beginning antihypertensive drug therapy.
In the patient found to have high blood pressure after a stroke or TIA, evidence of end-organ damage should be sought, because such damage suggests a chronic disorder rather than an acute condition. In some patients with chronically elevated blood pressure, the brain may depend on abnormally higher perfusion pressures because of derangement of the normal cerebral autoregulation of intracranial blood vessels. In this setting, abrupt lowering of blood pressure could promote cerebral ischemia or even extend an evolving infarction. Rarely, TIA is a manifestation of hemodynamically significant critical stenosis of an extracranial or intracranial vessel. In this condition, the brain requires increased cerebral perfusion pressure, and overtreatment of blood pressure may promote cerebral ischemia. The physician may note that TIAs occur when the patient's blood pressure drops or when the patient stands up or sits up.
In most patients, blood pressure should not be treated aggressively immediately (i.e., within the first 24 hours) after a stroke or TIA unless the systolic blood pressure is higher than 220 mm Hg or the diastolic blood pressure is above 120 mm Hg. (5) Important exceptions include patients with acute myocardial infarction (especially with left ventricular failure), hypertensive crisis or hypertensive encephalopathy, renal failure, aortic dissection, or retinal hemorrhages.
If, in the absence of the previously mentioned conditions, treatment is necessary, blood pressure should be reduced slowly over days to prevent worsening ischemia.
Angiotensin-Converting Enzyme (ACE) Inhibitors. Increased attention is being directed at ACE inhibitors because of the results of the recent Heart Outcomes Prevention Evaluation (HOPE) study. (6) In this large, randomized trial, inpatients considered to be at "high cardiovascular risk" were treated with ramipril or placebo. Over four years, the relative reduction in the risk of stroke was 32 percent (within a composite outcome) in the patients who received ramipril. Debate currently centers on whether the HOPE study findings were unique to ACE inhibitors as a class or occurred because of a more general blood pressure -lowering effect that also could be obtained with other antihypertensive drug classes.
In the Perindopril Protection Against Recurrent Stroke Study (PROGRESS), (7) patients with stroke or TIA within the previous five years were given placebo or combination therapy consisting of perindopril (an ACE inhibitor) and indapamide (a diuretic). In both hypertensive and "nonhypertensive" patients, the drug combination resulted in a 43 percent reduction in the relative risk of recurrent stroke (four-year follow-up). In PROGRESS, hypertension was defined as a systolic blood pressure of 160 mm Hg or higher or a diastolic blood pressure of 90 mm Hg or higher.
To date, however, no consensus statements indicate a preference for one antihypertensive drug or drug class over another for use in secondary (or primary) stroke prevention. (2,8,9) In particular, the use of ACE inhibitors after acute stroke remains controversial. (2) [Reference 2: SOR B, unknown effectiveness]
SMOKING
A meta-analysis (10) of 32 studies found that the risk of stroke in persons of either sex and all ages was 50 percent higher in smokers than in nonsmokers. Therefore, the family physician should make a vigorous attempt, at every clinic visit, to implement a smoking cessation plan, particularly in the patient who has had a TIA. Smoking cessation may be more likely to be successful if the physician encourages all family members to quit smoking simultaneously.
HEART DISEASE
Cardiac disease (i.e., rheumatic heart disease, mitral valve stenosis, atrial fibrillation with or without valvular disease) is a predisposing factor for TIA and stroke. In addition, the electrocardiographic finding of left ventricular hypertrophy resulting from prolonged hypertension is associated with a fourfold increased risk of stroke.
Patients with atrial fibrillation who also have other risk factors are at particularly high risk for TIA or stroke. These additional risk factors include a history of hypertension, poor left ventricular function, rheumatic mitral valve disease, prosthetic heart valves, previous stroke, systemic embolism, and age greater than 75 years. Patients with atrial fibrillation who have already had a TIA are considered to be at high risk for stroke. The results of one study (11) of patients with atrial fibrillation and TIA or minor stroke indicate that anticoagulant therapy is significantly more effective than aspirin in preventing recurrent stroke.
In addition, short-term cardiac morbidity is substantial after a TIA. One recent study (12) suggested that among patients who have a TIA, the 90-day risk for a cardiac event is higher in those who have any abnormal finding on an electrocardiogram (ECG). In this study, the ECG findings of left ventricular hypertrophy, atrial fibrillation, and atrioventricular conduction abnormalities in patients with TIA were independently associated with more than a doubling of the risk of a cardiac event.
BLOOD LIPID LEVELS
Convincing evidence from observational studies shows that elevated blood lipid levels are a risk factor for ischemic stroke. (13) High cholesterol levels are a risk factor for coronary heart disease (CHD) and, thus, a substantial secondary risk factor for stroke.
Recent data indicate that in patients with CHD, treatment with statins (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors) results in a 30 to 32 percent reduction of the stroke risk. (2,14,15) [Reference 2: SOR A, beneficial] Because statins have multiple vascular effects, as well as cholesterol-lowering properties, the exact mechanism of stroke prophylaxis is unknown.
Current guidelines (16,17) recommend consideration of statin therapy in patients with known CHD, many of whom could present with TIA or stroke. According to a recent Cochrane review, (18) it is not clear whether statin therapy is as effective in the prevention of recurrent stroke or TIA as it is in the primary prevention of stroke in patients with CHD.
DIABETES MELLITUS
Diabetes mellitus, independent of its association with hypertension, increases the overall risk of stroke by approximately 25 to 50 percent. (19) There is no conclusive evidence that "tight" glucose control results in a reduction of ischemic stroke or other macrovascular events. (20,21)
Recent data from the Microalbuminuria, Cardiovascular, and Renal Outcomes in HOPE (MICRO-HOPE) substudy (22,23) indicate that ramipril therapy reduces cardiovascular and cerebrovascular events in patients with diabetes mellitus and one cardiac risk factor. In MICRO-HOPE, stroke events were reduced by 33 percent, and stroke-related deaths were reduced by 37 percent.
Antiplatelet Therapy
Currently available antiplatelet agents for stroke prophylaxis include aspirin, clopidogrel (Plavix), ticlopidine (Ticlid), and aspirin-dipyridamole (Aggrenox). Except in patients with special conditions such as atrial fibrillation, anticoagulation has no advantages over antiplatelet therapy and is associated with an increased risk of bleeding. (2,24,25) [Reference 2: SOR A, likely to be harmful or ineffective]
ASPIRIN
Aspirin is the most widely used and most economical antiplatelet agent. Aspirin therapy after a stroke or TIA reduces the long-term relative risk of stroke and increases the chance of a full recovery. (26) The optimal aspirin dosage for use in the prevention of stroke or TIA remains controversial, but a range of 50 to 325 mg per day has been recommended. (3)
OTHER ANTIPLATELET AGENTS
Because of safety and tolerance issues associated with ticlopidine, clopidogrel is the more widely used second-line antiplatelet agent. Neutropenia, rash, diarrhea, and thrombotic thrombocytopenic purpura (TTP) occur less frequently with clopidogrel than with ticlopidine. The incidence of ticlopidine-related TTP is estimated to be one case per 1,600 to 5,000 patients treated. (3) Although clopidogrel and aspirin have similar safety profiles, there have been rare reports of clopidogrel-related TTP, with the majority of cases occurring within two weeks of initiation of the drug. (27)
One large, randomized, double-blind clinical trial (28) compared clopidogrel (75 mg per day) and aspirin (325 mg per day), with the composite outcome being the primary end points of stroke, myocardial infarction, and vascular death. There was a slight trend for clopidogrel to reduce annual outcome events compared with aspirin (5.3 percent versus 5.8 percent; P = .043). Based on this marginal difference and the fact that clopidogrel currently is more expensive than aspirin, many physicians favor the use of aspirin in a standard dosage (325 mg per day) for antiplatelet therapy but choose clopidogrel when patients cannot tolerate aspirin.
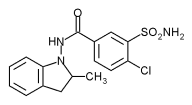
The U.S. Food and Drug Administration recently approved the use of combination aspirin-dipyridamole (Aggrenox) for stroke prevention. The combination drug contains 50 mg of aspirin (low dose) and 400 mg of extended-release dipyridamole. A single large, randomized study (29) found that this specific aspirin-dipyridamole combination reduced stroke by 22 percent compared with low-dose aspirin therapy alone. However, the expected similar benefits for reducing myocardial infarction and vascular death were not observed with aspirin, dipyridamole, or combination therapy.
Debate continues about the value of combination therapy and the interpretation of study data. Table 1 (3,27,29-31) summarizes key points about antiplatelet therapy in patients who have had a TIA.
Special Management Issues
TIA OR STROKE RECURRENCE DURING ANTIPLATELET THERAPY
Although well-established evidence supports the role of antiplatelet therapy in the prevention of recurrent stroke, fewer data are available to guide therapeutic decisions in patients who are receiving antiplatelet therapy but have another TIA or stroke. In patients who are taking an antiplatelet agent (most often, aspirin), the annual rate of recurrent stroke is estimated to be about 8 percent (range: 4 to 14 percent). (30,32)
Patient compliance with antiplatelet therapy should be determined. When possible, the cause of the TIA or sroke should be identified. If there is evidence of new-onset atrial fibrillation or a cardioembolic source, anticoagulation (rather than antiplatelet therapy) may be required, depending on the patient's age and other risk factors. All stroke risk factors should be immediately reevaluated and aggressively treated.
Many physicians question the therapeutic value of increasing the dosage of an antiplatelet agent, switching to a new agent, adding a second antiplatelet agent, or adding a low-dose anticoagulant drug. (3)
SYMPTOMATIC CAROTID DISEASE
Carotid Endarterectomy. There is little controversy surrounding the use of carotid endarterectomy for secondary prevention of stroke in patients with symptomatic severe carotid stenosis, defined as 70 to 99 percent vessel occlusion, based on the results of the North American Symptomatic Endarterectomy Trial (NASCET). (33) In the initial trial analysis (two-year follow-up), carotid endarterectomy reduced the relative risk of stroke by 65 percent compared with medical management.
The NASCET collaborators (34) recently reported that carotid endarterectomy may result in only a modest reduction of the stroke rate in patients with symptomatic moderate stenosis, defined as 50 to 69 percent vessel occlusion. The incidence of ipsilateral stroke was 16 percent in surgically treated patients and 22 percent in medically managed patients (P = .045). Based on their results, the authors recommended restraint rather than promotion of carotid endarterectomy.
A substudy analysis of patients from NASCET (35) who presented with bilateral carotid stenosis--one side that was symptomatic (noncardioembolic TIA or stroke) and the other side that was asymptomatic--revealed that the overall risk of stroke at five years was relatively low. Patients with 60 to 99 percent stenosis in the asymptomatic carotid artery had an overall 10 percent risk of a first stroke in the territory of the asymptomatic carotid, and a total 16 percent risk of stroke when lacunar and cardioembolic strokes were included (3.2 percent annual risk of stroke).High-risk patients included those with diabetes mellitus, silent brain infarction, or higher degree of stenosis. AHA guidelines for carotid endarterectomy recommend the use of aspirin (unless contraindicated) before surgery. (36)
Vascular Angioplasty and Stenting. The roles of vascular angioplasty and stenting procedures in stroke prevention remain controversial. The controversy has been fueled by the rapid development of new technologies and techniques, including distal cerebral protection devices. (37) It has been argued that patients with symptomatic high-grade carotid stenosis (70 percent vessel stenosis or higher) who are not candidates for routine carotid endarterectomy may represent a small subpopulation of patients who can benefit from extracranial carotid stenting or angioplasty; to date, however, this view has not been supported by published data from any large clinical trial.
ANTICOAGULATION
Unless contraindicated, anticoagulation therapy is appropriate in patients with high-risk cardioembolic conditions. 3 These conditions include atrial fibrillation, a known cardioembolic source (confirmed thrombus), or a suspected cardioembolic source (recent large myocardial infarction, mechanical valve, dilated cardiomyopathy, rheumatic mitral valve stenosis).
Anticoagulation has a well-established role in the primary prevention of stroke in patients with atrial fibrillation, especially high-risk patients with hypertension, poor left ventricular function, rheumatic mitral valve disease, prosthetic heart valves, a previous stroke, a TIA, systemic embolism, or age greater than 75 years. There is also evidence that warfarin (Coumadin) is useful for secondary prevention of stroke, as well as primary prevention. (38) It is unclear whether heparin should be started immediately after a TIA in patients with atrial fibrillation.
The rate of stroke recurrence after acute stroke in patients with atrial fibrillation currently is under debate. Reported recurrence rates for the initial weeks vary widely (2.5 to 20 percent). (39) The Cerebral Embolism Task Force (40) concluded that the risk of recurrent stroke was low during the first two weeks after a stroke in patients with nonvalvular atrial fibrillation. Whether the risk of recurrent TIA or the risk of stroke also is low in the patient with atrial fibrillation and TIA alone is unknown.
Patients who have atrial fibrillation also have noncardioembolic strokes. Therefore, even in the patient with atrial fibrillation, an evaluation for noncardiembolic risk factors should be performed. In the patient who previously has been diagnosed with TIA or stroke and is adequately anticoagulated, a second TIA or stroke could represent a noncardioembolic source. (41)
In patients with cardiogenic emboli, consensus is lacking on whether to start intravenous heparin therapy before chronic oral anticoagulation is initiated. (37,42,43)
HORMONE THERAPY IN WOMEN AFTER A TIA
The Women's Estrogen for Stroke Trial (44,45) was a randomized, blinded, placebo-controlled study that evaluated the effects of estrogen alone in a large cohort of postmenopausal women who had had a stroke or TIA. In this trial, estrogen therapy did not affect the incidence of nonfatal stroke during a mean follow-up period of 2.8 years.
New data indicate that certain menopausal hormone therapies increase the risk of CHD and ischemic stroke. (45,46) Therefore, the benefits and risks of hormone therapy should be weighed carefully in women who have had a TIA.
A recent meta-analysis (47) found an increased risk of stroke in women who use oral contraceptive pills (OCPs), including those who use low-dose OCPs. However, because of the low incidence of stroke in this young population, the overall benefit of OCPs may outweigh the risk. In women with previous stroke or TIA, it may be prudent to withhold OCPs or hormone therapy.
VERTEBROBASILAR ISCHEMIA
Anticoagulation commonly is used in patients who have had a vertebrobasilar stroke. However, a joint committee from the American Academy of Neurology and the American Stroke Association (48) found no clear evidence addressing this specific clinical situation and therefore provided no specific recommendations for the use of anticoagulation in these patients during acute cerebral ischemia. There is no mention of the use of anticoagulation in patients who have had a TIA, or of the use of surgical or endovascular treatments in patients with significant vertebrobasilar stenosis.
In patients with recurrent vertebrobasilar symptoms, interventions such as angioplasty, stenting, surgical reconstruction, and decompression have unproven efficacy. In an acute life-threatening situation such as midbasilar thrombotic occlusion (a condition associated with high morbidity and mortality rates), intra-arterial thrombolysis (if available) is an extreme option. Patients with refractory vertebrobasilar TIA should be evaluated by a neurologist before invasive procedures are performed, because these procedures can be associated with significant morbidity and mortality. (21,49)
Guidelines for the management of patients with TIAs are summarized in Tables 2 (4,16,17,21,50-53) and 3. (3,21,30,33,34,36,43,49,54-56)
The author indicates that she does not have any conflicts of interest. Sources of funding: none reported.
REFERENCES
(1.) Mouradian MS, Majumdar SR, Senthilselvan A, Khan K, Shuaib A. How well are hypertension, hyperlipidemia, diabetes, and smoking managed after a stroke or transient ischemic attack? Stroke 2002;33:1656-9.
(2.) Sudlow C, Gubitz G, Sandercock P, Lip G. Stroke prevention. Clin Evid 2003;(9):221-45.
(3.) Albers GW, Hart RG, Lutsep HL, Newell DW, Sacco RL. AHA scientific statement. Supplement to the guidelines for the management of transient ischemic attacks: a statement from the Ad Hoc Committee on Transient Ischemic Attacks, Stroke Council, American Heart Association. Stroke 1999;30:2502-11.
(4.) Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report [published correction appears in JAMA 2003;290:197]. JAMA 2003;289: 2560-72.
(5.) Semplicini A, Maresca A, Boscolo G, Sartori M, Rocchi R, Giantin V, et al. Hypertension in acute ischemic stroke: a compensatory mechanism or an additional damaging factor? Arch Intern Med 2003;163:211-6.
(6.) Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators [published correction appears in N Engl J Med 2000;342:1376]. N Engl J Med 2000;342: 145-53.
(7.) PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack [published corrections appear in Lancet 2001;358:1556 and Lancet 2002;359: 2120]. Lancet 2001;358:1033-41.
(8.) Hankey GJ. Angiotensin-converting enzyme inhibitors for stroke prevention: is there HOPE for PROGRESS after LIFE? Stroke 2003; 34:354-6.
(9.) Donnan GA, Davis SM, Thrift A. The role of blood pressure lowering before and after stroke. Current Opin Neurol 2003;16:81-6.
(10.) Shinton R, Beevers G. Meta-analysis of relation between cigarette smoking and stroke. BMJ 1999;298:789-94.
(11.) Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. EAFT (European Atrial Fibrillation Trial) Study Group. Lancet 1993;342:1255-62.
(12.) Elkins JS, Sidney S, Gress DR, Go AS, Bernstein AL, Johnston SC. Electrocardiographic findings predict short-term cardiac morbidity after transient ischemic attack. Arch Neurol 2002;59:1437-41.
(13.) Iso H, Jacobs DR Jr, Wentworth D, Neaton JD, Cohen JD. Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the Multiple Risk Factor Intervention Trial. N Engl J Med 1989;320:904-10.
(14.) Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994;344:1383-9.
(15.) Plehn JF, Davis BR, Sacks FM, Rouleau JL, Pfeffer MA, Bernstein V, et al. Reduction of stroke incidence after myocardial infarction with pravastatin: the Cholesterol and Recurrent Events (CARE) study. The CARE Investigators. Circulation 1999;99:216-23.
(16.) Goldstein LB, Adams R, Becker K, Furberg CD, Gorelick PB, Hademenos G, et al. Primary prevention of ischemic stroke: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Circulation 2001;103:163-82.
(17.) Pearson TA, Blair SN, Daniels SR, Eckel RH, Fair JM, Fortmann SP, et al. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation 2002;106:388-91.
(18.) Manktelow B, Gillies C, Potter JF. Interventions in the management of serum lipids for preventing stroke recurrence. Cochrane Database Syst Rev 2004;(1):CD002091.
(19.) Burchfiel CM, Curb JD, Rodriguez BL, Abbott RD, Chiu D, Yano K. Glucose intolerance and 22-year stroke incidence. The Honolulu Heart Program. Stroke 1994;25:951-7.
(20.) Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group [published correction appears in N Engl J Med 2000;342:1376]. N Engl J Med 2000;342:381-9.
(21.) Straus SE, Majumdar SR, McAlister FA. New evidence for stroke prevention: scientific review. JAMA 2002;288:1388-95.
(22.) Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Heart Outcomes Prevention Evaluation Study Investigators [published correction appears in Lancet 2000;356:860]. Lancet 2000;355:253-9.
(23.) Gerstein HC. Reduction of cardiovascular events and microvascular complications in diabetes with ACE inhibitor treatment: HOPE and MICRO-HOPE. Diabetes Metab Res Rev 2002;18(suppl 3): S82-5.
(24.) Sandercock P, Mielke O, Liu M, Counsell C. Anticoagulants for preventing recurrence following presumed non-cardioembolic ischaemic stroke or transient ischaemic attack. Cochrane Database Syst Rev 2004;(1):CD000248.
(25.) Berge E, Sandercock P. Anticoagulants versus antiplatelet agents for acute ischaemic stroke. Cochrane Database Syst Rev 2004; (1):CD003242.
(26.) Antithrombotic Trialists' Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients [published correction appears in BMJ 2002;324:141]. BMJ 2002; 324:71-86.
(27.) Bennett CL, Connors JM, Carwile JM, Moake JL, Bell WR, Tarantolo SR, et al. Thrombotic thrombocytopenic purpura associated with clopidogrel. N Engl J Med 2000;342:1773-7.
(28.) A randomised, blinded trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee. Lancet 1996,348:1329-39.
(29.) Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci 1996; 143:1-13.
(30.) Wolf PA, Clagett GP, Easton JD, Goldstein LB, Gorelick PB, Kelly-Hayes M, et al. Preventing ischemic stroke in patients with prior stroke and transient ischemic attack: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke 1999;30:1991-4.
(31.) Wilterdink JL, Easton D. Dipyridamole plus aspirin in cerebrovascular disease. Arch Neurol 1999;56:1087-92.
(32.) Hankey GJ, Warlow CP. Treatment and secondary prevention of stroke: evidence, costs, and effects on individuals and populations. Lancet 1999;354:1457-63.
(33.) Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 1991;325:445-53.
(34.) Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 1998;339:1415-25.
(35.) Inzitari D, Eliasziw M, Gates P, Sharpe BL, Chan RK, Meldrum HE, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 2000; 342:1693-700.
(36.) Biller J, Feinberg WM, Castaldo JE, Whittemore AD, Harbaugh RE, Dempsey RJ, et al. Guidelines for carotid endarterectomy: a statement for health care professionals from a Special Writing Group of the Stroke Council, American Heart Association. Circulation 1998; 97:501-9.
(37.) Bettmann MA, Katzen BT, Whisnant J, Brant-Zawadzki M, Broderick JP, Furlan AJ, et al. Carotid stenting and angioplasty: a statement for healthcare professionals from the Councils on Cardiovascular Radiology, Stroke, Cardio-Thoracic and Vascular Surgery, Epidemiology and Prevention, and Clinical Cardiology, American Heart Association. Stroke 1998;29:336-8.
(38.) Koudstaal PJ. Anticoagulants versus antiplatelet therapy for preventing stroke in patients with nonrheumatic atrial fibrillation and a history of stroke or transient ischemic attacks. Cochrane Database Syst Rev 2004;(1):CD000187.
(39.) Hart RG, Palacio S, Pearce LA. Atrial fibrillation, stroke, and acute antithrombotic therapy: analysis of randomized clinical trials. Stroke 2002;33:2722-7.
(40.) Cardiogenic brain embolism. The second report of the Cerebral Embolism Task Force [published correction appears in Arch Neurol 1989;46:1079]. Arch Neurol 1989;46:727-43.
(41.) Evans A, Perez I, Yu G, Kalra L. Secondary stroke prevention in atrial fibrillation: lessons from clinical practice. Stroke 2000;31:2106-11.
(42.) Fuster V, Ryden LE, Asinger RW, Cannom DS, Crijns HJ, Frye RL, et al. ACC/AHA/ESC guidelines for the management of patients with atrial fibrillation: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines and Policy Conferences (Committee to Develop Guidelines for the Management of Patients with Atrial Fibrillation in Collaboration with the North American Society of Pacing and Electrophysiology). Circulation 2001;104:2118-50.
(43.) Albers GW, Dalen JE, Laupacis A, Manning WJ, Petersen P, Singer DE. Antithrombotic therapy in atrial fibrillation. Chest 2001;119 (1 suppl 1):194S-206S.
(44.) Viscoli CM, Brass LM, Kernan WN, Sarrel PM, Suissa S, Horwitz RI. A clinical trial of estrogen-replacement therapy after ischemic stroke. N Engl J Med 2001;345:1243-9.
(45.) Manson JE, Hsia J, Johnson KC, Rossouw JE, Assaf AR, Lasser NL, et al.; Women's Health Initiative Investigators. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med 2003; 349:523-34.
(46.) Wassertheil-Smoller S, Hendrix SL, Limacher M, Heiss G, Kooperberg C, Baird A, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women's Health Initiative: a randomized trial. JAMA 2003;289:2673-84.
(47.) Gillum LA, Mamidipudi SK, Johnston SC. Ischemic stroke risk with oral contraceptives: a meta-analysis. JAMA 2000;284:72-8.
(48.) Coull BM, Williams LS, Goldstein LB, Meschia JF, Heitzman D, Chaturvedi S, et al. Anticoagulants and antiplatelet agents in acute ischemic stroke: report of the Joint Stroke Guideline Development Committee of the American Academy of Neurology and the American Stroke Association (a division of the American Heart Association). Stroke 2002;33:1934-42.
(49.) Hirsh J, Dalen J, Guyatt G; American College of Chest Physicians. The sixth (2000) ACCP guidelines for antithrombotic therapy for prevention and treatment of thrombosis. American College of Chest Physicians. Chest 2001;119(1 suppl):1S-307S.
(50.) Treating tobacco use and dependence. A clinical practice guide. Rockville, Md.: U.S. Dept. of Health and Human Services, Public Health Service, June 2000. Accessed January 15, 2004, at http:// www.surgeongeneral.gov/tobacco/treating_tobacco_use.pdf.
(51.) Woolf SH, Davidson MB, Greenfield S, Bell HS, Ganiats TG, Hagen MD, et al. Controlling blood glucose levels in patients with type 2 diabetes mellitus. An evidence-based policy statement by the American Academy of Family Physicians and American Diabetes Association. J Fam Pract 2000;49:453-60.
(52.) Fuster V, Ryden LE, Asinger RW, Cannm DS, Crijas HJ, Frye RL, et al. American Association of Clinical Endocrinologists. AACE medical guidelines for clinical practice for the diagnosis and treatment of dyslipidemia and prevention of atherogenesis. Endocr Pract 2000;6:162-213. Accessed January 15, 2004, at http://www.aace. com/clin/guidelines/lipids.pdf.
(53.) Gorelick PB, Sacco RL, Smith DB, Alberts M, Mustone-Alexander L, Rader D, et al. Prevention of first stroke: a review of guidelines and a multidisciplinary consensus statement from the National Stroke Association. JAMA 1999;281:1112-20.
(54.) Schunemann H, ed. Sixth ACCP Consensus Conference on Antithrombotic Therapy quick reference guide for clinicians. Accessed January 14, 2004, at http://www.chestnet.org/downloads/ guidelines/antithrombotic/qrg.pdf.
(55.) Hack W, Kaste M, Bogousslavsky J, Brainin M, Chamorro A, Lees K, et al; European Stroke Initiative Executive Committee and the EUSI Writing Committee. European Stroke Initiative recommendations for stroke management--update 2003. Cerebrovasc Dis 2003;16:311-37.
(56.) Sacco RL. Clinical practice. Extracranial carotid stenosis. N Engl J Med 2001;345:1113-8.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group