Received 6 February 2003; accepted 11 April 2003
ABSTRACT
UVB irradiation induces nuclear factor-[kappa]B (NF-[kappa]B) activation, tumor necrosis factor-[alpha] (TNF-[alpha]) expression and reactive oxygen intermediates (ROI) in keratinocytes. We investigated whether ROI play a role in UVB-induced TNF-[alpha] mRNA expression. The antioxidants N-acetyl cysteine, NAC, epigallocathin gallate, EGCG, butylated hydroxyanisole (BHA) and vitamin C could reduce UVB-induced TNF-[alpha] mRNA levels to various degrees; vitamin E ([alpha]-tocopherol) had no effect. BHA was the most potent inhibitor. The oxidant tertiary butylated hydroperoxide could effectively induce TNF-[alpha] mRNA expression. Nordihydroguaiaretic acid (NDGA) and MK-886, inhibitors of lipoxygenase (LOX), and indometacin and quinacrine, inhibitors of cyclooxygenase (COX) and phospholipase A^sub 2^, respectively, could also reduce UVB-induced TNF-[alpha] mRNA expression. Inhibition by NDGA was in concordance with the results for BHA. NDGA, indometacin, quinacrine and BHA could also effectively inhibit the inhibitor of NF-[kappa]B degradation, thereby maintaining NF-[kappa]B inactivity. In conclusion, we show that ROI are implicated in the induction of TNF-[alpha] mRNA by UVB and that not all antioxidants are equally effective inhibitors. COX products and more importantly LOX products, which themselves are products of an oxidative metabolism, are the main ROI implicated in this induction of TNF-[alpha] expression by UVB probably via activation of NF-[kappa]B.
Abbreviations: BHA, butylated hydroxyanisole; COX, cyclooxygenase; EGCG, epigallocatechin gallate; FLAP, 5-lipoxygenase-activating protein; I[kappa]B[alpha] inhibitor of NF-[kappa]B; LOX, lipoxygenase; NAC, N-acetylcysteine; NDGA, nordihydroguaiaretic acid; NF-[kappa]B, nuclear factor-[kappa]B; NHK, normal human keratinocytes; PLA^sub 2^, phospholipase A^sub 2^; ROI, reactive oxygen intermediates; tBHP, tertiary butylated hydroperoxide; TNF-[alpha], tumor necrosis factor-[alpha].
INTRODUCTION
Keratinocytes are the major target for UVB effects on skin. UVB absorption by keratinocytes results in direct DNA damage (1) as well as in the production of reactive oxygen intermediates (ROI) such as superoxide anion, hydroxyl radical, lipid peroxyl radical and hydrogen peroxide (2). UVB can also induce cytokine induction in keratinocytes including interleukin 1 (IL-1), IL-6, IL-8, IL-10, granulocyte-macrophage colony-stimulating factor (GM-CSF) and tumor necrosis factor-[alpha] (TNF-[alpha]) (3). TNF-[alpha] has a wide range of proinflammatory and cytotoxic effects (4). TNF-[alpha] production by UVB irradiated keratinocytes has not only been implicated in the local inflammatory reactions but TNF-[alpha] may also enter the circulation and cause systemic effects (5,6). It has also been demonstrated that TNF-[alpha] is involved in sunburn cell formation (apoptotic keratinocytes) after UVB irradiation (7).
The promoter site of TNF-[alpha] contains a consensus binding site for nuclear factor-[kappa]B (NF-[kappa]B). UVB also induces NF-[kappa]B activity (8). NF-[kappa]B or (p50-Rel), is the best-known member of the NF-[kappa]B-Rel family. NF-[kappa]B is retained in the cytoplasm by an inhibitor of NF-[kappa]B [alpha] (I[kappa]B[alpha]) protein (9). An appropriate signal can trigger the phosphorylation, ubiquitination and degradation of this inhibitory protein after which the NF-[kappa]B translocates to the nucleus and binds to its responsive elements present in a variety of genes, including cytokines like TNF-[alpha].
In a previous study, we have shown that UVB induces TNF-[alpha] mRNA expression and secretion (10). Much is known about the signaling pathway triggered by TNF-[alpha] (leading to inflammation and apoptosis) and the effect of UVB on this pathway, but not many reports investigate the mechanisms of TNF-[alpha] induction by UVB irradiation in keratinocytes. Previous studies point toward a possible role of reactive oxygen intermediates (ROI) (11-13) as well as direct DNA damage (14-17) in the induction mechanisms of TNF-[alpha] expression.
Phospholipase A2 (PLA^sub 2^) is an enzyme that mainly cleaves arachidonic acid from the sn-2 position of phospholipids in the membrane. The liberated arachidonic acid can then be converted to eicosanoids through the action of cyclooxygenase (COX)-1 and COX-2, with the formation of different prostaglandins, or by 5-lipoxygenase (LOX), 12-LOX and 15-LOX, with the formation of different hydroperoxyeicostetraenoic acid (HPETE), hydroxyeicosatetraenoic acid (HETE) and subsequently leukotrienes (18). In keratinocytes it has been shown that UVB can induce PLA^sub 2^ as well as COX through the action of ROI (19,20). Whether or not LOX is induced by UVB remains an open question but it is known that the enzyme needs a minimum peroxide tone for its function and that it generates hydroperoxides and superoxide anion radicals (21,22).
UVB is an effective inducer of oxidative stress with the primary production of superoxide anion. Exposure of human keratinocytes to UVB results in lipid peroxidation whereby antioxidant enzymes are destroyed and COX and LOX products are produced (23). Exogenous antioxidants can strengthen the enzymatic line of defense against oxidative molecules. Epigallocatechin gallate (EGCG) is a flavonoid antioxidant, which is an ideal scavenger of peroxyl radicals and is thus, in principle, an effective inhibitor of lipid peroxidation (24). N-acetylcysteine (NAC) is a precursor for reduced glutathione, which constitutes the glutathione redox cycle, an inherent antioxidant defense system of the cell. A component of this redox cycle is the glutathione peroxidase that can neutralize lipid peroxides. [alpha]-Tocopherol is the isoform of vitamin E, which is absorbed and maintained in the human body. It is incorporated into the cellular membranes and can effectively inhibit lipid peroxidation by scavenging the chain-propagating peroxyl radical. The free-radical form of vitamin E must in its turn be reduced by other antioxidants such as the cytoplasmic vitamin C (ascorbic acid), otherwise further propagation of the free radical chain between lipids can occur (25). Besides its antioxidative properties, [alpha]-tocopherol also has nonoxidative properties, such as inhibition of protein kinase C and gene regulation (26). Butylated hydroxyanisole (BHA) is a synthetic, lipid-soluble antioxidant with free radical scavenging properties. Nordihydroguaiaretec acid (NDGA) is a lipid-soluble, selective LOX inhibitor (IC^sub 50^ 200 nM for 5-LOX and 30 [mu]M for 12- and 15-LOX) with powerful hydroxyl radical quenching properties. MK-886 is a selective 5-LOX inhibitor. It inhibits 5-lipoxygenase-activating protein (FLAP) that is necessary for the activation of 5-LOX (27).
The objective of this study was to investigate whether ROI and COX and LOX products play a role in the induction of TNF-[alpha] by UVB irradiation in normal human keratinocytes (NHK). Various antioxidants, as well as a PLA^sub 2^, COX and LOX inhibitors were tested for their capacity to inhibit TNF-[alpha] expression in UVB-irradiated keratinocytes. Our results indicate that ROI are implicated in UVB-induced expression of TNF-[alpha] in keratinocytes and that COX products and more importantly LOX products, also known as eicosanoids and which are themselves products of an oxidative metabolism, are the main ROI implicated in this induction. These eicosanoids likely exert their function through activation of NF-[kappa]B.
MATERIALS AND METHODS
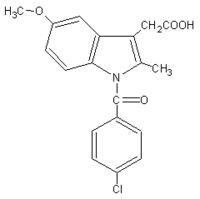
Materials. All chemicals used were purchased from Sigma-Aldrich (Bornem, Belgium) except for MK-886, which was purchased from Biomol-Sanvertech (Boechout, Belgium). EGCG, [alpha]-tocopherol, BHA, NDGA and MK-886 were dissolved in EtOH. Vitamin C, NAC and indometacin were dissolved in phosphate-buffered saline (PBS). Quinacrine was dissolved in sterile Baxter water, and FeCl^sub 2^ solutions were made fresh, also in sterile Baxter water. The following concentrations were used: NAC (3 mM), EGCG (50 [mu]M), vitamin C (1 mM), vitamin E (50 [mu]M), tertiary butylated hydroperoxide (tBHP) (200 [mu]M), FeCl^sub 2^ (4 [mu]g/ml), NDGA (10 [mu]M), indometacin (10 [mu]M) and quinacrine (10 [mu]M).
Cell culture. NHK were grown as described previously (10). For experiments, NHK (passage 4) were seeded at a density of 1.10^sup 6^ cells in 100 mm petridishes. The next day, various antioxidants were added to the cells for 24 h before irradiation. The inhibitors NDGA, indometacin, quinacrine and MK-886 were added 12 h before irradiation, and the oxidants tBHP and FeCl^sub 2^ were added 1 h before irradiation.
Irradiation procedure. Three Philips TL20W 12 tubes with a peak output around 310 nm were used as a UVB source. Before irradiation, cells were washed with PBS and then irradiated through a thin film of PBS. Cells were then reefed with their own medium immediately after irradiation. Cells were irradiated with a single sublethal UVB dose (32 mJ/cm^sup 2^), as measured with an IL 700 A Research Radiometer (International Light, Newburyport, MA). Cells were collected for RNA of protein isolation at 5 h after irradiation unless otherwise specified.
Northern blot analysis. Cells were collected 5 h after irradiation for RNA isolation and Northern blot analysis with TNF-[alpha] and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) probes as previously described (10).
Western blot analysis. Protein isolation and immunoblot analysis were performed as previously described (28). A polyclonal rabbit anti-mouse I[kappa]B[alpha] antibody (BD Biosciences-Life Science, Erembodegem, Belgium) was used. Equal loading of proteins was verified with a monoclonal antiactin antibody (Clone AC-15, Sigma-Aldrich).
RESULTS
UVB-induced TNF-[alpha] mRNA expression is inhibited to varying degrees by different antioxidants
As shown in previous studies, TNF-[alpha] mRNA and protein expression is almost undetectable in untreated NHK. At 5 h postirradiation, levels of TNF-[alpha] mRNA and excreted protein are easily detected (10). To investigate whether ROI were involved in the TNF-[alpha] mRNA induction, various antioxidants were added to the NHK 24 h before UVB irradiation. At 5 h postirradiation, we see a clear expression level of TNF-[alpha] mRNA. BHA (200 [mu]M) almost completely suppresses UVB-induced TNF-[alpha] mRNA. Addition of NAC (3 mM) resulted in a + or - 2.5-fold inhibition, EGCG (50 [mu]M) and vitamin C (1 mM) were less effective inhibitors, and vitamin E (50 [mu]M) and more importantly the combination of vitamin E and vitamin C had no effect (Fig. 1). Figure 1 represents data of at least three independent experiments, and nearly identical findings were obtained in all experiments. The concentrations of the antioxidants used in this study were on the basis of earlier reports (29-36).
TNF-[alpha] mRNA expression is induced by the free radical producer tBHP but not by FeCl^sub 2^
tBHP is a hydroperoxide. Hydroperoxide breakdown results in the formation of hydroxyl radical and alkoxyl radical. The hydroxyl radical is the primary inducer of lipid peroxidation. FeCl^sub 2^ can activate lipid peroxidation because the FeII atom is implicated in the Fenton reaction, the catalyzed formation of hydroxyl radicals from hydroperoxide (37). In this scenario, the hydroperoxide molecule already has to be present in sufficient amounts, which is not the case in unstressed, unirradiated cells.
We could observe an induction of TNF-[alpha] mRNA by the addition of tBHP (200 [mu]M) but not by FeCl^sub 2^ (4 [mu]g/ml) in unirradiated keratinocytes. However, the addition of tBHP or FeCl^sub 2^ before UVB irradiation did not result in a synergistic effect. Instead we could see a reduction of UVB-induced TNF-[alpha] mRNA (Fig. 2).
Products of the COX and LOX pathway are involved in the induction of TNF-[alpha] mRNA expression by UVB irradiation
NDGA (10 [mu]M) is a selective LOX inhibitor and an effective scavenger of radicals. NDGA could almost completely inhibit UVB-induced TNF-[alpha] mRNA expression (Fig. 3). Considering the low concentration of NDGA we can presume that LOX products are important mediators of TNF-[alpha] expression after UVB irradiation. Inhibitor of COX, indometacin (10 [mu]M) (38), and inhibitor of PLA^sub 2^, quinacrine (10 [mu]M) (39), could also reduce TNF-[alpha] mRNA, which indicates that in general the eicosanoids play an important role in the induction of TNF-[alpha] expression by UVB (Fig. 3). To further confirm the involvement of products of the LOX pathway, we performed a dose-response experiment with NDGA. Figure 4 demonstrates a dose-dependent inhibition of UVB-induced TNF-[alpha] mRNA expression, starting at a very low dose, 1 [mu]M and total inhibition at 5 and 10 [mu]M. Also the addition of a specific 5-LOX inhibitor MK-886 (1 [mu]M; inhibitor of FLAP) could reduce UVB-induced TNF-[alpha] mRNA levels (Fig. 4).
UVB induces I[kappa]B[alpha] degradation in NHK
UVB is known to activate NF-[kappa]B (8). To assess the kinetics of NF-[kappa]B activation by UVB in our experimental conditions, we studied the expression levels of the protein I[kappa]B[alpha]. Degradation of this protein reflects indirectly activation of NF-[kappa]B. UVB induces a decrease in the protein levels of I[kappa]B[alpha], with a maximal effect within 5 h after irradiation, indicative of maximal NF-[kappa]B activation within 5 h after irradiation (Fig. 5).
Products of the COX and LOX pathway are involved in NF-[kappa]B activation by UVB irradiation
The promoter site of TNF-[alpha] contains a consensus binding site for NF-[kappa]B. Therefore we explored the possibility of whether the inhibitors studied could also reduce UVB-induced NF-[kappa]B activation which could then be responsible for the reduced TNF-[alpha] levels. Activation status of NF-[kappa]B was studied via investigation of the expression levels of the protein I[kappa]B[alpha]. As shown in Fig. 6, NDGA (10 [mu]M) completely inhibited UVB-induced I[kappa]B[alpha] degradation at 5 h after irradiation. Indometacin (10 [mu]M) and quinacrine (10 [mu]M) could also reduce UVB-induced I[kappa]B[alpha] degradation. This indeed indicates that products of LOX and COX activity are important in the activation of NF-[kappa]B by UVB.
We also tested whether BHA, which was very effective in reducing UVB-induced TNF-[alpha] levels, could also inhibit UVB-induced NF-[kappa]B activation. As is shown in the left side of Fig. 6, BHA treatment (200 [mu]M) resulted in increased I[kappa]B[alpha] levels after UVB irradiation, indicative of a lower NF-[kappa]B activity.
DISCUSSION
Addition of different antioxidants could inhibit UVB-induced TNF-[alpha] mRNA expression to various degrees. BHA was the most potent inhibitor and could almost completely suppress UVB-induced TNF-[alpha] expression. NAC was also an efficient inhibitor. NAC has already been implicated in the inhibition of lipopolysaccharide (LPS)-induced TNF-[alpha] levels (40).
Vitamin E, the well-known lipophilic antioxidant was ineffective as inhibitor of TNF-[alpha] expression. We performed a dose-response for vitamin E: 1, 10, 50 and 100 [mu]M (results not shown). Concentrations of up to 100 [mu]M vitamin E could not affect TNF-[alpha] expression levels in UVB-irradiated keratinocytes. However, in this study 50 [mu]M of vitamin E, the concentration most often used in the literature, could effectively inhibit lipid peroxidation in UVB-irradiated keratinocytes, pretreated with EPA, indicating that vitamin E is taken up by the cell and is active in these concentrations. Our results with vitamin E correspond with the results of Eugui et al. (12), who could not inhibit LPS-induced cytokine levels by using vitamin E. The reason for this remains obscure. Maybe vitamin E can influence TNF-[alpha] expression via other cellular pathways by its nonantioxidative properties or maybe vitamin E is not in the right cellular compartment for efficient scavenging of the ROI responsible for cytokine induction. A third reason can be that the unstable vitamin E radical, which can propagate the radical chain reaction, is not efficiently neutralized by other antioxidants like vitamin C. In our model, however, the combined addition of vitamin E and vitamin C did not result in the inhibition of TNF-[alpha] mRNA.
Vitamin C alone could reduce UVB-induced TNF-[alpha] mRNA levels and finally EGCG also had, although in a less effective way, inhibitory properties.
O'Connor et al. (14) have shown that breaks in DNA double strand can induce TNF-[alpha] in a murine keratinocyte cell line and in the epidermis of mice. Cruz et al. (16) found that thymidine dinucleotides which arise from DNA damage induced by UVB can activate the TNF-[alpha] gene in a human squamous cell carcinoma line. Finally, Kibitel et al. (17) demonstrated decreased TNF-[alpha] expression when the level of DNA repair is increased by adding the DNA repair enzyme T4 endonuclease. These studies suggest that direct DNA damage plays a role, however not necessarily an exclusive role, in the induction mechanisms of TNF-[alpha] by UVB. On the other hand, TNF-[alpha] expression on stimulation like LPS has been shown to involve ROI (12), and a more recent study by Dy et al. (13) also points to a possible role of ROI in the induction of TNF-[alpha] in keratinocytes on UVB irradiation. They found that the platelet-activating factor receptor (PAF-R) was necessary for the induction of TNF-[alpha] after UVB irradiation. Instead of PAF itself, PAF-like agonists, probably phospholipids oxidized by the pro-oxidative stressor UVB, were responsible for activation of this receptor. Finally, the study by Corsini et al. (11) reported that IL-1[alpha] has an autocrine effect in inducing TNF-[alpha] and that the addition of antioxidants could inhibit TNF-[alpha] release in the human keratinocyte cell line NCTC 2544. Also our data argue for a role for ROI in the induction of TNF-[alpha] by UVB in keratinocytes because four well-known anti-oxidants, BHA, NAC, EGCG and Vitamin C, could reduce TNF-[alpha] expression in UVB-irradiated keratinocytes. The effect of these antioxidants cannot be attributed to their effect on induction of direct DNA damage because the induction of this damage is oxygen independent.
In addition to antioxidants, inhibitors of the eicosanoid pathway could also inhibit UVB-induced TNF-[alpha] expression. NDGA, a LOX inhibitor could dose dependency suppress TNF-[alpha] expression, until complete suppression. Because we already observed an effect with low concentration of NDGA, we can presume that these LOX products are important mediators of TNF-[alpha] expression after UVB irradiation. In addition we could show that a low dose of another potent and selective inhibitor of 5-LOX, MK-886, could suppress TNF-[alpha] expression in UVB-irradiated keratinocytes. This is another argument in favor of a role for LOX products as mediators of TNF-[alpha] expression in UVB-irradiated keratinocytes.
Indometacin, a nonsteroidal anti-inflammatory drug (NSAID), which inhibits COX and quinacrine, an inhibitor of PLA^sub 2^, also inhibits TNF-[alpha] expression in UVB-irradiated keratinocytes. In keratinocytes it has been shown that UVB can induce PLA^sub 2^ as well as COX (10,18,19), and this may explain the inhibitory effects of indometacin and quinacrine on TNF-[alpha] mRNA expression in UVB-irradiated keratinocytes.
The LOX pathway generates hydroperoxides (21,22); therefore, we investigated the effect of tBHP and FeCl^sub 2^ on TNF-[alpha] mRNA expression. The hydroperoxide tBHP but not FeCl^sub 2^ was able to induce TNF-[alpha] mRNA expression. However, tBHP or FeCl^sub 2^ in combination with UVB irradiation did not result in a synergistic effect on TNF-[alpha] expression. Instead, and much to our surprise, a reduction could be observed. The reason for this remains obscure. We hypothesize that the UVB-induced oxidative stress together with the presence of oxidants results in destruction and further oxidative breakdown of the functional ROI. Or maybe, the addition of oxidants before irradiation results in an upregulation of endogenous antioxidative enzymes and a more efficient scavenging of UVB-induced oxidative molecules.
UVB can induce NF-[kappa]B activity and cytokine expression. NF-[kappa]B (p50-Rel) is a ubiquitous transcription factor and the best-known member of the NF-[kappa]B-Rel family. NF-[kappa]B is retained in the cytoplasm by an I[kappa]B[alpha] protein. An appropriate signal can trigger the phosphorylation, ubiquitination and degradation of this inhibitory protein after which the NF-[kappa]B translocates to the nucleus and binds to its responsive elements present in a variety of genes, like cytokines (TNF-[alpha] and [beta], IL-2, IL-6, IL-8 and IFN-[beta]). NF-[kappa]B is redox sensitive and can be activated by H^sub 2^O^sub 2^ (41). Flohe et al. (42) already hypothesized that the activation of NF-[kappa]B by H^sub 2^O^sub 2^ could be extended to a large variety of hydroperoxides. Therefore, we investigated the effect of the eicosanoid inhibitors on I[kappa]B[alpha] degradation, indicative of NF-[kappa]B activation. Pretreatment with the LOX inhibitor NDGA completely prevented I[kappa]B[alpha] degradation by UVB. Indometacin, an NSAID that inhibits COX and quinacrine, an inhibitor of PLA^sub 2^, had also inhibitory properties. This was in concordance with the results from van Puijenbroek et al. (43), which show that NDGA and 4-bromophenacyl bromide, an inhibitor of PLA^sub 2^, could inhibit TNF-[alpha]-induced NF-[kappa]B activity.
These data indicate that the main ROI which induce TNF-[alpha], probably via an NF-[kappa]B-dependent pathway, in UVB-irradiated keratinocytes are products of LOX and COX activity. This may also explain why BHA was very effective in the inhibition of UVB-induced NF-[kappa]B activation and TNF-[alpha] mRNA expression. BHA is, like NDGA, a lipid-soluble antioxidant with free radical scavenging properties but has also inhibitory activity on LOX (44).
Our findings may have clinical implications. TNF-[alpha] is a multifunctional cytokine, which plays an important role in UV-induced inflammatory effects, both locally on the skin and systemically (6). TNF-[alpha] is also involved in sunburn cell formation (apoptotic keratinocytes) in the epidermis after UVB irradiation (7). A better understanding of the induction mechanisms of TNF-[alpha] upon UVB in keratinocytes may open new possibilities for therapeutic intervention of the above-mentioned UV effects mediated by this cytokine.
In conclusion, our data demonstrate that ROI are implicated in the induction of TNF-[alpha] mRNA by UVB and that not all antioxidants are equally effective inhibitors. COX products and more importantly LOX products, which themselves are products of a certain oxidative metabolism, are the main ROI implicated in this induction of TNF-[alpha] expression by UVB, probably via their activation of NF-[kappa]B. Hence, this study is, to our knowledge, the first to show a major involvement of the eicosanoid pathway in the induction of NF-[kappa]B and TNF-[alpha] in UVB-irradiated keratinocytes.
Acknowledgements-This work was supported, in part, by grant OT/96/27 from the university of Leuven and the European Commission (EN54-CT97-0537). M.G. is clinical research associate (FWO).
[para]Posted on the website on 28 April 2003.
REFERENCES
1. Vink, A. A. and L. Roza (2001) Biological consequences of cyclobutane pyrimidine dimers. J. Photochem. Photobiol. B: Biol. 65, 101-104.
2. Tyrrell, R. M. (1995) Ultraviolet radiation and free radical damage to skin. Biochem. Soc. Symp. 61, 47-53.
3. Takashima, A. and P. R. Bergstresser (1996) Impact of UVB radiation on the epidermal cytokine network. Photochem. Photobiol. 63, 397-400.
4. Bazzoni, F. and B. Beutler (1996) The tumor necrosis factor ligand and receptor families. N. Engl. J. Med. 334, 1717-1725.
5. Kondo, S. and D. N. Sauder (1995) Keratinocyte-derived cytokines and UVB-induced immunosuppression. J. Dermatol. 22, 888-893.
6. Kock, A., T. Schwarz, R. Kirnbauer, A. Urbanski, P. Perry, J. C. Ansel and T. A. Luger (1990) Human keratinocytes are a source for tumor necrosis factor alpha: evidence for synthesis and release upon stimulation with endotoxin or ultraviolet light. J. Exp. Med. 172, 1609-1614.
7. Schwarz, A., R. Bhardwaj, Y. Aragane, K. Mahnke, H. Riemann, D. Metze, T. A. Luger and T. Schwarz (1995) Ultraviolet-B-induced apoptosis of keratinocytes: evidence for partial involvement of tumor necrosis factor-alpha in the formation of sunburn cells. J. Investig. Dermatol. 104, 922-927.
8. Simon, M. M., Y. Aragane, A. Schwarz, T. A. Luger and T. Schwarz (1994) UVB light induces nuclear factor kappa B (NF kappa B) activity independently from chromosomal DNA damage in cell-free cytosolic extracts. J. Investig. Dermatol. 102, 422-427.
9. Baeuerle, P. A. and D. Baltimore (1996) NF-kappa B: ten years after. Cell 87, 13-20.
10. Pupe, A., R. Moison, P. De Haes, V. H. Beijersbergen, L. Rhodes, H. Degreef and M. Garmyn (2002) Eicosapentaenoic acid, a n-3 polyunsaturated fatty acid differentially modulates TNF-alpha, IL-1alpha, IL-6 and PGE2 expression in UVB-irradiated human keratinocytes. J. Investig. Dermatol. 118, 692-698.
11. Corsini, E., A. Bruccoleri, M. Marinovich and C. L. Galli (1995) In vitro mechanism(s) of ultraviolet-induced tumor necrosis factor-alpha release in a human keratinocyte cell line. Photodermatol. Photoimmunol. Photomed. 11, 112-118.
12. Eugui, E. M., B. DeLustro, S. Rouhafza, M. Ilnicka, S. W. Lee, R. Wilhelm and A. C. Allison (1994) Some antioxidants inhibit, in a co-ordinate fashion, the production of tumor necrosis factor-alpha, IL-beta, and IL-6 by human peripheral blood mononuclear cells. Int. Immunol. 6, 409-422.
13. Dy, L. C., Y. Pei and J. B. Travers (1999) Augmentation of ultraviolet B radiation-induced tumor necrosis factor production by the epidermal platelet-activating factor receptor. J. Biol. Chem. 274, 26917-26921.
14. O'Connor, A., C. Nishigori, D. Yarosh, L. Alas, J. Kibitel, L. Burley, P. Cox, C. Bucana, S. Ullrich and M. Kripke (1996) DNA double strand breaks in epidermal cells cause immune suppression in vivo and cytokine production in vitro. J. Immunol. 157, 271-278.
15. Yarosh, D., D. Both, J. Kibitel, C. Anderson, C. Elmets, D. Brash and D. Brown (2000) Regulation of TNFalpha production and release in human and mouse keratinocytes and mouse skin after UV-B irradiation. Photodermatol. Photoimmunol. Photomed. 16, 263-270.
16. Cruz Jr., P. D., M. Leverkus, I. Dougherty, M. J. Gleason, M. Eller, M. Yaar and B. A. Gilchrest (2000) Thymidine dinucleotides inhibit contact hypersensitivity and activate the gene for tumor necrosis factor alpha1. J. Investig. Dermatol. 114, 253-258.
17. Kibitel, J., V. Hejmadi, L. Alas, A. O'Connor, B. M. Sutherland and D. Yarosh (1998) UV-DNA damage in mouse and human cells induces the expression of tumor necrosis factor alpha. Photochem. Photobiol. 67, 541-546.
18. Heller, A., T. Koch, J. Schmeck and K. van Ackern (1998) Lipid mediators in inflammatory disorders. Drugs 55, 487-496.
19. Chen, X., A. Gresham, A. Morrison and A. P. Pentland (1996) Oxidative stress mediates synthesis of cytosolic phospholipase A2 after UVB injury. Biochim. Biophys. Acta 1299, 23-33.
20. Isoherranen, K., K. Punnonen, C. Jansen and P. Uotila (1999) Ultraviolet irradiation induces cyclooxygenase-2 expression in keratinocytes. Br. J. Dermatol. 140, 1017-1022.
21. Roy, P., M. P. Sajan and A. P. Kulkarni (1995) Lipoxygenase-mediated glutathione oxidation and superoxide generation. J. Biochem. Toxicol. 10, 111-120.
22. Roy, P., S. K. Roy, A. Mitra and A. P. Kulkarni (1994) Superoxide generation by lipoxygenase in the presence of NADH and NADPH. Biochim. Biophys. Acta 1214, 171-179.
23. Punnonen, K., A. Puntala, C. T. Jansen and M. Ahotupa (1991) UVB irradiation induces lipid peroxidation and reduces antioxidant enzyme activities in human keratinocytes in vitro. Acta Dermato-Venereol. 71, 239-242.
24. Rice-Evans, C. (2001) Flavonoid antioxidants. Curr. Med. Chem. 8, 797-807.
25. Packer, L., S. U. Weber and G. Rimbach (2001) Molecular aspects of alpha-tocotrienol antioxidant action and cell signalling. J. Nutr. 131, 369S-373S.
26. Ricciarelli, R., J. M. Zingg and A. Azzi (2001) Vitamin E: protective role of a Janus molecule. FASEB J. 15, 2314-2325.
27. Dixon, R. A., R. E. Diehl, E. Opas, E. Rands, P. J. Vickers, J. F. Evans, J. W. Gillard and D. K. Miller (1990) Requirement of a 5-lipoxygenase-activating protein for leukotriene synthesis. Nature 343, 282-284.
28. Courtois, S. J., S. Segaert, H. Degreef, R. Bouillon and M. Garmyn (1998) Ultraviolet B suppresses vitamin D receptor gene expression in keratinocytes. Biochem. Biophys. Res. Commun. 246, 64-69.
29. Garmyn, M. and H. Degreef (1997) Suppression of UVB-induced c-fos and c-jun expression in human keratinocytes by N-acetylcysteine. J. Photochem. Photobiol. B: Biol. 37, 125-130.
30. Ahmad, N., S. Gupta and H. Mukhtar (2000) Green tea polyphenol epigallocatechin-3-gallate differentially modulates nuclear factor kappa B in cancer cells versus normal cells. Arch. Biochem. Biophys. 376, 338-346.
31. Verhaegen, S., A. J. McGowan, A. R. Brophy, R. S. Fernandes and T. G. Cotter (1995) Inhibition of apoptosis by antioxidants in the human HL-60 leukemia cell line. Biochem. Pharmacol. 50, 1021-1029.
32. Timmins, G. S. and M. J. Davies (1993) Free radical formation in isolated murine keratinocytes treated with organic peroxides and its modulation by antioxidants. Carcinogenesis 14, 1615-1620.
33. Finstad, H. S., M. C. Wik Myhrstad, H. Heimli, J. Lomo, H. Kiil Blomhoff, S. O. Kolset and C. A. Drevon (1998) Multiplication and death-type of leukemia cell lines exposed to very long-chain polyunsaturated fatty acids. Leukemia 12, 921-929.
34. Straface, E., M. T. Santini, G. Donelli, P. U. Giacomoni and W. Malorni (1995) Vitamin E prevents UVB-induced cell blebbing and cell death in A431 epidermoid cells. Int. J. Radiat. Biol. 68, 579-587.
35. Shang, J., C. Schwarz, R. H. Sanchez, T. Hertting, C. E. Orfanos and B. Tebbe (2002) Effects of UVA and L-ascorbic acid on nuclear factor-kappa B in melanocytes and in HaCaT keratinocytes. Skin Pharmacol. Appl. Skin Physiol. 15, 353-359.
36. Savini, I., M. V. Catani, A. Rossi, G. Duranti, G. Melino and L. Avigliano (2002) Characterization of keratinocyte differentiation induced by ascorbic acid: protein kinase C involvement and vitamin C homeostasis. J. Investig. Dermatol. 118, 372-379.
37. Ogura, R., M. Sugiyama, J. Nishi and N. Haramaki (1991) Mechanism of lipid radical formation following exposure of epidermal homogenate to ultraviolet light. J. Investig. Dermatol. 97, 1044-1047.
38. Salari, H., P. Braquet and P. Borgeat (1984) Comparative effects of indomethacin, acetylenic acids, 15-HETE, nordihydroguaiaretic acid and BW755C on the metabolism of arachidonic acid in human leukocytes and platelets. Prostaglandins Leukot. Med. 13, 53-60.
39. Coutant, K. D., N. Corvaia and N. S. Ryder (1997) Bradykinin induces actin reorganization and enhances cell motility in HaCaT keratinocytes. Biochem. Biophys. Res. Commun. 237, 257-261.
40. Hulten, L. M., H. Lindmark, H. Schersten, O. Wiklund, F. N. Nilsson and G. C. Riise (1998) Butylated hydroxytoluene and N-acetylcysteine attenuates tumor necrosis factor-alpha (TNF-alpha) secretion and TNF-alpha mRNA expression in alveolar macrophages from human lung transplant recipients in vitro. Transplantation 66, 364-369.
41. Piette, J., B. Piret, G. Bonizzi, S. Schoonbroodt, M. P. Merville, S. Legrand-Poels and V. Bours (1997) Multiple redox regulation in NF-kappaB transcription factor activation. Biol. Chem. 378, 1237-1245.
42. Flohe, L., R. Brigelius-Flohe, C. Saliou, M. G. Traber and L. Packer (1997) Redox regulation of NF-kappa B activation. Free Radic. Biol. Med. 22, 1115-1126.
43. van Puijenbroek, A. A., S. Wissink, P. T. van der Saag and M. P. Peppelenbosch (1999) Phospholipase A2 inhibitors and leukotriene synthesis inhibitors block TNF-induced NF-kappa B activation. Cytokine 11, 104-110.
44. Slapke, J., T. Schewe, S. Hummel, J. Winkler and M. Kopf (1983) Lung strips from guinea pigs as test system for lipoxygenase inhibitors. Inhibition of arachidonic acid-induced contractions by 3-t-butyl-4-hydroxyanisole and nordihydroguaiaretic acid. Biomed. Biochim. Acta 42, 1309-1318.
Annemie Pupe, Hugo Degreef and Marjan Garmyn*
Department of Dermatology, Katholieke Universiteit Leuven, Leuven, Belgium
*To whom correspondence should be addressed at: Department of Dermatology, UZ Street, Rafael, Kapucijnenvoer 33, B-3000 Leuven, Belgium. Fax: 32-16-346278; e-mail: marjan.garmyn@med.kuleuven.ac.be
Copyright American Society of Photobiology Jul 2003
Provided by ProQuest Information and Learning Company. All rights Reserved