Pulmonary hypertension (PH) results from constriction and remodeling of pulmonary vessels. Serotonin contributes to both phenomena through different signaling pathways. The mitogenic effect of serotonin on pulmonary vascular smooth muscle cells is mediated by the serotonin transporter (5-hydroxytryptamine transporter [5-HTT]), whereas its constricting effect is mediated by 5-HT^sub 1B/1D^ and 5-HT^sub 2A^ receptors. Here, we investigated the respective roles of 5-HTT and 5-HT receptors on the development of chronic hypoxic PH in mice. During exposure to hypoxia (10% O2 for 2 weeks), the animals received one of the specific 5-HTT inhibitors citalopram and fluoxetine (10 mg/kg/day), the selective 5-HT^sub 1B/1D^ receptor antagonist GR127935 (2 and 10 mg/kg/day), or the 5-HT^sub 2A^ receptor antagonist ketanserin (2 mg/kg/day). Mice treated with the 5-HTT inhibitors showed less right ventricle hypertrophy (ratio of right ventricle/left ventricle + septum = 36.7 + or - 2.0% and 35.8 + or - 1.3% in citalopram- and fluoxetine-treated mice, respectively, vs. 41.5 + or - 1.5% in vehicle-treated mice) and less pulmonary vessel muscularization (p
Keywords: pulmonary hypertension; serotonin transporter; chronic hypoxia; serotonin receptors
Pulmonary hypertension (PH) occurs either as a complication of various abnormal conditions or as a primary disease for which no underlying cause can be found (1). Persistent vasoconstriction and structural remodeling of the pulmonary vessels are cardinal features of PH (2) but remain largely unexplained. Serotonin (5-hydroxytryptamine [5-HT]) has been suggested to play a major role in the pathogenesis of PH (3). Vasoconstriction occurs when 5-HT binds to 5-HT^sub 2^ and 5-HT^sub 1B/1D^ receptors expressed by pulmonary smooth muscle cells (4, 5). In addition, once internalized by a high-affinity selective transporter, 5-HT exerts potent mitogenic and comitogenic effects on pulmonary artery smooth muscle cells (PA-SMCs) (6-8). The 5-HT transporter (5-HTT) is abundantly expressed in the lung (9) and is the target of appetite suppressant drugs reported to increase the risk of primary PH (10, 11). In recent studies of lung tissues and pulmonary arteries from patients undergoing lung transplantation to treat primary PH, we found increased expression of 5-HTT and marked enhancement of the proliferative growth response of cultured PA-SMCs to 5-HT but not to other growth factors (12). Additional data suggested that the increased expression of 5-HTT in these patients was related to polymorphism of the 5-HTT gene promoter (12). A role for 5-HTT in experimental hypoxic PH has also been clearly established (13). Therefore, 5-HT, most notably through its specific transporter, appears to be a key player in the pathogenesis of various types of human and experimental PH.
Drugs such as fluoxetine and paroxetine competitively inhibit 5-HTT (14) and, therefore, abolish the in vitro proliferative response of PA-SMCs to 5-HT and also, to a large extent, to serum (8). However, their effects on the development of PH have not been investigated. We reasoned that antidepressant drugs capable of inhibiting 5-HTT may inhibit PA-SMC proliferation and prevent structural remodeling of blood vessels during PH development, not only in vitro but also in vivo. Hypoxic PH results from both constriction and remodeling of the pulmonary vessels and, consequently, offers the opportunity to compare the effects of 5-HTT inhibitors with those of 5-HT receptor antagonists. Selective effects would be expected, with 5-HTT inhibitors selectively blocking PA-SMC proliferation and 5-HT receptor antagonists selectively reducing 5-HT-induced pulmonary vasoconstriction. In this study, we investigated the respective roles of 5-HT receptors and 5-HTT on the development of chronic hypoxic PH in mice. For this purpose, we treated mice with one of the specific 5-HTT inhibitors citalopram and fluoxetine (14), with the selective 5-HT^sub 1B/1D^ receptor antagonist GR127935 (15) or with the 5-HT^sub 2A^ receptor antagonist ketanserin (16).
METHODS
Animal Models and Experimental Design
All experiments were performed using adult male mice (8-week-old C57BL6/J) according to institutional guidelines that comply with national and international regulations.
Hemodynamic Response of Normoxic Mice to Acute Hypoxia
Mice were anaesthetized with ketamine (6 mg/100 g. intraperitoneally) and xylazine (1 mg/100 g, intraperitoneally). The trachea was cannulated, and the lungs were ventilated with room air at a tidal volume of 0.2 ml and a rate of 90 breaths per minute. Systemic arterial pressure was determined by catheterization of the carotid artery. A 26-gauge needle was then introduced percutaneously into the right ventricle (RV) via the subxyphoid approach. Right ventricular systolic pressure (RVSP) was measured using a Gould P10 EZ pressure transducer connected to pressure modules and a Gould TA 550 recorder. RVSP and heart rate were recorded while the animal was ventilated with room air and then after 5 minutes of ventilation with a hypoxic gas mixture (8% O2, 92% N^sub 2^). The heart rate under these conditions was between 300 and 400 beats per minute. If the heart rate fell below 300 beats per minute, measurements were excluded from analysis.
Exposure to Chronic Hypoxia
Mice were exposed to chronic hypoxia (10% O2) in a ventilated chamber (500-L volume; Flufrance, Cachan, France), as previously described (13). To establish the hypoxic environment, the chamber was flushed with a mixture of room air and nitrogen, and the gas was recirculated. The chamber environment was monitored using an oxygen analyzer (Servomex OA150, Crowborough, UK). Carbon dioxide was removed by soda lime granules, and excess humidity was prevented by cooling the recirculation circuit. The chamber temperature was maintained at 22-24[degrees]C. The chamber was opened every other day for 1 hour to clean the cages and replenish food and water supplies. Normoxic mice were kept in the same room with the same light-dark cycle.
Assessment of PH
Mice previously exposed to hypoxia or room air for 2 weeks were anesthetized and ventilated with room air as described previously here. After incision of the abdomen, a 26-gauge needle connected to a pressure transducer was inserted into the RV, and RVSP was recorded immediately. Blood was then sampled for hematocrit determination. Finally, the animals were deeply anesthetized with sodium pentobarbital (4 mg/100 g, intraperitoneally) and exsanguinated, and their thorax was opened to remove the lungs and heart. The RV was dissected from the left ventricle + septum (LV + S), and these dissected samples were weighed.
The lungs were fixed by intratracheal infusion of 4% aqueous buffered formalin at a pressure of 23 cm H2O. The entire specimen was immersed in a bath of the same fixative for 1 week. A midsagittal slice of the right lung including the apical, azygous, and diaphragmatic lobes was processed for paraffin embedding. Sections (5 [mu]m thick) were cut for light microscopy and stained with hematoxylin-phloxin-saffron and orcein-picroindigo-carmine.
In each mouse, 50-60 intraacinar vessels accompanying either alveolar ducts or alveoli were analyzed by an observer blinded to treatment. Each vessel was categorized as nonmuscularized (no evidence of any vessel wall muscularization), partially muscularized (SMCs identifiable in less than three-fourths of the vessel circumference), or fully muscularized (SMCs in more than three-fourths of the vessel circumference). Muscularization was defined as the presence of typical SMCs stained red with phloxin, each exhibiting an elongated shape and square-ended nucleus and bound by two orcein-stained elastic laminae. The percentage of pulmonary vessels in each muscularization category was determined by dividing the number of vessels in that category by the total number counted in the same experimental group.
Pharmacologic Treatments
To investigate the effects of 5-HTT inhibition and/or 5-HT receptor blockade on acute hypoxic vasoconstriction, nine groups of mice (six to seven in each group) were studied. Inhibition of 5-HTT was achieved by administering citalopram or fluoxetine (10 mg/kg/day, in distilled water by gavage) in the first two groups. Two other groups were treated with the 5-HT^sub 2A^ receptor antagonist ketanserin or the 5-HT^sub 1B/1D^ receptor antagonist GR127935, both in a dosage of 2 mg/kg/day, intraperitoneally. Four additional groups were treated with a combination of one 5-HTT inhibitor and one 5-HT receptor antagonist. The last group consisted of control animals that received vehicles. The treatments were given for 2 days, and acute hypoxic vasoconstriction was measured on the following day 1 hour after the last treatment.
The effect of 5-HTT inhibition and/or 5-HT receptor blockade was assessed in mice exposed to normoxia or to hypoxia during 15 days. Six groups of normoxic mice (six mice in each group) and six groups of chronically hypoxic mice (10-14 in each group) were treated once a day with citalopram (10 mg/kg/day), fluoxetine (10 mg/kg/day) (17, 18), ketanserin (2 mg/kg/day) (19), GR127935 (2 and 10 mg/kg/day) (20, 21), or vehicle. An additional group was treated with both fluoxetine (10 mg/kg/day) and GR127935 (2 mg/kg/day).
Effect of 5-HT on Proliferation of Human PA-SMCs
The methods used to culture and to characterize human PA-SMCs have been previously described (12). In brief, PA-SMCs were obtained from patients undergoing lung resection for cancer. They were seeded in 24-well plates at a density of 5 x 10^sup 4^ cells/well and were allowed to adhere in Dulbecco's modified Eagle medium supplemented with 15% fetal calf serum. The cells were then subjected to 48 hours of growth arrest in medium containing only 0.2% fetal calf serum before being incubated in Dulbecco's modified Eagle medium supplemented with 0.2% fetal calf serum, 0.6 mM of ascorbic acid, 0.1 mM of iproniazid (a monoamine oxidase inhibitor), and 0.6 [mu]Ci/ml of [^sup 3^H]thymidine, with or without 5-HT (10^sup -8^ to 10^sup -6^ M). The effect of 5-HT was also examined in the presence of 10^sup -6^ M of fluoxetine, citalopram, GR127935, ketanserin, or the 5-HT^sub 2B/2C^ receptor antagonist SB206553 (16). Each of these drugs was added 20 minutes before 5-HT. After incubation for 24 hours, the cells were washed twice with phosphate-buffered saline, treated with ice-cold 10% trichloroacetic acid (1 ml/well), and dissolved in 0.1 N NaOH (0.5 ml/well). The incorporated radioactivity was counted and reported as counts per minute per well.
Chemicals
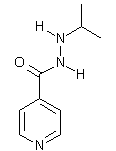
[^sup 3^H]Thymidine was from Amersham Pharmacia Biotech (Buckingham, UK). Iproniazid, ascorbic acid, 5-HT, and SB206553 (N-3-pyridinyl-3,5-dihydro-5-methyl-benzo[1,2-b:4,5-b']dipyrrole-1[2H]-carboxamide hydrochloride) were from Sigma (St. Louis, MO). The other compounds were fluoxetine (Eli Lilly, Indianapolis, IN), citalopram (Lundbeck, Copenhagen, Denmark), ketanserin (Janssen, Beerse, Belgium), GR127935 (2'-methyl-4'-(5-methyl-[1,2,4]oxadiazol-3-yl)-biphenyl-4-carboxylic acid [4-methoxy-3-(4-methyl-piperazine-1yl)-phenyl]amide; GlaxoSmithKline, Harlow, UK).
Statistical Analyses
To compare the effects of pretreatment with 5-HTT inhibitors or 5-HT receptor antagonists on pressure changes caused by acute hypoxia, two-way analysis of variance with repeated measurements was performed: Significance was tested for pretreatment effect, RVSP under normoxic and hypoxic conditions, and interaction. When interaction was significant, the Mann-Whitney nonparametric test was used to compare the effects of the treatments.
One-way analysis of variance was performed to compare hemodynamic values in mice treated with vehicle or active drugs during continuous exposure to chronic hypoxia. When analysis of variance indicated significant differences between groups, Scheffe's method was used to compare those groups. Between-group comparisons of ratios of RV over LV + S (RV/LV + S) weights and of hematocrits were performed using a similar statistical analysis alter arcsine transformation of individual values.
To compare the degree of pulmonary vessel muscularization in the various groups of animals, the vessels were ordinally classified as nonmuscularired, partially muscularized, and fully muscularized (discussed previously here). Muscularization was compared at both the alveolar duct and the wall levels, using the nonparametric Kruskal-Wallis test. When a significant difference was observed (p
All results are expressed as means + or - SEM.
RESULTS
Effects of 5-HTT Inhibitors or 5-HT Receptor Antagonists on 5-HT-induced PA-SMC Proliferation
In cells cultured in 0.2% fetal calf serum, 5-HT (10^sup -8^ to 10^sup -6^ M) produced a concentration-dependent increase in [^sup 3^H]thymidine incorporation (Figure 1). Pretreatment of the cells with fluoxetine (10^sup -6^ M) or citalopram (10^sup -6^ M), two 5-HTT inhibitors, completely abolished the 5-HT-induced increase in [^sup 3^H]thymidine incorporation. In contrast, the mitogenic response to 5-HT was not affected by incubation of the cells with any of the receptor antagonists, namely, GR127935, ketanserin, and SB 206553, all tested at 10^sup -6^ M (Figure 1). Doses of fluoxetine or citalopram as low as 10^sup -7^ M completely abolished the PA-SMC growth response to 5-HT, whereas doses of 5-HT receptor antagonists as high as 10^sup -5^ M failed to affect this response.
Effects of 5-HTT Inhibitors and 5-HT Receptor Antagonists on Response to Acute Hypoxia
Exposure to acute hypoxia (10% O2) induced an increase in RVSP in each of the control mice, reaching a maximum at 5 minutes. Two days of pretreatment with a 5-HTT inhibitor, that is, citalopram or fluoxetine, did not alter baseline RVSP but potentiated its increase in response to acute hypoxia, to 172% and 142% of the pressor response in vehicle-treated control subjects, respectively (p
Effects of Chronic Treatment with 5-HTT Inhibitors or 5-HT Receptor Antagonists on Physiologic Parameters during Normoxia
Treatment with either a 5-HTT inhibitor or a 5-HT receptor antagonist did not alter body weight, heart rate, or systemic arterial pressure. Mean systemic arterial pressure, which was 88 + or - 7 mm Hg in the control mice, remained unchanged after treatment with fluoxetine (86 + or - 5 mm Hg), citalopram (87 + or - 7 mm Hg), GR127935 (85 + or - 6 mm Hg), or ketanserin (83 + or - 4 mm Hg). None of these drugs affected RVSP (Figure 3A) or the RV/LV + S ratio (Figure 3B). Muscularization of distal pulmonary arteries, which was less than 5% in the normoxic animals (Figure 4), was not affected by these drugs.
Effects of 5-HTT Inhibitors and 5-HT Receptor Antagonists on the Development of PH
RVSP. After 2 weeks of exposure to hypoxia (10% O2) combined with daily administration of citalopram, fluoxetine, GR127935, ketanserin, or vehicle, no differences in body weight, heart rate, or hematocrit were found among the corresponding groups of mice (Table 1).
Exposure to hypoxia produced a significant increase in RVSP (31.2 + or - 0.6 mm Hg as compared with 17.5 + or - 0.7 mmHg in mice maintained in normoxia, p
Right ventricular hypertrophy. At the end of exposure to chronic hypoxia, LV + S weight in the hypoxic mice did not differ from that in the mice maintained under normoxic conditions (Table 1) whether the hypoxic animals were treated with fluoxetine, citalopram, ketanserin, GR127935, or vehicle. However, exposure to chronic hypoxia was associated with right ventricular hypertrophy, as assessed by the RV/LV+S ratio (41.5 + or - 1.5% vs. 25.5 + or - 1.3% in hypoxic and normoxic vehicle-treated mice, respectively; Figure 3B). Right ventricular hypertrophy was less marked in the chronically hypoxic mice treated with citalopram or fluoxetine than in those given the vehicle (Figure 3B). In contrast, in mice treated with GR127935 (2 or 10 mg/kg/day) or ketanserin, the RV/LV + S ratio did not differ from that measured in the hypoxic vehicle-treated mice. Moreover, combined treatment with GR127935 plus fluoxetine had no additional effect on right ventricular hypertrophy, as compared with fluoxetine alone (data not shown). Under normoxic conditions, none of these treatments affected the RV/LV + S ratio (Figure 3B).
Pulmonary vascular remodeling. As compared with normoxic mice treated with vehicle, exposure to chronic hypoxia induced muscularization of the distal pulmonary arteries (p
DISCUSSION
In this study, antidepressant drugs that selectively inhibit the serotonin transporter protected against the development of hypoxic PH in mice. These drugs inhibited the proliferation of pulmonary vascular SMCs in vitro and impaired hypoxia-induced pulmonary vascular remodeling in vivo. In contrast, serotonin receptor antagonists, which did not affect SMC proliferation, had no effect on pulmonary vascular remodeling. We found that 5-HTT inhibitors potentiated the pulmonary pressure response to hypoxia, whereas some 5-HT receptor antagonists reduced it. This suggests that structural remodeling of pulmonary blood vessels in response to hypoxia can be reduced independently from an effect on pulmonary vascular tone.
Hypoxia is a well recognized stimulus for pulmonary blood vessel remodeling. Classically, chronic hypoxic PH is ascribed to vascular remodeling in response to sustained pulmonary vasoconstriction and to the subsequent increase in pulmonary artery pressure, which presumably trigger hypertrophy and proliferation of the vascular SMCs. Another mechanism possibly involved in this effect is a direct influence of hypoxia on the expression of specific genes controlling SMC proliferation (22). Recent studies showed that mice with targeted disruption of the 5-HTT gene (5-HTT knockout mice) developed less severe hypoxic PH than wild-type control subjects (13), pointing to 5-HTT as a key effector for pulmonary vascular remodeling in response to hypoxia.
The serotonin transporter can be selectively inhibited by antidepressant drugs such as fluoxetine and citalopram (14). As previously reported (8), we confirmed here that these 5-HTT inhibitors, but not the 5-HT^sub 2A^ receptor antagonist ketanserin, the 5-HT^sub 2B/2C^ receptor antagonist SB 206553, or the 5-HT^sub 1B/1D^ receptor antagonist GR127935, inhibited the mitogenic effect of 5-HT on human PA-SMCs. In addition, as expected from such an effect, we found that mice exposed to hypoxia and treated with fluoxetine or citalopram developed less severe PH than the vehicle-treated animals. Not only was RVSP lower, but right ventricular hypertrophy and pulmonary vessel muscularization were also considerably less marked in the 5-HTT inhibitor-treated mice than in the vehicle-treated control subjects. These findings indicate that the ability of these antidepressants to diminish PA-SMC proliferation was responsible for the attenuation of PH.
Interestingly, mice treated with either fluoxetine or citalopram showed a potentiated pulmonary pressure response to acute hypoxia, as compared with vehicle-treated control subjects. In previous studies, we also observed that the pulmonary pressure response to hypoxia was increased in 5-HTT knockout mice (13). One possible explanation is that inhibition of 5-HT uptake by platelets or vascular cells left more indoleamine available for binding to 5-HT receptors on pulmonary SMCs in the citalopram- and fluoxetine-treated mice. This hypothesis is consistent with in vitro observations that serotonin potentiates hypoxia-induced pulmonary vasoconstriction (23, 24). Moreover, in an earlier study in conscious rats, we found that 5-HT infusion potentiated the acute pulmonary pressure response to hypoxia (25). Our present results showing blunting of the pulmonary pressure response to hypoxia in mice treated with the 5-HT^sub 1B^ receptor antagonist GR127935 are consistent with this hypothesis. They also suggest that endogenous serotonin may contribute to the degree of hypoxic vasoconstriction. Indeed, serotonin is synthesized in the lung, most notably by neuroendocrine cells, and lung production of serotonin increases during hypoxia (26-28).
That 5-HTT inhibition, on the one hand, protected against vascular remodeling but, on the other hand, increased vascular tone should be viewed as a physiological paradox. Indeed, in most cases, physiologic or pharmacologic conditions associated with decreased pulmonary vascular tone protect against PH, whereas increased vascular tone has the opposite effect (29). We reasoned that if increased availability of 5-HT for 5-HT receptors was responsible for the increased vasomotor tone in response to 5-HTT inhibition, treatment with 5-HT receptor antagonists would abolish this increase in tone, thereby providing additional benefits. We therefore examined the effects of pharmacological blockade of the 5-HT receptors most likely to be involved, namely, 5-HT^sub 1B^ and 5-HT^sub 2A^ receptors, which have previously been shown to mediate pulmonary constriction in response to 5-HT (5). When GR127935 was given in association with citalopram or fluoxetine, the presser response to acute hypoxia, which was expected to be enhanced by the 5-HT uptake blockade, was not significantly different from that observed in the absence of drugs. On the other hand, neither GR127935 nor ketanserin affected the development of PH caused by chronic hypoxia, and the combination of GR127935 plus fluoxetine was not more effective than fluoxetine alone in attenuating this phenomenon. Several conclusions can be drawn from these results. First, the pressure response to hypoxia, which is considered an important contributor to pulmonary arterial muscularization, may not fully explain the pathophysiology of hypoxic PH. Second, SMC proliferation, which represents the main component of pulmonary vascular remodeling, may be viewed as a process unrelated to the severity of hypoxic pulmonary vasoconstriction but closely linked to 5-HTT activity. Third, 5-HT^sub 1B/1D^ or 5-HT^sub 2A^ receptors, which mediate serotonin-induced constriction of pulmonary vessels, seem considerably less effective than 5-HTT in mediating pulmonary vascular remodeling.
These results contrast with a previous study in which knockout mice unable to express 5-HT^sub 1B^ receptors (5-HT^sub 1B^-/-) developed less severe PH and vascular remodeling than did wild-type control subjects (21). The apparent discrepancy between this study and ours is probably related to differences in the severity of PH. In our study, the PH was more severe in the hypoxic control mice, with greater pulmonary vascular remodeling and, probably a smaller relative contribution of pulmonary vasoconstriction, as compared with the study in knockout mice (21). Recent work also showed that 5-HT^sub 2B^ receptors were involved in hypoxia-induced PH in mice (30). Again, pulmonary vascular remodeling was far less severe than in this study, and this difference is a major obstacle to comparisons of the respective importance of 5-HT^sub 2B^ receptors versus the 5-HTT. It should also be emphasized that the mechanisms by which 5-HT^sub 2B^ receptors affect the pulmonary vasculature are presently unknown. Indeed, the 5-HT^sub 2B^ receptors are not involved in serotonin-induced SMC proliferation, as shown in this study, nor do they play a role in hypoxic pulmonary vasoconstriction, as reported in the article cited previously here (30).
It is noteworthy that 5-HTT is also the target of appetite suppressant drugs reported to increase the risk of primary PH (10). Dexfenfluramine shares with citalopram and fluoxetine an ability to inhibit platelet 5-HT uptake, but also exerts other effects (31). It triggers the release of serotonin from platelets and has recently been shown to behave like a 5-HTT substrate, as do other anorectic drugs known or suspected to increase the risk of primary PH, such as aminorex, and chlorphentermine (32). The effects of dexfenfluramine on experimental PH have varied across studies, with potentiation of pulmonary vascular remodeling in some studies (30) and reduction (33) or no change (34) in others. The reason why dexfenfluramine may protect against PH under some conditions is unclear but may involve 5-HTT inhibition. In previous studies, we found that discontinuation of prolonged dexfenfluramine treatment was associated with upregulation of 5-HTT and subsequent aggravation of the pulmonary hypertensive process in response to chronic hypoxia (35). It is therefore likely that the effects of drugs interacting with 5-HTT vary according to the type of interaction, intrinsic drug toxicity, and individual patient susceptibility (36).
Our results showing that antidepressant drugs with selective 5-HTT inhibitory properties protect against hypoxia-induced PH may be of clinical relevance, particularly in the light of previous evidence that 5-HTT overexpression is responsible for pulmonary smooth muscle hyperplasia in patients with primary PH (12). Indeed, associations linking 5-HTT overexpression to PH and 5-HTT gene polymorphism to susceptibility to PH may exist in various types of PH. In this study, we found that fluoxetine and citalopram protected against PA-SMC proliferation but also potentiated in vivo pulmonary vasoreactivity. In patients with PH, this suggests that selective 5-HTT inhibitors should be given cautiously or in association with 5-HT receptor antagonists. An important question is whether 5-HTT inhibitors, which are widely used, are harmful or beneficial in patients with PH. According to a preliminary report on a case-control study conducted in Europe in 1996 (37), antidepressant medication use was significantly less common in patients with PPH than in control subjects, suggesting that use of these medications may diminish the risk of PPH development. Clearly, the potential effects of these drugs on PH in humans deserve to be investigated.
Acknowledgment: The authors thank the pharmaceutical companies Eli Lilly, GlaxoSmithKline, Janssen, and Lundbeck for donating the drugs.
References
1. Rubin LJ. Primary pulmonary hypertension. N Engl J Med 1997;336:111-117.
2. Wagenvoort CA, Wagenvoort N. Primary pulmonary hypertension: a pathologic study of the lung vessels in 156 clinically diagnosed cases. Circulation 1970;42:1163-1171.
3. MacLean MR, Herve P, Eddahibi S, Adnot S. 5-hydroxylryptamine and the pulmonary circulation receptors, transporter and relevance to pulmonary arterial hypertension. Br J Pharmacol 2000;131:161-168.
4. Choi DS, Maroteaux L. Immunohistochemical localisation of the serotonin 5-HT2B receptor in mouse gut, cardiovascular system, and brain. PEBS Lett 1996;391:45-51.
5. MacLean MR, Sweeney G, Baird M, McCulloch KM, Houslay M, Morecroft I. 5-Hydroxytryptamine receptors mediating vasoconstriction in pulmonary arteries from control and pulmonary hypertensive rats. Br J Pharmacol 1996;119:917-930.
6. Lee SL, Wang WW, Moore BJ, Fanburg BL. Dual effect of serotonin on growth of bovine pulmonary artery smooth muscle cells in culture. Circ Res 1991;68:1362-1368.
7. Lee SL, Wang WW, Lanzillo JJ, Fanburg BL. Serotonin produces both hyperplasia and hypertrophy of bovine pulmonary artery smooth cells in culture. Am J Physiol 1994;266:L46-L52.
8. Eddahibi S, Fabre V, Boni C, Martres MP, Raffestin B, Hamon M, Adnot S. Induction of serotonin transporter by hypoxia in pulmonary vascular smooth muscle cells-Relationship with the mitogenic action of serotonin. Circ Res 1999;84:329-336.
9. Ramamoorthy S, Bauman AL, Moore KR, Han H, Yang-Feng T, Chang AS, Ganapathy V, Blakely RD. Antidepressant- and cocaine-sensitive human serotonin transporter: molecular cloning, expression, and chromosomal localization. Proc Natl Acad Sci USA 1993;90:2542-2546.
10. Abenhaim L, Moride Y, Brenot F, Rich S, Benichou J, Kurz X, Higenbottam T, Oakley C, Wouters E, Aubier M, et al. Appetite-suppressant drugs and the risk of primary pulmonary hypertension. N Engl J Med 1996;335:609-616.
11. Brenot F, Herve P, Petitpretz P. Primary pulmonary hypertension and the appetite suppressant fenfluramine. Br Heart J 1993;89:117-120.
12. Eddahibi S, Humbert M, Fadel E, Raffestin B, Darmon M, Capron F, Simonneau G, Dartevelle P, Hamon M, Adnot S. Serotonin transporter overexpression is responsible for pulmonary artery smooth muscle hyperplasia in primary pulmonary hypertension. J Clin Invest 2001;108:1141-1150.
13. Eddahibi S, Hanoun N, Lanfumey L, Lesch K, Raffestin B, Hamon M, Adnot S. Attenuated hypoxic pulmonary hypertension in mice lacking the 5-hydroxytryptamine transporter gene. J Clin Invest 2000;105:1555-1562.
14. De Jonghe F, Swinkels J. Selective serotonin reuptake inhibitors: relevance of differences in their pharmacological and clinical profiles. CNS Drugs 1997;7:452-467.
15. Skingle M, Beattie DT, Scopes DT, Starkey SJ, Connor HE, Feniuk W, Tyers MB. GR127935: a potent and selective 5-HT1D receptor antagonist. Behav Brain Res 1996;73:157-161.
16. Barnes NM, Sharp T. A review of central 5-HT receptors and their function. Neuropharmacology 1999;38:1083-1152.
17. Auerbach SB, Hjorth S. Effect of chronic administration of the selective serotonin (5-HT) uptake inhibitor citalopram on extracellular 5-HT and apparent autoreceptor sensitivity in rat forebrain in vivo. Naunyn Schmiedebergs Arch Pharmacol 1995;352:597-606.
18. Gobbi M, Crespi D, Foddi M, Fracasso C, Mancini L, Parotti L, Mennini T. Effects of chronic treatment with fluoxetine and citalopram on 5-HT uptake, 5-HT1B autoreceptors, 5-HT3 and 5-HT4 receptors in rats. Naunyn Schmiedebergs Arch Pharmacol 1997;356:22-28.
19. Yamada J, Sugimoto Y, Yoshikawa T, Horisaka K. Hyperglycemia induced by the 5-HT receptor agonist, 5-methoxytryptamine, in rats: involvement of the peripheral 5-HT2A receptor. Eur J Pharmacol 1997;323:235-240.
20. Gobert A, Rivet JM, Cistarelli L, Millan MJ. Potentiation of the fluoxetine-induced increase in dialysate levels of serotonin (5-HT) in the frontal cortex of freely moving rats by combined blockade of 5-HT1A and 5-HT1B receptors with WAY 100,635 and GR 127,935. J Neurochem 1997;68:1159-1163.
21. Keegan A, Morecroft I, Smillie D, Hicks MN, MacLean MR. Contribution of the 5-HT(1B) receptor to hypoxia-induced pulmonary hypertension: converging evidence using 5-HT(1B)-receptor knockout mice and the 5-HT(1B/1D)-receptor antagonist GR127935. Circ Res 2001;89:1231-1239.
22. Yu AY, Shimoda LA, Iyer NV, Huso DL, Sun X, McWilliams R, Beaty T, Sham JSK, Wiener CM, Semenza GL. Impaired physiological response to chronic hypoxia in mice partially deficient for hypoxia-inducible factor 1[alpha]. J Clin Invest 1999;103:691-696.
23. Demiryurek AT, Wadsworth RM, Kane KA. Pharmacological evidence for the role of mediators in hypoxia-induced vasoconstriction in sheep isolated intrapulmonary artery rings. Eur J Pharmacol 1991;203:1-8.
24. Uzun O, Demiryurek AT, Kanzik I. The role of tyrosine kinase in hypoxic constriction of sheep pulmonary artery rings. Eur J Pharmacol 1998;358:41-47.
25. Eddahibi S, Raffestin B, Pham I, Launay JM, Aegerter P, Sitbon M, Adnot S. Treatment with 5-HT potentiates development of pulmonary hypertension in chronically hypoxic rats. Am J Physiol 1997;272:H1173-H1181.
26. Cutz E, Speirs V, Yeger H, Newman C, Wang D, Perrin DG. Cell biology of pulmonary neuroepithelial bodies-validation of an in vitro model: I: effects of hypoxia and Ca2+ ionophore on serotonin content and exocytosis of dense core vesicles. Anat Rec 1993;236:41-52.
27. Fu XW, Nurse CA, Wong V, Cutz E. Hypoxia-induced secretion of serotonin from intact pulmonary neuroepithelial bodies in neonatal rabbit. J Physiol 2002;539:503-510.
28. Lauweryns JM, de Bock V, Guelinckx P, Decramer M. Effects of unilateral hypoxia on neuroepithelial bodies in rabbit lungs. J Appl Physiol 1983;55:1665-1668.
29. Voelkel NF, Tuder RM. Hypoxia-induced pulmonary vascular remodeling: a model for what human disease? J Clin Invest 2000;106:733-738.
30. Launay JM, Herve P, Peoc'h K, Tournois C, Callebert J, Nebigil CG, Etienne N, Drouet L, Humbert M, Simonneau G, et al. Function of the serotonin 5-hydroxytryptamine 2B receptor in pulmonary hypertension. Nat Med 2002;8:1129-35.
31. Russell BR, Laverty R. Correlation between 5-HT content and uptake site density following (S)-MDMA and dexfenfluramine-induced depletion, and with neuroprotection by the glycine site-specific NMDA antagonist ACEA 1021. Ann N Y Acad Sci 2000:914:208-214.
32. Rothman RB, Ayestas MA, Dersch CM, Baumann MH. Aminorex, fenfluramine, and chlorphenterinine are serotonin transporter substrates. Implications for primary pulmonary hypertension. Circulation 1999;100:869-875.
33. Mitani Y, Mutlu A, Russell JC, Brindley DN, DeAlmeida J, Rabinovitch M. Dexfenfluramine protects against pulmonary hypertension in rats. J Appl Physiol 2002;93:1770-1778.
34. Eddahibi S, Raffestin B, Launay JM, Sitbon M, Adnot S. Effect of dexfenfluramine treatment in rats exposed to acute and chronic hypoxia. Am J Respir Crit Care Med 1998;157:1111-1119.
35. Eddahibi S, Adnot S, Frisdal E, Levame M, Hamon M, Raffestin B. Dexfenfluramine-associated changes in 5-hydroxytryptamine transporter expression and development of hypoxic pulmonary hypertension in rats. J Pharmacol Exp Ther 2001;297:148-154.
36. Eddahibi S, Adnot S. Anorexigen-induced pulmonary hypertension and the serotonin (5-HT) hypothesis: lessons for the future in pathogenesis. Respir Res 2002;3:9-13.
37. Louis WJ. Primary pulmonary hypertension and anorectic drugs. N Engl J Med 1999;340:481-482.
Elisabeth Marcos, Serge Adnot, Minh Hien Pham, Anne Nosjean, Bernadette Raffestin, Michel Hamon, and Saadia Eddahibi
Departement de Physiologie, INSERM U 492, AP-HP, CHU Henri Mondor, Creteil; Departement de Physiologie, Universite Versailles-Saint Quentin en Yvelines, Hopital Ambroise Pare, AP-HP, UFR Paris-lle de France, Ouest, Boulogne; and INSERM U288, NeuroPsychoPharmacologie Moleculaire, Cellulaire et Fonctionnelle, Faculte de Medecine Pitie-Salpetriere, Paris Cedex 13, France
(Received in original form October 23, 2002; accepted in final form May 23, 2003)
Supported by grants from the INSERM, Ministere de la Recherche, Bristol-Myers Squibb Foundation (Unrestricted Biomedical Research Grant), and Fondation de France.
Correspondence and requests for reprints should be addressed to Saadia Eddahibi, INSERM U492, Faculte de Medecine, CHU Henri Mondor, 94010 Creteil, France.
E-mail: saadia.eddahibi@creteil.inserm.fr
Conflict of Interest Statement: E.M. has no declared conflict of interest. S.A. has no declared conflict of interest. M.H.P. has no declared conflict of interest. A.N. has no declared conflict of interest. B.R. has no declared conflict of interest. M.H. has no declared conflict of interest. S.E. has no declared conflict of interest.
Copyright American Thoracic Society Aug 15, 2003
Provided by ProQuest Information and Learning Company. All rights Reserved