Study objective: To compare the efficacy and safety of ipratropium bromide reformulated with the chlorofluorocarbon (CFC)-free propellant hydrofluoroalkane (HFA)-134a (ipratropium bromide HFA) to that of the marketed ipratropium bromide inhalation aerosol (containing CFC) in patients with COPD.
Design: This was a randomized, double-blind, parallel-group, placebo-controlled, multicenter trial. The primary efficacy parameter was acute bronchodilator response. The primary end points were peak change in [FEV.sub.1] from baseline and area under the response-time curve.
Setting: Thirty-one clinical centers in the United States participated in this project.
Patients: A total of 507 patients with moderate-to-severe COPD were randomized, and 444 patients completed the trial.
Interventions: Twelve weeks of treatment four times daily with one of the following: ipratropium bromide HFA, 42 [micro]g; ipratropium bromide HFA, 84 [micro]g; HFA placebo; ipratropium bromide inhalation aerosol, 42 [micro]g; or CFC placebo.
Measurements and results: Patients in all active treatment groups had significant bronchodilator responses as shown by increases in mean [FEV.sub.1] from baseline of at least 15%. Bronchodilator response in all active treatment groups was also significantly more than their respective placebo treatments based on [FEV.sub.1], area under the time-response curve from 0 to 6 h, and peak response. FVC results were similar to those seen with [FEV.sub.1]. There were no significant differences in adverse events, laboratory findings, or ECG findings among the treatment groups.
Conclusions: Ipratropium bromide HFA, 42 [micro]g, provided bronchodilation comparable to the marketed ipratropium bromide CFC, 42 [micro]g, over 12 weeks of regular use. (CHEST 2001; 120:1253-1261)
Key words: chlorofluorocarbon; COPD; hydrofluoroalkane-134a; ipratropium bromide
Abbreviations: AU[C.sub.0-6] = area under the response-time curve from 0 to 6 h; CFC = chlorofluorocarbon; HFA = hydrofluoroalkane; MDI = metered-dose inhaler
Metered-dose inhalers (MDIs) have historically used chlorofluorocarbons (CFCs) to propel a metered dose of an aerosol drug. During the past several years, the harmful effects of CFC propellants on the concentration of ozone have received worldwide attention. (1) The possibility that CFCs could lead to depletion of the ozone layer was first suggested in 1974 by the Nobel Prize winners Molina and Rowland. (2) International action to reduce CFC use began in 1987 when 23 nations signed the "Montreal Protocol on Substances that Deplete the Ozone Layer." The removal of CFC propellants from industrial and household products has been agreed to by > 165 countries, of which > 135 are developing countries. (3) The pharmaceutical industry has endeavored to develop aerosols with alternatives to CFCs in response to this situation.
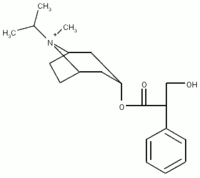
Hydrofluoroalkane (HFA)-134a (1,1,1,2-tetrafluoroethane) has been shown (4-9) to be a suitable replacement for CFCs in MDIs. HFA-134a has environmental advantages over CFCs because it does not contain chlorine and is therefore considered to have no ozone-depleting potential. (10) Preclinical evaluations (11) have demonstrated the acceptability of this propellant in terms of pharmacology, toxicology, and safety. Ipratropium bromide inhalation aerosol (Atrovent; Boehringer Ingelheim; Ridgefield, CT) has been established as a first-line medication for maintenance treatment of bronchospasm in patients with COPD. (12) This drug has been reformulated successfully with the new HFA-134a propellant system. The present study was designed to compare the efficacy and safety of the new Atrovent HFA-134a formulation and the currently marketed Atrovent inhalation aerosol in COPD patients.
MATERIALS AND METHODS
Study Design and Conduct
Thirty-one clinical centers in the United States participated in this project. Each center conformed to the institutional review board and informed consent provisions of Code of Federal Regulations. The study compared the efficacy and safety of two doses of ipratropium bromide HFA to ipratropium bromide inhalation aerosol containing CFC and placebo formulations of each in patients with a diagnosis of COPD who were at least 40 years old and had a smoking history of at least 10 pack-years. Each participant was required to have stable airway obstruction with [FEV.sub.1] [less than or equal to] 65% predicted normal and [FEV.sub.1] [less than or equal to] 70% of the FVC. (13)
An acute bronchodilator test in response to short-acting [[beta].sub.2] agonist was not performed as a selection criterion in this study. Patient selection followed standard COPD selection criteria (14) designed to exclude patients with asthma. Specifically, patients with a history of asthma, allergic rhinitis, atopy, or those who had a total eosinophil count > 600/[micro]L were excluded. Also excluded were patients who required > 10 mg of oral prednisone daily within 6 weeks before entry into the study. Before admission to the trial, each patient had his/her medical history taken and underwent laboratory testing, physical examination, and 12-lead ECG recording; these tests were repeated at the completion of the study.
Five hundred seven patients were selected and randomized into the trial. Visits to the clinic were scheduled once every 2 weeks throughout the treatment period, During these visits, adverse events, use of concomitant medications, and other evaluations were recorded.
While continued use of stable doses of theophylline was allowed during the study (28% of patients were receiving theophylline), regular use of inhaled bronchodilators other than the study drug was not allowed. Temporary increases or additions of theophylline and corticosteroids during exacerbations were permitted but limited to two periods of 5 days and 7 days, respectively, during the 85-day trial. The use of cromolyn sodium, oral [beta]-agonists, and [beta]-blockers was not allowed. Patients were allowed to receive inhaled albuterol for control of symptoms as necessary during the study period.
The study was double blind. A blinding device (blinding jacket) was used to blind all study medications. Therefore, there were no visual differences in the treatment groups. However, the taste of the HFA and CFC formulations were different, HFA formulation contains alcohol and citric acid while CFC formulation does not. Since we had included the placebo of both formulations in this study, patients could not distinguish between the taste of active and placebo treatments of each formulation.
Patient compliance was monitored by patient diary cards. Patients completed a daily worksheet indicating each dose of investigational drug and rescue medication (albuterol) taken. After reviewing this worksheet with the patient, the investigator recorded on the case report forms the patient's usual daily dosing regimen and the number of puffs of albuterol that the patient took during the 2-week period preceding that visit.
Treatments
Following a 2-week baseline period to establish clinical stability, patients were randomly assigned by order of entry to receive one of the following treatments: ipratropium bromide HFA, 42 [micro]g (125 patients); ipratropium bromide HFA, 84 [micro]g (127 patients); HFA placebo (62 patients); ipratropium bromide CFC, 42 [micro]g (127 patients); or CFC placebo (66 patients) [Table 1]. Patient stability was defined based on the patient's respiratory medication (ie, no changes) and the absence of respiratory infections in the preceding 6 weeks. Patients with any viral infection or febrile illness including upper respiratory tract infections during the 6-week period preceding the visit were excluded from participation in the study.
Patients were instructed to receive two inhalations of study medication four times daily. The majority of patients (95 to 100%) reported that they inhaled the drug four times daily during the 85-day treatment period.
Observations
Pulmonary function testing, including measurements of [FEV.sub.1] and FVC, was conducted four times, on treatment days 1, 29, 57, and 85, to assess the consistency of response during the 12-week study period. Testing was done immediately before drug administration, at 15, 30, 60, 90, and 120 min after drug administration, and hourly thereafter, for a total of 8 h. Theophylline treatment was withheld for at least 24 h, and treatment with [beta]-adrenergic bronchodilators and the study drug was withheld for at least 12 h prior to pulmonary function testing. The study drug was administered between 7 AM and 10 AM, after baseline spirometry had been performed. All pulmonary function tests were conducted in triplicate, and the spirometric results with the greatest sum of [FEV.sub.1] and FVC were recorded and used for analysis. Spirometers met American Thoracic Society standards. (15) BP and pulse rates were measured on each test day, just prior to each pulmonary function test for a period of 8 h. Severity of COPD symptoms (wheezing, shortness of breath, coughing, and tightness of chest) was reported at the end of the 2-week baseline period and every 2 weeks thereafter. Investigators rated the severity of symptoms using a 4-point scale: none (0), mild (1), moderate (2), and severe (3). This assessment was based on the patient's condition since the previous visit. This evaluation was made before the start of pulmonary function testing. A global evaluation of each patient's overall condition was made by the investigator at each visit and was expressed as a numerical value from 1 (poor) to 8 (excellent). This global evaluation was based on the physician's assessment of the overall condition of the patient's disease, need for concomitant medication, number and severity of exacerbations, severity of cough, ability to exercise, and amount of wheezing, etc.
Statistical Evaluation
Acute bronchodilator response was measured by changes from baseline in the spirometric variables [FEV.sub.1] and FVC. The primary end points were peak change from baseline and average area under the response-time curve from 0 to 6 h (AU[C.sub.0-6]), as calculated by the trapezoidal rule. (16) [FEV.sub.1] responses were also used to derive the onset of end point and duration of therapeutic response (defined as 15% increase from test-day baseline) and time to peak response. Response was considered terminated when patients no longer demonstrated improvement in [FEV.sub.1] > 15% from the baseline at two consecutive time points. Duration of action was defined as the interval between onset and termination of therapeutic response. The FVC response was similarly evaluated in terms of AU[C.sub.0-6] and peak response.
Analysis of covariance with test-day baseline as the covariate was used to evaluate acute bronchodilator response. Other terms used in the model were treatment, center, and treatment-by-center interaction. The efficacy analysis was performed using intent-to-treat data set. End point analyses (last observation carried forward) were performed to account for withdrawals after day 1.
RESULTS
Subjects and Subject Disposition
A total of 507 patients were randomized into the study, and 444 of these patients completed the trial. The demographic and baseline characteristics of these patients are presented in Table 1. The disposition of the study participants is summarized in Table 2. The highest dropout rate was observed in the CFC placebo group (22.7%). The dropout rates for patients receiving HFA placebo, 84 [micro]g of ipratropium bromide HFA, and 42 [micro]g of ipratropium bromide CFC were all between 11.3% and 14.2%, while the lowest dropout rate was seen in the group receiving ipratropium bromide HFA, 42 [micro]g (6.4%). The most common adverse reactions leading to discontinuation were lower respiratory tract system events, including, acute exacerbations of chronic bronchitis, cough, dyspnea, and pneumonia, which caused the withdrawal of eight patients (12%) receiving CFC placebo; nine patients (7%) receiving ipratropium bromide CFC, 42 [micro]g; two patients (3%) receiving HFA placebo; two patients (2%) receiving ipratropium bromide HFA, 42 [micro]g; and five patients (4%) receiving ipratropium bromide HFA, 84 [micro]g. Between 95% and 100% of all patients in different treatment groups took the study drug four times daily according to diary records.
Efficacy
The baseline [FEV.sub.1] values for the five groups were comparable on each of the 4 test days and were reasonably stable over the course of the study (Table 3). Bronchodilator response in the three active treatment groups was significantly more than their respective placebo treatments based on absolute change in [FEV.sub.1], AU[C.sub.0-6], and peak response (Fig 1). Between 72% and 83% of patients receiving active treatments were classified as responders since they had increases in [FEV.sub.1] of at least 15%. The percentage of nonresponders in each treatment group is shown in Table 4. On test day 1, [FEV.sub.1], [AU[C.sub.0-6], and peak response for ipratropium bromide HFA, 84 [micro]g, were 45 mL and 52 mL higher, respectively, (p < 0.05) than ipratropium bromide CFC, 42 [micro]g. However, on the following test days, all active treatment groups were comparable. There was no statistically significant difference between ipratropium bromide HFA, 84 [micro]g, and ipratropium bromide HEA, 42 [micro]g.
[FIGURE 1 OMITTED]
The median time to onset of a 15% increase in [FEV.sub.1] on the 4 test days ranged from 14.0 to 17.5 min for ipratropium bromide HFA, 42 [micro]g; from 12.5 to 22.0 min for ipratropium bromide HFA, 84 [micro]g; and from 15.0 to 19.0 min for ipratropium bromide CFC, 42 [micro]g. Median time to peak response was 90 min for each of the active treatment groups on test days 1, 29, and 57. On day 85, median time to peak response was 90 min for ipratropium bromide HFA, 42 [micro]g, and 60 min for ipratropium bromide HFA, 84 [micro]g, and ipratropium bromide CFC, 42 [micro]g.
Median durations of action, defined as 15% increases from test-day baseline values, are summarized in Table 5. Median duration of action on the 4 test days ranged from 2.3 to 3.1 h for ipratropium bromide CFC, 42 [micro]g; 2.0 to 2.8 h for ipratropium bromide HFA, 42 [micro]g; and 1.6 to 4.1 h for ipratropium bromide HFA, 84 [micro]g. Pairwise comparisons of ipratropium bromide CFC, 42 [micro]g, vs ipratropium bromide HFA, 42 [micro]g, and ipratropium bromide HFA, 84 [micro]g, showed that differences between the groups were not statistically significant.
FVC results were similar to those seen with [FEV.sub.1] (Fig 2). On all test days, the two dosage strengths of ipratropium bromide HFA (42 [micro]g and 84 [micro]g) were significantly more effective than HFA placebo based on FVC, AU[C.sub.0-6], and peak response, ipratropium bromide CFC, 42 [micro]g, was significantly more effective than CFC placebo on all test days for FVC AU[C.sub.0-6].
[FIGURE 2 OMITTED]
With respect to [FEV.sub.0], all three active treatment groups were shown to be comparable on 3 of 4 test days. On test day 1, ipratropium bromide HFA, 84 [micro]g, was significantly more effective than ipratropium bromide CFC, 42 [micro]g, in terms' of [FEV.sub.1], AU[C.sub.0-6], and peak response.
Other Efficacy Variables
Adjusted mean physician's global evaluation scores were between 4.8 to 5.4 for all treatment groups, which represent a rating of "fair to good." The COPD symptom scores (wheezing, shortness of breath, coughing, and tightness of chest) did not change over time and did not differ among the placebo and active treatment groups. In general, they were of mild severity. During any 2-week treatment period, there was no difference in the percentage of patients who reported using their study drug more often than four times daily (range, 0 to 2% of patients).
On average, patients were using albuterol for rescue medication approximately two to three times per day. Patients in the placebo groups reported slightly higher use of albuterol. There was no difference in the use of albuterol in the active treatment groups.
Safety
Adverse events included any new or worsened condition without respect to any possible relationship to study medication. In general, the incidence of adverse events was similar across all treatment groups. The most frequently occurring adverse events were COPD exacerbations and upper respiratory tract infections. Adverse events that were possibly drug related were reported in 6 patients (4.8%) receiving ipratropium bromide HFA, 42 [micro]g; 10 patients (7.9%) receiving ipratropium bromide HFA, 84 [micro]g; 8 patients (12.9%) receiving HFA placebo; 17 patients (13.4%) receiving ipratropium bromide CFC, 42 [micro]g; and six patients (9.1%) receiving CFC placebo. The most common adverse event that was judged possibly related to therapy was headache, which was reported in up to 3.1% of patients in different treatment groups. Six patients (1.2%) died during the study period: one patient (1.6%) in the group receiving HFA placebo (cause of death, pulmonary carcinoma); four patients (3.2%) in the group receiving ipratropium bromide HFA, 42 [micro]g (cause of death, COPD exacerbation in two patients, pulmonary carcinoma in one patient, and pancreatitis in one patient); and one patient (0.8%) in the group receiving ipratropium bromide HFA, 84 [micro]g (cause of death, pulmonary carcinoma). None of the six deaths were reported to be related to the study drug.
The most common adverse event leading to patient discontinuation was COPD exacerbation. This event was reported in two patients (1.6%) in the group receiving ipratropium bromide HFA, 42 [micro]g; four patients (3.1%) in the group receiving ipratropium bromide HFA, 84 [micro]g; two patients (3.2%) in the group receiving HFA placebo; seven patients (5.5%) in the group receiving ipratropium bromide CFC, 42 [micro]g; and four patients (6.1%) in the group receiving CFC placebo. All adverse events occurring in > 3% of the patients are shown in Table 6.
There were no clinically significant changes from baseline in mean laboratory values, or BP and pulse rate following treatment, nor were there any clinically significant differences in these parameters in the five treatment groups. Clinically significant ECG findings, as determined by the investigator, were reported for five patients. None of the findings were related to the study drug. The clinically significant ECG findings were reported in one patient receiving HFA placebo; three patients receiving ipratropium bromide HFA, 84 [micro]g; and one patient receiving ipratropium bromide CFC, 42 [micro]g.
DISCUSSION
Ipratropium bromide is a well-established bronchodilator for the maintenance treatment of COPD (12) and remains the lone agent in the class of anticholinergics in the United States. As the MDI is the most common dose form of this drug, the need to provide a safe and effective alternative to the currently used CFC propellant is an important public health initiative.
The formulation of ipratropium bromide using the alternative propellant HFA was an important first step as the general safety and tolerability of the propellant itself has been established. (4) Nevertheless, the drug-device combination using this new formulation in clinical trials was needed to ensure, at a minimum, comparable safety and efficacy to the innovator CFC product. Such clinical testing is prudent, as the changes to the ultimate product involve an array of pharmaceutical considerations, ranging from suitable additives, suitable sealing elastomers, optimization of the actuator, and development or optimization of the manufacturing technique for mass production. (17) As in vivo studies have indicated that the fine-particle dose of ipratropium bromide-containing HFA propellant is comparable to that of the CFC product, the clinical program had a reasonable basis for demonstrating comparability.
In this study, both formulations of ipratropium bromide provided superior bronchodilation compared to their respective placebo treatments, as would be expected. Importantly, the spirometric efficacy of the currently marketed 42-[micro]g CFC aerosol was comparable to the HFA product, thus supporting a dose-for-dose switch between the two formulations. Such dose-for-dose comparability is consistent with other bronchodilators, including albuterol (7-9) and the combination formulation of ipratropium bromide/fenoterol, (18) as well as for the mediator-modifying compound cromolyn. (19) This is in contrast to the formulation of beclomethasone for asthma, where significant reduction of particle size from the HFA formulation resulted in marketing of a reduced dose for comparable effects. (20)
In the current study, there was no significant difference observed between 49 [micro]g and 84 [micro]g of HFA ipratropium bromide, which is consistent with previous single-dose trials (21) that found these two doses on the plateau of the dose-response curve. While there was a difference noted between 84-[micro]g HFA and 42-[micro]g CFC that was limited to the first test day, analysis of the 4 test days reveals an atypically small 49-[micro]g CFC response on this initial test day. The difference in the first test day may have been a simple chance finding.
There was a small but statistically significant difference between placebo and active CFC formulation with regard to the use of albuterol as rescue medication. Placebo patients, on average, used slightly more albuterol during the study period. A possible explanation for a lack of a larger difference between active and placebo groups is that patients were not specifically instructed to try to decrease the use of rescue medication. Therefore, they continued to use albuterol as it was used prior to participation in the study.
The incidence of side effects that are common to the anticholinergic class was low and similar among different treatment groups. For example, dry mouth (4.8% and 2.4%) and taste perversion (0% and 0.8%) were in reported groups receiving ipratropium bromide HFA, 42 [micro]g, and ipratropium bromide CFC, 42 [micro]g, respectively.
In summary, the results of this study show that ipratropium bromide HFA, 42 [micro]g, can provide both similar clinical benefit as the currently marketed ipratropium bromide CFC, 42 [micro]g, formulation, and a comparable tolerability profile. This supports a smooth transition for patients with COPD when prescribed the new formulation of ipratropium bromide.
APPENDIX
The study investigators are as follows: Roblee Allen, MD, Sacramento, CA; Theodore Amgott, MD, Melbourne, FL; Horst Blumberg, MD, St. Petersburg, FL; Shari Anne Brazinsky, MD, San Diego, CA; James R. Castle, MD, Roanoke, VA; Peter J. Costantini, PharmD, DO, Pleasantville, NJ; William T. Ellison, MD, Greer, SC; Joe Garcia, MD, Indianapolis, IN; W. Thomas Garland, MD, Lawrenceville, NJ; Michael Goldman, MD, Los Angeles, CA; Fredrie Jackson, MD, Seattle, WA; Mitchell Kaye, MD, Minneapolis, MN; Steven Knoper, MD, Tucson, AZ,; Arthur Kotch, MD, Danbury, CT; Stephen M. Kreitzer, MD, Tampa, FL; Robert Lapidus, MD, Wheat Ridge, CO; H. Charles Miller, MD, Cincinnati, OH; K. Scott Miller, MD, Charleston, SC; M. Brooke Nicotra, MD, Tyler, TX; Bohdan Pichurko, MD, Detroit, MI; Kathryn L. Rice, MD, Minneapolis, MN; Andrew Ries, MD, San Diego, CA; Joseph Sokolowski, MD, Cherry, Hill, NJ; James Taylor, MD, Tacoma, WA; James Tita, MD, Toledo, OH; Michael P. Tonner, MD, Vero Beach, FL; Bernhard Votteri, MD, Redwood City, CA; Andrew S. Wachtel, MD, Los Angeles, CA; Laurence A. Weiss, MD, Hallandale, FL; Lewis Wesselius, MD, Kansas City, MO; and Jan Westennan, MD, Lackland AFB, TX.
REFERENCES
(1) Hayman GD. CFCS and the ozone layer. Br J Clin Pract Suppl 1997; 89:2-9
(2) Molina MJ, Rowland FS. Stratospheric sink for chlorofluoromethanes: chlorine atom catalyzed destruction of ozone. Nature 1974; 249:810-814
(3) Dolovich M. New delivery systems and propellants. Can Respir J 1999; 6:290-295
(4) Harrison LI, Donnel D, Simmons JL, et al. Twenty-eight-day double-blind safety study of an HFA-134a inhalation aerosol system in healthy subjects. J Pharm Pharmacol 1996; 48:596-600
(5) Dahl R, Ringdal N, Ward SM, et al. Equivalence of asthma control with new CFC-free formulation HFA-134a beclomethasone dipropionate and CFC-beclomethasone dipropionate. Br J Clin Pract 1997; 51:11-15
(6) Donnell D, Harrison LI, Ward S, et al. Acute safety of the CFC-free propellant HFA-134a from a pressurized metered dose inhaler. Eur J Clin Pharmacol 1995; 48:473-477
(7) Bleecker ER, Tinkelman DG, Ramsdell J, et al. Proventil HFA provides bronchodilation comparable to Ventolin over 12 weeks of regular use in asthmatics. Chest 1998; 113:283-289
(8) Tinkleman DG, Bleecker ER, Ramsdell J, et al. Proventil HFA and Ventolin have similar safety profiles during regular use. Chest 1998; 113:290-296
(9) Dockhorn RJ, Wagner DE, Burgess GL, et al. Proventil HFA provides protection from exercised-induced bronchoconstriction comparable to Proventil and Ventolin. Ann Allergy Asthma Immunol 1997; 79:85-88
(10) Hayman G. Why the environment matters. Br J Clin Pratt Suppl 1995; 49:2-6
(11) CPMP on possible alternatives to CFCs. Scrip-World Pharmaceutical News 1994; 1943:26
(12) Ferguson GT, Cherniack RM. Management of chronic obstructive pulmonary disease. N Engl J Med 1993; 328:1017-1022
(13) Morris JF, Koski A, Temple WP, et al. Fifteen-year interval spimmetric evaluation of the Oregon predictive equations. Chest 1988; 93:123-127
(14) American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD). Am J Respir Crit Care Med 1995; 152:S77-S120
(15) American Thoracic Society. Standardization of spirometry. Am J Respir Crit Care Med 1995; 152:1107-1136
(16) Munen MA, Foulis, DJ. Approximation of definite integrals: the trapezoidal rule and Simpson's rule. In: Simens GF, ed. Calculus with analytic geometry. 2nd ed. New York, NY: McGraw Hill, 1984; 338-341
(17) Tansey I. The technical transition to CFC-free inhalers. Br J Clin Pratt Suppl 1997; 89:22-27
(18) Maesen FP, Greefhorst LPM, Smeets JJ, et al. Therapeutic equivalence of a novel HFA-134a containing metered dose inhaler and the conventional CFC inhaler (Berodual) for the delivery of a fixed combination of fenoterol/ipratropium bromide: a randomized double-blind, placebo-controlled crossover study in patients with asthma. Respiration 1997; 64:273-280
(19) Blumenthal MN, Casale TB, Fink JN, et al. Evaluation of non-chlorofluorocarbon formulation of cromolyn sodium (Intal) metered-dose inhaler versus the chlorofluorocarbon formulation in the treatment of adult patients with asthma: a controlled trial. J Allergy Clin Immunol 1998; 101:7-13
(20) Vanden Burgt JA, Busse WW, Martin RJ, et al. Efficacy and safety overview of a new inhaled corticosteroid, QVAR (hydrofluoroalkane-beclomethasone extrafine inhalation aerosol), in asthma. J Allergy Clin Immunol 2000; 106:1210-1226
(21) Floreani A, Henderson W, Sokolowski J, et al. Dose response study of ipratropium bromide dry powder (IBDP) in patients with chronic obstructive pulmonary disease (COPD) [abstract]. Chest 1998; 114(suppl):318S
James Taylor, MD, FCCP; Arthur Kotch, MD, FCCP; Kathryn Rice, MD, FCCP; Mo Ghafouri, PhD; Caryn L. Kurland, PhD; Nora M. Fagan, MS; Theodore J. Witek, Jr, DrPH; and the Ipratropium Bromide HFA Study Group ([dagger])
* From Pulmonary Consultants (Dr. Taylor), Tacoma, WA; Danbury Hospital (Dr. Kotch), Danbury, CT; VA Medical Center (Dr. Rice), Minneapolis, MN; and Boehringer Ingelheim Pharmaceuticals, Inc. (Drs. Ghafouri, Kurland, Witek, and Ms. Fagan), Ridgefield, CT.
([dagger]) The study investigators are listed in the Appendix.
This study was supported by a grant from Boehringer Ingelheim Pharmaceuticals, Inc., Ridgefield, CT.
Dr. Ghafouri, Dr. Witek, and Ms. Fagan are employed by Boehringer Ingelheim Pharmaceuticals, Inc. Dr. Kurland is a former employee of Boehringer Ingelheim Pharmaceuticals, Inc. Manuscript received May 24, 2000; revision accepted May 1, 2001.
Correspondence to: Mo Ghafouri, PhD, Senior Associate Director, Clinical Research, Boehringer Ingelheim Pharmaceuticals, Inc., 900 Ridgebury Rd, PO Box 368, Ridgefield, CT 06877-0368; e-mail: mghafour@rdg.boehringer-ingelheim.com
COPYRIGHT 2001 American College of Chest Physicians
COPYRIGHT 2001 Gale Group