I have just returned from the 41st annual meeting of the American Society of Clinical Oncology (ASCO). Twenty-five thousand oncologists converged on Orlando, Florida, to present their latest work and to learn about the progress that has been made over the past year in treating various types of cancer. There were nearly 10,000 abstracts presented at this meeting, as well as numerous commercial displays in the vast and towering exhibition hall. Some of these were masterpieces of advertising design, although not necessarily of hard science.
[ILLUSTRATION OMITTED]
The first thing that strikes me is the dramatic shift over the last dozen years from a chemotherapy-based model of cancer treatment to the new paradigm based around molecularly 'targeted' therapies. Such a change should in fact be welcomed by people who are sympathetic to complementary and alternative medicine (CAM). The great philosophical debate over the excess toxicity of standard chemotherapy has been won by those favoring a "kinder, gentler" approach to cancer treatment. Indeed, almost every speech and most of the poster sessions featured targeted drugs of one description or another.
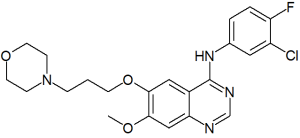
At the same time, I find little in the actual practice of targeted therapy to kindle much enthusiasm. In this, I am at odds with most leaders of oncology. For instance, in his 2005 Karnofsky Memorial Lecture (the highest honor given by ASCO), Charles L. Sawyers, MD, of the University of California at Los Angeles (UCLA), spoke for many of his colleagues when he said that the age of molecularly targeted cancer therapy had unquestionably arrived. As he saw it, the fact that so many presentations focused on the use of so-called tyrosine kinase inhibitors such as imatinib (Gleevec), gefitinib (Iressa) and erlotinib (Tarceva) validated the basic concepts of targeted therapy.
Since it has been seven years since the Food and Drug Administration (FDA) approved Herceptin (trastuzumab), one of the very first targeted drugs, to treat breast cancer, and four years since it approved Gleevec for chronic myelogenous leukemia (CML), one could certainly expect to see some definitive proof of the targeted treatment philosophy. But while such agents have undoubtedly scored some successes over the years--Gleevec in particular is a very worthwhile agent--the field as a whole has run into many unanticipated obstacles as it tries to tackle the common tumors of adults.
In particular, it has turned out that these agents have more side effects than was predicted initially by advocates of molecular targeting. For example, take the surprisingly widespread occurrence of potentially fatal bleeding episodes with the drug Avastin (bevacizumab). According to the manufacturer's own website: "Serious, and in some cases fatal, hemoptysis [the coughing of blood from the lungs, ed.] has occurred in patients with non-small cell lung cancer treated with chemotherapy and Avastin. In a small study, the incidence of serious or fatal hemoptysis was 31% in patients with squamous histology and 4% in patients with adenocarcinoma receiving Avastin as compared to no cases in patients treated with chemotherapy alone. Patients with recent hemoptysis should not receive Avastin."
In addition, when given as stand-alone treatments, most of these agents have demonstrated surprisingly poor results in various clinical trials. As was seen recently with the phase III clinical trials of Iressa, they sometimes do not actually extend overall survival at all. In April, 2005, the US National Cancer Institute (NCI) decided to discontinue all further clinical trials with Iressa, once a front-runner in the targeted therapy movement. "Iressa Clinical Trials Squashed Like a Nasty Cigarette Butt," is how one former pharmaceutical developer (Stacey Lloyd) graphically summed up NCI's action.
Plenary Session Disappointments
At the ASCO plenary session held on Saturday afternoon (May 14, 2005), there was a discussion of three different combinations of chemotherapy with targeted drugs, in this case antiangiogenic agents. Such agents are designed to stop the formation of new blood vessels that can promote the growth of tumors. This session illustrated the complex obstacles that researchers in this field have encountered. Two of the speakers reported that the targeted drug bevacizumab (Avastin) provided what they called a significant survival advantage in patients with metastatic colorectal cancer and advanced non-small cell lung cancer, respectively. However, a third study, using the up-and-coming antiangiogenic drug PTK/ZK, failed to show that this drug significantly improved progression-free survival when given in combination with chemotherapy as a first-line treatment for advanced colorectal cancer.
At first sight, you might think that two positive trials out of three is not bad. However, what the survival numbers actually show is something quite different. Thus, when Avastin was given alone to patients with metastatic colorectal cancer, their median overall survival was just 10.2 months. A standard chemo regimen of 5-FU, leucovorin and oxaliplatin, called FOLFOX 4, yielded a very similar 10.8 months. Only when the two treatments were administered together did survival rise to 12.9 months. Thus there was a gain of two months through the use of this intensive--and expensive--regimen. How much of this increased survival time was spent by patients feeling sick because of toxicity remains to be discovered.
NOTE: The median is the middle number in a set of ordered data. Thus, the median of the numbers 1,1,1,2,4,6,6 is 2 since 2 is the middle number when all of the numbers are placed in order. In statistics, the median is considered a more reliable measure than the mean, which is more commonly what is meant by the word "average."
Another figure that oncologists frequently look at is median progression-free survival (PFS). This refers to the time that elapses between administration of the treatment and the time that progression of the disease is detected in a living patient. Here the figures were even less encouraging. With Avastin alone, this period of remission was just 2.7 months. With FOLFOX 4 alone it was 4.8 months. When the two were given together it was 7.2 months. At that point, the cancer was detected to be once again on the march. So, again, we're talking about a gain of a few months.
In the second reported trial, the standard regimen FOLFOX 4 was given with PTK/ZK, a new orally administered, targeted antiangiogenic agent. The effects of this combination were then compared to FOLFOX 4 given with a placebo pill. No figures on median overall survival will be available until 2006. But the combination that included PTK/ZK yielded an average (median) progression-free survival of 7.7 months. This was nearly identical to the 7.6 months experienced by the FOLFOX 4 group. It seems therefore that in this group of patients, the new drug had no effect on the progression of their cancer.
In a third trial, a standard regimen of two drugs, paclitaxel and carboplatin (PC), was compared to PC + bevacizumab (Avastin) in the treatment of metastatic non-small cell lung cancer. The median overall survival here was 10.2 months for PC alone vs. 12.5 months when Avastin was added. The median progression free survival was 4.5 months for PC alone vs. 6.4 months for the combination. These studies support the idea that Avastin (at least in clinical trials) adds around two months to disease free and to overall survival when it is added to standard chemotherapy for some advanced solid tumors of adults.
Gemzar + Tarceva
A similar picture emerged from an eagerly awaited Canadian clinical trial of the standard drug gemcitabine (Gemzar) with and without the targeted agent erlotinib (Tarceva) for advanced pancreatic cancer. The trial in question began in October 2001 and ran for several years. It was a large study, with a total of 569 pancreatic cancer patients from 140 centers in 17 countries. This study was considered so important that it was listed as Abstract #1 out of over 9,700 abstracts presented at the 2005 ASCO meeting. It was further highlighted at the first plenary session.
Tarceva is one of several drugs that are directed against the so-called epidermal growth factor receptor (EGFR), a common target for these ingenious new agents. EGFR is commonly over-expressed in pancreatic cancer and so, by all calculations, should have worked against this cancer.
Despite this promising theoretical basis, Tarceva in actual practice had little effect on survival in these difficult-to-treat patients. The median overall survival for patients in the Gemzar + Tarceva group was 6.37 months. This compared to 5.91 months for Gemzar + placebo. Thus the net benefit of giving Tarceva was only two weeks extra survival.
Progression-free survival was 3.75 months for Gemzar + Tarceva compared to just 3.55 months for the Gemzar + placebo. Thus Tarceva added about one week of remission-free survival for these patients.
Yet, amazingly, some doctors at the meeting argued that this was an important and exciting finding. They pointed out that the benefit was statistically significant, or not due to chance. (The possibility of establishing statistical significance was increased by the relatively large number of patients included in this trial.) Malcolm Moore, MD, the lead investigator at Princess Margaret Hospital, Toronto, hailed the study as the first evidence of what he called the "benefits of EGFR tyrosine kinase inhibitors in combination with chemotherapy" (ASCO Daily News, May 16, 2005).
When these same data were presented at an ASCO seminar in January, 2005, the manufacturer, Roche, claimed that the "breakthrough drug Tarceva provides new hope for patients with advanced pancreatic cancer." For me, such comments have a Through-the-Looking-Glass feel. After all, we're talking about one or two WEEKS of life extension.
Oftentimes, these unrealistic statements go unchallenged at ASCO, where a rah-rah atmosphere surrounds the latest products drummed up by Big Pharma. But this time the official discussant, James L. Abbruzzese, MD, of the celebrated M.D. Anderson Cancer Center, Houston, Texas, challenged the principal observation of the study. "I do not feel that the results clearly alter the standard of care for patients with advanced pancreatic cancer," he told the audience. In my opinion this was a diplomatic way of saying that despite the imprimatur of "statistical significance," Tarceva didn't really do anything of importance for such patients.
There was also a public disagreement over the toxicity of the combined treatment. Dr. Moore claimed the combined treatment caused "only modest increases in toxicity and minimal effect on quality of life," although no details concerning toxicity were provided in the abstract. Dr. Abbruzzese, however, stated that the modest gains in survival had to be balanced against the increased toxicity.
The results so far with targeted therapies for solid tumors of adults, with or without standard chemo, are, to my mind, underwhelming. These drugs are nothing like the blockbusters that have been heralded by the mainstream media and that once garnered front-page coverage in Time magazine and elsewhere. Although these drugs may lead to remissions in some individuals, given alone, they hardly do anything to extend life in carefully designed clinical trials; given in combination with chemotherapy a few of them add a month or two at best, to the survival of carefully chosen patients with selected kinds of cancer.
These patented drugs are collectively driving a rapid inflation in the cost of cancer care. According to the Los Angeles Times, for instance, the targeted drugs Avastin and Herceptin cost nearly $8,000 a month. The economic burden of this new generation of targeted drugs is staggering. By 2006, global spending on cancer drugs is predicted to total $31.7 billion, up from $22.3 billion in 2004, according to the consulting firm of Bain & Co. That makes cancer the fastest growing drug category (Gellene 2005).
As an example, in colorectal cancer, until recently, the standard treatment was 5-FU, or fluorouracil, administered with a vitamin-like substance called leucovorin. This treatment cost a lifetime total of around $500 per patient. But now patients with inoperable colon cancer are being treated with a combination of newer chemotherapy drugs (such as the FOLFOX 4 regimen) as well as targeted therapies, including Avastin and Erbitux.
According to Dr. Leonard Saltz of Memorial Sloan-Kettering Cancer Center, the average life expectancy of patients has doubled to 22 months. But the cost of treatment has not just doubled but increased 500 times to $250,000 per patient. There are approximately 105,000 new cases of colorectal cancer in the US each year, and over 56,000 deaths. No wonder these targeted drugs are now earning billions of dollars for their manufacturers. But the indisputable fact is that the cost of these targeted therapies has increased so dramatically that they run the risk of bankrupting health insurance plans, not to mention the cancer patients among the 45 million Americans who lack insurance entirely. For them, and for society as a whole, the rising cost of cancer therapy can be a tragedy in its own right.
Sources:
Gellene, Denise. New cancer drugs are driving up cost of care. Los Angeles Times, May 14, 2005.
Genentech statement on Avastin: http://www.gene.com/gene/products/information/oncology/avastin/index.jsp
Stacey Lloyd website: http://lungdiseases.about.com/mbiopage.htm
Roche statement on Tarceva: http://www.roche.com/inv-update-2005-01-28b
by Ralph W. Moss, PhD, Director, The Moss Reports
[c]2004 Ralph W. Moss, PhD. All Rights Reserved
800-980-1234 * www.cancerdecisions.com
COPYRIGHT 2005 The Townsend Letter Group
COPYRIGHT 2005 Gale Group