Rationale: The role of monocytes in acute endotoxemia has been ascribed to systemic release of mediators within the central circulation. Little is known about the potential role of "marginated" monocytes in regulating microvascular inflammatory signaling.
Objectives: To investigate whether lung-marginated monocytes can locally activate pulmonary endothelial cells through cell contact-dependent interactions in early endotoxemia.
Methods: Mice were challenged with LPS to produce acute endotoxemia and pulmonary vascular injury. Adoptive transfer of ex vivo LPS-stimulated donor leukocytes to recipient mice was also performed to evaluate cell-associated inflammatory signaling between monocytes and endothelial cells within the lung. Cell suspensions from excised lungs were analyzed by flow cytometry for expression of tumor necrosis factor α (TNF-α) on monocytes and cell adhesion molecules on endothelial cells.
Results: Substantial numbers of monocytes rapidly marginated to the lungs after endotoxin challenge in mice, and lung-marginated monocytes expressed significantly higher levels of membrane TNF than circulating monocytes, due to higher TNF production by the marginated cells. Injection of activated wild-type donor leukocytes to wild-type or TNF receptor double knockout recipients demonstrated that lung-marginated monocytes can induce TNF-dependent upregulation of adhesion molecules on pulmonary endothelial cells. Injection of activated donor leukocytes from TNF knock-in mice that express uncleavable mutant membrane TNF also induced adhesion molecule upregulation in wild-type recipients without a systemic soluble TNF release.
Conclusions: These results reveal a previously unacknowledged role for lung-marginated monocytes in early endotoxemia, exerting local, cell-associated TNF signaling within the pulmonary microcirculation, contributing to the evolution of pulmonary vascular injury.
Keywords: endothelial cells; endotoxin shock; lipopolysaccharide; lung; macrophages
Septic shock is an important cause of mortality in hospitalized patients (1, 2), associated with activation of cells and mediators of the innate immune system and dysfunction of various body organs, including the lung. Monocytes, a multipotential blood cell population of the mononuclear phagocyte system (MPS), actively respond to inflammatory stimuli in vitro by releasing mediators such as the cytokine tumor necrosis factor α (TNF-α). However, the in vivo role of monocytes in endotoxin shock has not been well defined, in particular during the early phase, a period of intense inflammatory signaling long before the chronic mononuclear infiltration in the later stages of sepsis-associated organ injury (3-5). It is generally assumed that circulating monocytes contribute to the increased plasma levels of cytokines during endotoxemia, but the major portion of plasma TNF response to LPS has been shown to originate from tissue macrophages, particularly liver Kupffer cells (6, 7). Hence, monocytes may not be major contributors to systemic release of cytokines and generalized activation of immune and endothelial cells in endotoxemia (8).
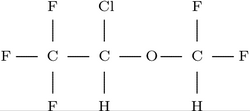
Blood monocytes, due to their adhesive interactions with endothelial cells before extravasation, are distributed approximately equally between the central circulation (circulating pool) and the microvasculature (marginated pool) (9-12). It is well established that monocytes actively migrate into tissue at sites of endothelial injury and locally regulate chronic inflammation (e.g., atherosclerosis) (13). However, the potential role of "marginated" monocytes within the intravascular space in modulating microvascular inflammatory signaling during acute endotoxemia has not been defined. TNF is a critical mediator in experimental models of endotoxin shock as well as human meningococcal septicemia (14, 15). TNF is first expressed as a membrane-bound protein (memTNF) and then its extracellular domain is cleaved by TNF-α-converting enzyme (TACE) to produce a soluble cytokine (solTNF) (16, 17). There is growing evidence that memTNF is bioactive in cell-to-cell interactions (18-21), and that solTNF also signals in a paracrine fashion to adjacent cells unless an excessive amount is produced that spills over into the central circulation (22). For such cell-associated, highly localized TNF signaling, circulating monocytes are not candidates because of their continuous movement. In contrast, marginated monocytes, in close, direct contact with endothelial cells, may exert such cell-associated microvascular TNF signaling via memTNF and/or locally released solTNF.
We hypothesized that marginated monocytes, as opposed to circulating monocytes, play a crucial role in early endotoxemia, locally activating microvascular endothelial cells through direct cell-to-cell interactions, particularly within the pulmonary circulation, contributing to the progression of acute lung injury. Using an LPS-induced model of endotoxin shock and associated pulmonary vascular injury in mice (23), we found that substantial numbers of monocytes rapidly marginated to the lungs after LPS challenge where they express memTNF and solTNF at significantly higher levels than circulating monocytes. In vivo adoptive leukocyte transfer experiments using wild-type (WT) as well as TNF-mutant and TNF-receptor double knockout (DKO) mice indicated that marginated monocytes are capable of activating endothelial cells within the pulmonary microcirculation, upregulating cell adhesion molecules (CAMs) via local, cell-contact, and TNF-dependent mechanisms. Some of the results of these studies have been previously reported in the form of abstracts (24-26).
METHODS
Animals
All protocols were reviewed and approved by the U.K. Home Office, in accordance with the Animals (Scientific Procedures) Act 1986, United Kingdom. Experiments were performed using male C57BL6 mice (Charles River, Margate, UK) aged 8 to 12 wk, age-matched TNF-receptor DKO mice (p55^sup -/-^p75^sup -/-^) backcrossed onto its WT C57BL6 strain for five generations (Amgen, Thousand Oaks, CA) (27, 28), or aged-matched TNF knock-in (KI) mice (memTNF^sup [white triangle up]/[white triangle up]^), which were rendered deficient in cleavage of memTNF by the replacement of TACE-sensitive TNF amino acid sequence (background C57BL6; DNAX, Palo Alto, CA) (29).
Endotoxin-induced Pulmonary Vascular Injury in Mice
Mice received an intravenous (via tail vein) or intraperitoneal injection of 0.02 to 200 µg of LPS (Escherichia coli O111:B4; Sigma, Poole, UK). We have previously shown that an LPS injection of 20 µg or more produced progressive circulatory failure and pulmonary vascular injury in C57BL6 mice over several hours (23). At 15 to 120 min after LPS injection, mice were heparinized intravenously and killed by isoflurane overdose. Blood was obtained by cardiac puncture, and their lungs were excised with care taken to avoid the hilum connective tissues.
Donor-recipient Model of Pulmonary Vascular Inflammation in Mice
Leukocyte-enriched suspensions, prepared from donor mouse blood by dextran separation followed by ammonium chloride-induced red blood cell lysis, were incubated with 0.1 µg LPS for 10 min at 37°C and then placed on ice. After washing four times (200 × g at 4°C for 5 min) to remove LPS, cells were resuspended in saline and viable cells counted using Trypan blue. Cells were then injected intravenously into recipient mice, which were killed after 4 h and the lungs excised. In some experiments, after exposure to LPS, cells were labeled with 2.5 µM 5-(and 6-)carboxyfluorescein-diacetate-succinimidyl-ester (CFSE) (Molecular Probes, Leiden, The Netherlands) for 5 min at room temperature (30), washed, and then injected into recipients.
Preparation of Lung Cell Suspension
Lung cell suspensions were prepared from the excised lungs either by mechanical disruption, as described previously (23, 31), or by mechanical disruption plus collagenase treatment. For quantitation and characterization of lung monocytes, finely minced lung tissue was homogenized on a 70-µm nylon mesh sieve (BD Falcon, Oxford, UK) with a syringe plunger. In some animals, lung lavage was performed, before excising the lungs, with 750 µl of saline as described previously (28, 32). For determination of in situ memTNF levels on lung monocytes, minced lung tissues were homogenized, and then immediately placed on ice, and 10 µM BB94 (British Biotech, Abingdon, UK), a hydroxamate-based TACE inhibitor, was added to minimize changes in memTNF levels during analysis. Blood was also treated in a similar fashion to the lung samples (i.e., at room temperature during mincing of the lungs, cooled, and BB94 added) to compare memTNF levels between lung and blood monocytes. For extraction of endothelial cells and measurement of CAM expression, minced lung tissue was incubated in collagenase type IV (Sigma) at 1 mg/ml for 15 min at 37°C and homogenized. Cell suspensions were flushed through sieves, resuspended in ice-cold fluorescence-activated cell sorter medium (phosphate-buffered saline with 2% fetal calf serum, 0.1% sodium azide, and 5 mM ethylenediaminetetraacetic acid).
Ex Vivo Determination of TNF Production by Lung and Blood Cells
Mice were killed 30 min after 20 µg intraperitoneal LPS injection, and lung cell suspensions prepared by mechanical disruption with the addition of CO2-independent medium (Invitrogen, Paisley, UK) plus 10% fetal calf serum, and blood diluted 1 in 10 in the same medium. Cells were incubated in a 37°C water bath for 30 min with or without 10 µM of BB94. Levels of memTNF were determined by flow cytometry, and in situ TNF production estimated by memTNF at 30 min with BB94 minus memTNF at 0 min, and TNF cleavage estimated by memTNF at 30 min with BB94 minus memTNF at 30 min without BB94.
Flow Cytometric Analysis
Cells were stained in the dark at 4°C for 30 min with fluorophore-conjugated antimouse antibodies for TNF (clone MP6-XT22), CD11b (M1/70), CD34 (RAM34), platelet-endothelial CAM (PECAM)-1 (MEC13.3), vascular CAM (VCAM)-1 (429), E-selectin (10E9.6; BD Pharmingen, Oxford, UK), F4/80 (Serotec, Oxford, UK), or appropriate isotype-matched control antibodies. In experiments involving blood, red blood cell lysis and fixation were performed using fluorescence-activated cell sorter-lyse solution (BD Pharmingen). Samples were acquired (a minimum of 1,000 gated monocytes were acquired per sample) and analyzed using a FACSCalibur flow cytometer and Cell Quest software (BD Pharmingen). Absolute cell counts in samples were determined using microspheres beads (Catlag Medsystems, Towcester, UK), as previously described (31).
SolTNF Measurement
Levels of solTNF were measured by ELISA (R&D Systems, Minneapolis, MN). Levels of bioactive solTNF were determined by the WEHI 164 cytotoxicity assay as previously described (32, 33), using a recombinant TNF protein (410-MT; R&D Systems) as the standard.
Statistical Analysis
Data are expressed as mean ± SD. Statistical comparisons were made by t tests or analysis of variance with Scheffé's tests. Statistical significance was defined as p
RESULTS
MemTNF Expression on Circulating Monocytes after LPS Challenge
To define the timing of the monocyte TNF response relative to the systemic release of TNF into the circulation, we measured solTNF levels in plasma and memTNF expression on circulating monocytes in LPS-challenged mice (Figures 1A and 1B). After intravenous LPS challenge (200 µg), plasma solTNF peaked at 60 min, whereas memTNF expression was detected on blood monocytes (identified by CD11b and F4/80 expression) at 30 min and maintained until 60 min. Quantification of blood monocytes indicated that LPS challenge produced a rapid and severe monocytopenia (Figure 1C), which preceded or coincided with memTNF expression on circulating monocytes.
Flow Cytometric Analysis of memTNF Expression on Lung-marginated Monocytes
To quantify monocyte margination to the lung and evaluate their in situ activation in mice, we developed a flow cytometry-based method by modifying our previous method of detecting neutrophil sequestration in the whole lung of mice (31). Lung cell suspensions were prepared from the excised lungs of mice injected intravenously with saline or LPS, by mechanical disruption without enzymatic digestion. Monocytes were differentiated from alveolar macrophages, which are negative for CD11b with high forward/side scatter and substantial autofluorescence, and from neutrophils, which are negative for F4/80 with high side scatter (Figure 2A). Monocytes in lung and blood samples displayed identical phenotypes by flow cytometry (not shown), indicating that our extraction method did not substantially influence the surface marker expression of lung cells. We found that lung monocytes showed a large increase at 45 min after LPS injection (6.98 ± 2.49 × 10^sup 5^/mouse) compared with saline-challenged control animals (3.17 ± 0.81 × 10^sup 5^/mouse, n = 4/group, p
Lung-marginated Monocytes Express More TNF than Circulating Monocytes
We then compared the levels of memTNF and solTNF expression by the lung-marginated and circulating monocytes in response to LPS. LPS (0.02-200 µg) was administered to mice via the intraperitoneal rather than intravenous route to avoid any abrupt exposure of the lung cells to undiluted LPS. We confirmed that intraperitoneal injection of LPS (45 min after 20 µg injection; n = 4) produced a similar increase in lung monocyte number (7.37 ± 1.18 × 10^sup 5^/ mouse) and a similar degree of monocytopenia (4.95 ± 0.93 × 10^sup 4^/ml) to those observed with intravenous injection. At 45 min after intraperitoneal LPS challenge, lung-marginated monocytes expressed significantly more memTNF per cell than circulating monocytes (Figure 3A) at all the LPS doses (p
To estimate in situ TNF production and processing by these lung-marginated and circulating monocytes, samples were harvested 30 min after LPS challenge (when memTNF was first detected on the monocyte surface), and then incubated ex vivo for a further 30 min, with or without a saturating dose of BB94, which produced greater than 95% inhibition of TNF cleavage. TNF production by these cells was assessed by accumulation of memTNF during the incubation with BB94, and TACE-mediated TNF cleavage was assessed by the difference between memTNF levels at the end of incubation with and without BB94 (Figure 3B). Both indices were much higher in lung than in blood monocytes (p
Flow Cytometric Detection of In Vivo CAM Upregulation on Pulmonary Endothelial Cells
To evaluate the degree of pulmonary microvascular inflammation in mice in vivo, we further modified the above flow cytometric method for detection of in vivo CAM upregulation on pulmonary endothelial cells. Pulmonary endothelial cells were identified in collagenase-digested lung cell suspensions as high PECAM-1 expressing cells (34, 35), which were also uniformly positive for CD34, consistent with the microvascular origin of these cells (Figure 4) (35). Mice injected intravenously with high doses of LPS (200 µg) or recombinant TNF (1 µg) displayed substantial upregulation of VCAM-1 and E-selectin expression on high PECAM-1-positive cells at 4 h after challenge. Thus, the method provides a sensitive technique to detect in vivo upregulation of VCAM-1 and E-seleclin on pulmonary endothelial cells, as previously shown by immunohistology in response to intravenous TNF challenge (36).
Monocytes Upregulate CAMs on Pulmonary Endothelial Cells via Cell-associated TNF Signaling
To investigate the effects of "local" cell-associated TNF signaling exerted by the lung-marginated monocytes, independent from the effects of "systemic" TNF signaling exerted by the circulating solTNF derived from the whole body MPS, we developed a donor-recipient model of pulmonary microvascular inflammation. Activated donor leukocytes were injected intravenously into a recipient mouse, where they were expected to produce cell-associated signaling in the lung microvasculature, with minimal involvement of the systemic proinflammatory response. In vitro incubations of donor leukocytes, with BB94 to enhance the memTNF signal, indicated that only monocytes produced TNF (Figure 5A), for a period up to 60 min after stimulation.
Using this model, we investigated the ability of activated donor monocytes to upregulate CAM expression on pulmonary endothelial cells in recipient mice. TNF dependency of such cell-associated signaling was evaluated using TNF receptor DKO mice (p55^sup -/-^p75^sup -/-^) as recipients. In WT recipients receiving 5 × 10^sup 6^ activated donor leukocytes (3.41 ± 0.47 × 10^sup 5^ donor monocytes), we found significant increases in VCAM-1 and E-selectin expression on pulmonary endothelial cells at 4 h after injection (Figure 5B). When untreated WT donor leukocytes were injected into WT recipients, no change in CAM expression was observed. CAM upregulation was substantially attenuated in DKO recipients (p
To assess the possible contribution of whole body circulating solTNF in this model, plasma levels of bioactive solTNF were measured in WT recipients. A time point of 1 h after donor leukocyte injection was chosen, which on the basis of in vivo LPS challenge data represents the time at which plasma solTNF would peak. The WEHI bioassay indicated bioactive solTNF levels of 224 ± 91 pg/ml (n = 4), using a recombinant TNF (R&D Systems) as the standard. In a separate group of WT mice, the same recombinant TNF was injected intravenously, the lungs were analyzed by flow cytometry after 3.5 h, and an in vivo dose-response curve relating the dose of TNF and the levels of CAM upregulation on pulmonary endothelial cells was constructed (Figure 6). On this curve, extrapolation of the mean fluorescent intensity values of CAM expression obtained in the donor-recipient experiments (~ 40 for VCAM-1 and ~ 4 for E-selectin) corresponds to a dose of 40 to 50 ng of recombinant TNF. This implies that a greater than 100-fold higher plasma solTNF concentration than was actually detected would be required to induce the observed levels of CAM upregulation, assuming approximately 2 ml of circulating blood volume for mice.
Monocytes Activate Pulmonary Endothelial Cells via memTNF Signaling
To further separate the effects of contact-dependent "memTNF" signaling by the lung-marginated monocytes from the effects of solTNF locally released by these monocytes within the microvasculature, we used donor cells from mutant TNF KI mice (memTNF^sup [white triangle up]/[white triangle up]^). Previous characterization of these mice indicated that levels of solTNF released in response to LPS were undetectable, whereas levels of memTNF expression were slightly lower than those in WT mice (29). Injection of 5 to 10 × 10^sup 6^ activated KI donor leukocytes (4.89 ± 1.58 × 10^sup 5^ donor monocytes) into WT recipients produced significant increases, albeit lower than those observed with WT donor leukocytes, in both VCAM-1 and E-selectin expression on pulmonary endothelial cells at 4 h after injection (Figure 7). However, levels of solTNF in plasma at 1 h after injection were undetectable by both WEHI assay (detection limit, ~ 0.5 pg/ml) and ELISA (detection limit, ~ 1 pg/ml). Thus, in the absence of a solTNF response, signaling by monocytes was reduced but still sufficient to induce endothelial activation, suggesting the presence of cell contact-dependent memTNF signaling by marginated monocytes in the pulmonary microcirculation.
To confirm the contact-dependent TNF signaling capacity of activated mouse monocytes, we developed an in vitro bioassay system based on coculture of live mouse leukocytes with endothelial cells, and found that leukocytes from WT as well as TNF KI mice induced endothelial CAM upregulation that was largely TNF-dependent, consistent with the above in vivo findings (see online supplement for the results of these additional experiments).
DISCUSSION
The present study demonstrated that monocytes were rapidly sequestered by the pulmonary circulation in response to acute endotoxemia, where they produced TNF-mediated CAM upregulation on pulmonary endothelial cells. A considerable number of additional monocytes (> 3.5 × 10^sup 5^ cells) marginated to the lung, accounting for more than 50% of estimated total circulating monocyte number (6.2 × 10^sup 5^ cells) for mice (9). Although there is some evidence in the literature suggesting a large LPS-induced shift of monocytes from circulating to marginated pools (37-39), in particular to the lung (40), the biological role of lung-marginated monocytes in the pathophysiology of acute endotoxemia has not been addressed. Using a method to quantitate in situ TNF expression by monocytes and CAM expression by endothelial cells in the lung and a technique of adoptive leukocyte transfer, we provide the first in vivo evidence of a previously unacknowledged "local" (by marginated monocytes), as opposed to "systemic" (by circulating monocytes), role of monocytes in acute endotoxemia and associated pulmonary vascular injury. The results suggest that lung-marginated monocytes, through direct and early activation of endothelial cells, may have a pivotal role in orchestrating inflammatory signaling within the pulmonary microvasculature during endotoxemia.
The contribution of blood monocyles to lung inflammation in endotoxemia has mainly been ascribed to a late period (24-48 h) after endotoxin challenge. Previous studies reported that accumulation of monocytes/macrophages within the lung was not evident until 24 h after LPS challenge in mice (5, 41). However, these studies performed perfusion of pulmonary vessels before the harvest of lung tissues, focusing mainly on migrating monocytes/macrophages in the intraalveolar and interstitial compartments. There was no evidence for monocyte extravasation for up to 6 h after LPS challenge, but the design of the experiments excluded analyses of any role of adherent intravascular monocytes before extravasation. Using a flow cytometry-based approach that enables access to cells in all lung compartments, including the intravascular space (see Figure 2A), we found that considerable numbers of monocytes, relative to the total circulating pool, were already present in the lungs of normal mice, which were then substantially increased within 1 h after LPS challenge. This large and very rapid increase in lung monocyte number after LPS challenge, without any evidence of intraalveolar migration, suggests localization of these monocytes within the pulmonary microvasculature. Our findings are consistent with the previous study by Doherty and colleagues (40) in which LPS induced an immediate and sustained margination of ex vivo radiolabeled monocytes in the lungs of recipient rabbits. The mechanism of monocyte-preferential margination to the lung has been attributed to the unique anatomic structure of the pulmonary microvascular bed (40). Monocytes as well as neutrophils must deform to pass through the narrow pulmonary capillary segments, and LPS produces physical stiffening of leukocytes by actin polymerization, leading to enhanced physical entrapment by the capillaries (42-44). Continued retention of monocytes in the pulmonary circulation has been shown to involve CD18-dependent adhesion (40).
We found that these monocytes marginated to the lung in response to LPS expressed much higher levels of memTNF and solTNF than the circulating monocytes. Ex vivo incubations with BB94 indicated an enhanced TNF production without impairment of memTNF cleavage (i.e., increased memTNF expression as well as solTNF release; see Figure 3B). Because there is evidence that TNF production by monocytes can be enhanced by interactions with endothelial cells in vitro (45), it is likely that a similar augmentation of monocyte activation occurs in vivo, leading to a more intense inflammatory signaling within the pulmonary microvasculature than in the central circulation. This discrepancy in activation status between lung-marginated and circulating monocytes is in agreement with the recently emerging concept of the paradoxic immunologic response during sepsis; that is, fluids and cells derived from local inflamed tissues are proinflammatory or hyperreactive to ex vivo stimuli, whereas plasma and circulating blood cells are often antiinflammatory or hyporeactive (46, 47).
Using the donor-recipient model of pulmonary microvascular inflammation, we addressed two key questions: (1) to what extent are marginated monocytes, independent of the systemic MPS response, capable of inducing activation of pulmonary endothelial cells, and (2) how much of the endothelial response is mediated by local cell adhesion-associated TNF signaling. CAM upregulation, a crucial in vivo pathophysiologic step for neutrophil sequestration and organ injury in endotoxemia, was used as a marker of pulmonary microvascular inflammation and injury (48-51). The donor leukocyte suspensions underwent extensive washing-that is, each wash diluting any contaminant at least 20- to 30-fold and repeated four times-which should result in a more than 10^sup 5^-fold reduction of the original LPS dose (0.1 µg) used for ex vivo stimulation. Because our flow cytometry method cannot detect any CAM upregulation with intravenous LPS doses of less than 0.02 µg, the observed CAM upregulation in recipient mice could not be explained by the effects of trace amounts of LPS in the injected cell suspensions. Despite the relatively small number of activated donor monocytes marginated to recipient lungs (~ 1 × 10^sup 5^ cells, assuming 30% margination of injected donor monocytes to the lung), as compared with the endogenous monocyte number present after LPS injection (6-7 × 10^sup 5^ cells), the results provided clear evidence that injection of WT donor leukocytes produced TNF-mediated CAM upregulation, using WT as well as TNF-receptor DKO mice as recipients (see Figure 5). Monocytes were the only cell population to produce TNF among the injected donor leukocytes, and therefore the observed effects should be ascribed to monocytemediated effects.
It is theoretically possible that the CAM upregulation observed in recipient mice could be due to circulating solTNF, produced either by the injected donor monocytes per se (marginated to the lung as well as other organ beds) or by the body MPS in response to cell transfusion. However, this possibility was effectively excluded because bioactive solTNF levels in recipient plasma induced by injection of WT donor leukocytes were considerably lower than the concentrations required to produce the observed CAM upregulation, as shown in Figure 6. Furthermore, injection of TNF KI (memTNF^sup Δ/Δ^) donor cells, which express only the TACE-uncleavable mutant memTNF molecules, produced small but significant CAM upregulation without evidence of systemic TNF release. Therefore, our results demonstrated that cell adhesion-dependent TNF signaling by lung-marginated monocytes can exert a significant physiologic impact on pulmonary microvascular inflammation. Comparison of CAM induction by WT and TNF KI donor cells revealed that lung-marginated monocytes contribute to pulmonary endothelial cell activation by a combination of both solTNF and memTNF signaling. It should be noted that expression of memTNF in KI mice is slightly reduced as compared with WT mice (29), and this may be an additional reason for the lower levels of CAM upregulation induced by KI monocytes. The relative contribution of each form of TNF will presumably vary according to the rate of TNF production and levels of TACE activity, which is known to alter under inflammatory conditions (52).
The present study used the well-characterized high-dose LPS bolus model of acute endotoxemia (5, 23, 40, 41, 53). It is well known that the magnitude of systemic cytokine response in this model is exaggerated as compared with human sepsis or peritonitis model of sepsis in animals (54, 55), and hence direct extrapolation of the results of the LPS bolus model to clinical sepsis and septic shock requires some caution. However, our findings would raise the possibility that local monocyte-mediated inflammation may play a significant role in pulmonary microvascular injury during sepsis. Consistent with this hypothesis, Hadjiminas and coworkers (56) reported that high and prolonged levels of TNF mRNA were localized to lung tissue in the absence of significant plasma TNF in the mouse cecal ligation and puncture model. Because plasma endotoxin is most likely responsible for stimulation of TNF production in these experiments, the data suggest the role of marginated intravascular monocytes as a potential source of TNF-mediated signaling in the lung in chronic models of sepsis.
Certain animal species, such as sheep and pigs, possess unique resident MPS cells within the pulmonary microvasculature, known as "pulmonary intravascular macrophages" (57). These macrophages, adhered to pulmonary endothelia, respond vigorously to infection by phagocytosis and release of mediators, including TNF (58), and hence have been considered to play an important role in pathogenesis of endotoxemia-associated acute lung injury in these species (59). Our findings suggest that in both rodents and humans, which do not have pulmonary intravascuiar macrophages, lung-marginated monocytes may potentially play a similar role to these specialized resident macrophages, regulating a critical early intravascular event in the lung with acute systemic inflammatory stimuli.
In summary, the present study provides direct in vivo evidence of "marginated" monocyte function in the lung in response to LPS, producing cell-associated, TNF-mediated activation of pulmonary microvascular endothelial cells. As compared with the conventional concept of systemic solTNF release initiating multiorgan propagation of the septic inflammatory response, the highly localized solTNF as well as memTNF signaling by lung-marginated monocytes may be an additional, or even the dominant, activating pathway, in the evolution of pulmonary microvascular injury during acute endotoxemia and potentially in the early phase of sepsis.
Conflict of Interest Statement: None of the authors have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
Acknowledgment: The authors thank Dr. J. D. Sedgwick for his invaluable advice on analysis of TNF KI mice and Mr. M. E. Coddard for his technical assistance.
References
1. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003;348: 1546-1554.
2. Riedemann NC, Guo RF, Ward PA. The enigma of sepsis. J Clin Invest 2003;112:460-467.
3. Doherty DE, Downey GP, Worthen GS, Haslett C, Henson PM. Monocyte retention and migration in pulmonary inflammation: requirement for neutrophils. Lab Invest 1988;59:200-213.
4. Ohgami M, Doerschuk CM, Gie RP, English D, Hogg JC. Late effects of endotoxin on the accumulation and function of monocytes in rabbit lungs. Am Rev Respir Dis 1992;146:190-195.
5. Standiford TJ, Kunkel SL, Lukacs NW, Greenbcrger MJ, Danforth JM, Kunkel RG, Stricter RM. Macrophage inflammatory protein-1 alpha mediates lung leukocyte recruitment, lung capillary leak, and early mortality in murine endotoxemia. J Immunol 1995;155:1515-1524.
6. Fong YM, Marano MA, Moldawer LL, Wei H, Calvano SE, Kenney JS, Allison AC, Cerarai A, Shires GT, Lowry SF. The acute splanchnic and peripheral tissue metabolic response to endotoxin in humans. J Clin Invest 1990;85:1896-1904.
7. Luster MI, Germolec DR, Yoshida T, Kayama F, Thompson M. Endotoxin-induced cytokine gene expression and excretion in the liver. Hepatology 1994;19:480-488.
8. Munoz C, Misset B, Fitting C, Bleriot JP, Carlet J, Cavaillon JM. Dissociation between plasma and monocyte-associated cytokines during sepsis. Eur J Immunol 1991;21:2177-2184.
9. van Furth R, Sluiter W. Distribution of blood monocytes between a marginating and a circulating pool. J Exp Med 1986;163:474-479.
10. Ohgami M, Doerschuk CM, Gie RP, English D, Hogg JC. Monocyte kinetics in rabbits. J Appl Physiol 1991;70:152-157.
11. Klonz A, Wonigeit K, Pabst R, Westermann J. The marginal blood pool of the rat contains not only granulocytes, but also lymphocytes, NK-cells and monocytes: a second intravascular compartment, its cellular composition, adhesion molecule expression and interaction with the peripheral blood pool. Scand J Immunol 1996;44:461-469.
12. Imhof BA, Aurrand-Lions M. Adhesion mechanisms regulating the migration of monocytes. Nat Rev Immunol 2004;4:432-444.
13. Linton MF, Fazio S. Macrophages, inflammation, and atherosclerosis. Int J Obes Relat Metab Disord 2003;27:S35-S40.
14. Waage A, Halstensen A, Espevik T. Association between tumour necrosis factor in serum and fatal outcome in patients with meningococcal disease. Lancet 1987;1:355-357.
15. van Deuren M, van der Ven-Jongekrijg J, Bartelink AK, van Dalen R, Sauerwein RW, van der Meer JW. Correlation between proinflammatory cytokines and antiinflammatory mediators and the severity of disease in meningococcal infections. J Infect Dis 1995;172:433-439.
16. Black RA, Rauch CT, Kozlosky CJ, Peschon JJ, Slack JL, Wolfson MF, Castner BJ, Stocking KL, Reddy P, Srinivasan S, et al. A metalloproteinase disintegrin that releases tumour-necrosis factor-alpha from cells. Nature 1997;385:729-733.
17. Werb Z, Yan Y. A cellular striptease act. Science 1998;282:1279-1280.
18. Mohler KM, Sleath PR, Fitzner JN, Cerretti DP, Alderson M, Kerwar SS, Torrance DS, Otten-Evans C, Greenstreet T, Weerawarna K, et al. Protection against a lethal dose of endotoxin by an inhibitor of tumour necrosis factor processing. Nature 1994;370:218-220.
19. Eissner G, Kohlhuber F, Grell M, Ueffing M, Scheurich P, Hieke A, Multhoff G, Bornkamm GW, Holler E. Critical involvement of transmembrane tumor necrosis factor-alpha in endothelial programmed cell death mediated by ionizing radiation and bacterial endotoxin. Blood 1995;86:4184-4193.
20. Pellegrini JD, Puyana JC, Lapchak PH, Kodys K, Miller-Graziano CL. A membrane TNF-alpha/TNFR ratio correlates to MODS score and mortality. Shock 1996;6:389-396.
21. Alexopoulou L, Pasparakis M, Kollias G. A murine transmembrane tumor necrosis factor (TNF) transgene induces arthritis by cooperative p55/p75 TNF receptor signaling. Eur J Immunol 1997;27:2588-2592.
22. Cavaillon JM, Munoz C, Fitting C, Missel B, Carlet J. Circulating cytokines: the tip of the iceberg? Circ Shock 1992;38:145-152.
23. Ghosh S, Wilson MR, Choudhury S, Yamamoto H, Goddard ME, Falusi B, Marczin N, Takata M. Effects of inhaled carbon monoxide on acute lung injury in mice. Am J Physiol Lung Cell Mol Physiol 2005;288: L1003-L1009.
24. O'Dea KP, Goddard ME, Robotham JL, Brennan FM, Takata M. Early expression of membrane TNF on lung-sequestered monocytes in a murine model of sepsis [abstract]. Am J Respir Crit Care Med 2003; 167:A553.
25. O'Dea KP, Wilson MR, Robotham JL, Brennan FM, Takata M. TNF-dependent activation of pulmonary endothelial cells by lung-sequestered monocytes in a mouse model of sepsis [abstract]. Am J Respir Crit Care Med 2004;169:A636.
26. Young AJ, O'Dea KP, Yamamoto H, Takata M. Monocytes expressing transmembrane TNF upregulate endothelial cell adhesion molecules [abstract]. Immunology 2003;110:86.
27. Peschon JJ, Torrance DS, Stocking KL, Glaccum MB, Otten C, Willis CR, Charrier K, Morrissey PJ, Ware CB, Mohler KM. TNF receptor-deficient mice reveal divergent roles for p55 and p75 in several models of inflammation. J Immunol 1998;160:943-952.
28. Wilson MR, Choudhury S, Takata M. Pulmonary inflammation induced by high-stretch ventilation is mediated by tumor necrosis factor signaling in mice. Am J Physiol Lung Cell Mol Physiol 2005;288:L599-L607.
29. Ruuls SR, Hoek RM, Ngo VN, McNeil T, Lucian LA, Janatpour MJ, Korner H, Scheerens H, Hessel EM, Cyster JG, et al. Membrane-bound TNF supports secondary lymphoid organ structure but is subservient to secreted TNF in driving autoimmune inflammation. Immunity 2001;15:533-543.
30. Weston SA, Parish CR. New fluorescent dyes for lymphocyte migration studies: analysis by flow cytometry and fluorescence microscopy. J Immunol Methods 1990;133:87-97.
31. Choudhury S, Wilson MR, Goddard ME, O'Dea KP, Takata M. Mechanisms of early pulmonary neutrophil sequestration in ventilator-induced lung injury in mice. Am J Physiol Lung Cell Mol Physiol 2004;287:L902-L910.
32. Wilson MR, Choudhury S, Goddard ME, O'Dea KP, Nicholson AG, Takata M. High tidal volume upregulates intrapulmonary cytokines in an in vivo mouse model of ventilator-induced lung injury. J Appl Physiol 2003;95:1385-1393.
33. Espevik T, Nissen-Meyer J. A highly sensitive cell line, WEHI 164 clone 13, for measuring cytotoxic factor/tumor necrosis factor from human monocytes. J Immunol Methods 1986;95:99-105.
34. Eppihimer MJ, Russell J, Langley R, Vallien G, Anderson DC, Granger DN. Differential expression of platelet-endothelial cell adhesion molecule-1 (PECAM-1) in murine tissues. Microcirculation 1998;5:179-188.
35. Muller AM, Hermanns MI, Skrzynski C, Nesslinger M, Muller KM, Kirkpatrick CJ. Expression of the endothelial markers PECAM-1, vWf, and CD34 in vivo and in vitro. Exp Mol Pathol 2002;72:221-229.
36. Neumann B, Machleidt T, Lifka A, Pfeffer K, Vestweber D, Mak TW, Holzmann B, Kronke M. Crucial role of 55-kilodalton TNF receptor in TNF-induced adhesion molecule expression and leukocyte organ infiltration. J Immunol 1996;156:1587-1593.
37. Kane MA, May JE, Frank MM. Interactions of the classical and alternate complement pathway with endotoxin lipopolysaccharide: effect on platelets and blood coagulation. J Clin Invest 1973;52:370-376.
38. Mackensen A, Galanos C, Wehr U, Engelhardt R. Endotoxin tolerance: regulation of cytokine production and cellular changes in response to endotoxin application in cancer patients. Eur Cytokine Netw 1992;3: 571-579.
39. Fijen JW, Kobold AC, de Boer P, Jones CR, van der Werf TS, Tervaert JW, Zijlstra JG, Tulleken JE. Leukocyte activation and cytokine production during experimental human endotoxemia. Eur J Intern Med 2000;11:89-95.
40. Doherty DE, Downey GP, Schwab B III, Elson E, Worthen GS. Lipolysaccharide-induced monocyte retention in the lung. Role of monocyte stiffness, actin assembly, and CD18-dependent adherence. J Immunol 1994;153:241-255.
41. VanOtteren GM, Strieter RM, Kunkel SL, Paine R III, Greenberger MJ, Danforth JM, Burdick MD, Standiford TJ. Compartmentalized expression of RANTES in a murine model of endotoxemia. J Immunol 1995;154:1900-1908.
42. Worthen GS, Schwab IIIB, Elson EL, Downey GP. Mechanics of stimulated neutrophils: cell stiffening induces retention in capillaries. Science 1989;245:183-186.
43. Wagner JG, Roth RA. Neutrophil migration mechanisms, with an emphasis on the pulmonary vasculature. Pharmacol Rev 2000;52:349-374.
44. Doerschuk CM. Mechanisms of leukocyte sequestration in inflamed lungs. Microcirculation 2001;8:71-88.
45. Fan ST, Edgington TS. Integrin regulation of leukocyte inflammatory functions: CDllb/CD18 enhancement of the tumor necrosis factor-alpha responses of monocytes. J Immunol 1993;150:2972-2980.
46. Munford RS, Pugin J. Normal responses to injury prevent systemic inflammation and can be immunosuppressive. Am J Respir Crit Care Med 2001;163:316-321.
47. Cavaillon JM, Adib-Conquy M, Cloez-Tayarani I, Fitting C. Immunodepression in sepsis and SIRS assessed by ex vivo cytokine production is not a generalized phenomenon: a review. J Endotoxin Res 2001;7: 85-93.
48. Xu H, Gonzalo JA, St Pierre Y, Williams IR, Kupper TS, Cotran RS, Springer TA, Gutierrez-Ramos JC. Leukocytosis and resistance to septic shock in intercellular adhesion molecule 1 -deficient mice. J Exp Med 1994;180:95-109.
49. Ridings PC, Windsor AC, Jutila MA, Blocher CR, Fisher BJ, Sholley MM, Sugerman HJ, Fowler AA III. A dual-binding antibody to E- and L-selectin attenuates sepsis-induced lung injury. Am J Respir Crit Care Med 1995;152:247-253.
50. Lo SK, Bevilacqua B, Malik AB. E-selectin ligands mediate tumor necrosis factor-induced neutrophil sequestration and pulmonary edema in guinea pig lungs. Circ Res 1994;75:955-960.
51. Nolte D, Kuebler WM, Muller WA, Wolff KD, Messmer K. Attenuation of leukocyte sequestration by selective blockade of PECAM-1 or VCAM-1 in murine endotoxemia. Eur Surg Res 2004;36:331-337.
52. Black RA. Tumor necrosis factor-alpha converting enzyme. Int J Biochem Cell Biol 2002;34:1-5.
53. Blackwell TS, Lancaster LH, Blackwell TR, Venkatakrishnan A, Christman JW. Chemotactic gradients predict neutrophilic alveolitis in endotoxin-treated rats. Am J Respir Crit Care Med 1999;159:1644-1652.
54. Cross AS, Opal SM, Sadoff JC, Gemski P. Choice of bacteria in animal models of sepsis. Infect Immun 1993;61:2741-2747.
55. Parker SJ, Watkins PE. Experimental models of gram-negative sepsis. Br J Surg 2001;88:22-30.
56. Hadjiminas DJ, McMasters KM, Peyton JC, Cheadle WG. Tissue tumor necrosis factor mRNA expression following cecal ligation and puncture or intraperitoneal injection of endotoxin. J Surg Res 1994;56:549-555.
57. Warner AE. Pulmonary intravascular macrophages: role in acute lung injury. Clin Chest Med 1996;17:125-135.
58. Cirelli RA, Carey LA, Fisher JK, Rosolia DL, Elsasser TH, Caperna TJ, Gee MH, Albertine KH. Endotoxin infusion in anesthetized sheep is associated with intrapulmonary sequestration of leukocytes that immunohistochemically express tumor necrosis factor-alpha. J Leukoc Biol 1995;57:820-826.
59. Warner AE, DeCamp MM Jr, Molina RM, Brain JD. Pulmonary removal of circulating endotoxin results in acute lung injury in sheep. Lab Invest 1988;59:219-230.
Kieran P. O'Dea, Arnold J. Young, Hirotoshi Yamamoto, James L. Robotham, Fionula M. Brennan, and Masao Takata
Department of Anesthetics and Intensive Care, and Kennedy Institute of Rheumatology Division, Faculty of Medicine, Imperial College London, London, United Kingdom; and Department of Anesthesiology, University of Rochester Medical Center, Rochester, New York
(Received in original form April 19, 2005; accepted in final form August 2, 2005)
Supported by grants from the Wellcome Trust (No. 057459) and the Medical Research Council UK (No. G0000101). Tumor necrosis factor (TNF) receptor double knockout mice were a gift from Amgen (Thousand Oaks, CA), and TNF knock-in mutant mice were a gift from DNAX (Palo Alto, CA).
Correspondence and requests for reprints should be addressed to Dr. Masao Takata, M.D., Ph.D., Department of Anaesthetics and Intensive Care, Imperial College London, Chelsea and Westminster Hospital, 369 Fulham Road, London SW10 9NH, UK. E-mail: m.takata@imperial.ac.uk
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Am J Respir Crit Care Med Vol 172. pp 1119-1127, 2005
Originally Published in Press as DOI: 10.1164/rccm.200504-605OC on August 4, 2005
Internet address: www.atsjournals.org
Copyright American Thoracic Society Nov 1, 2005
Provided by ProQuest Information and Learning Company. All rights Reserved