Effectiveness of modified release isosorbide mononitrate affected by incorrect use
James D Hider, Zaid Shehab, R Courteney-Harris, Ear, Nose, and Throat Department, City General Hospital, Newcastle under Lyme, Staffordshire
We report a case of ischaemic chest pain in a patient after the mode of administration of the antianginal drug isosorbide mononitrate was altered.
A 78 year old man had an aggressive and inoperable pharyngeal tumour. Radiotherapy had failed to control the tumour, and he had worsening dysphagia. The patient had several medical conditions, including ischaemic heart disease. He could swallow only fluids and tablets and not solids. On admission, feeding commenced through a nasogastric tube. This was well tolerated at first, but over a period of weeks he removed the tube several times owing to discomfort. Reinserting the tube became clinically more difficult, and it was decided to feed him through a percutaneous endogastric tube.
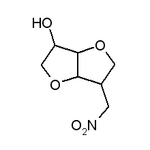
While being fed by the nasogastric tube and subsequently the percutaneous endogastric tube the patient regularly complained of upper epigastric pain and nausea, usually in the late afternoon and evening. This was thought to be a complication of feeding. The pain lessened when he used glyceryl trinitrate sublingual spray, which he had been using without the staff's knowledge. Electrocardiography during one of these episodes showed ischaemic changes in V3-6 leads (figure).
[Figure ILLUSTRATION OMITTED]
His drug chart was reviewed. He was receiving diuretics and modified release isosorbide mononitrate, which until recently had controlled his angina well. Diuretics and antibiotics were being given in liquid form through the feeding tube but as modified release isosorbide mononitrate is available only in tablet form the tablets were being crushed in water before being given through the percutaneous endogastric tube. Pharmacy confirmed that the sustained release effect of the nitrate would be lost if the coating was destroyed.
The drug regimen was altered to short acting nitrate three times daily. The angina resolved, and the patient no longer required the nitrate spray as an inpatient.
The manufacturer of isosorbide mononitrate stresses that the tablet should not be crushed, although the Medicines Control Agency have had no reports of a lack of effect or complications through this action.
Clopidogrel associated with acute arthritis
Anu Garg, Johannes Radvan, Neil Hopkinson, Department of Cardiology, Royal Bournemouth Hospital, Bournemouth, Dorset BH8 8DH
Clopidogrel is a new ADP receptor antagonist used in the prevention of myocardial infarction, stroke, and vascular death. We report two cases of acute arthritis and tendonitis after clopidogrel use.
Case 1
A 76 year old woman was referred with a six year history of angina pectoris. She was stabilised on treatment but began to develop further symptoms at rest two months before referral. She had a long history of hypertension. She took atenolol 100 mg once daily, diltiazem 90 mg twice daily, isosorbide mononitrate 20 mg twice daily, and aspirin 75 mg daily.
Significant two vessel coronary artery disease was found at cardiac catheterisation. She underwent percutaneous transluminal coronary angioplasty and stent insertion of the right coronary artery. She was prescribed diltiazem 120 mg twice daily, clopidogrel 75 mg once daily, and aspirin 150 mg once daily.
Two weeks later she developed widespread pruritus, with no obvious rash, and intense pain and swelling of the metacarpophalangeal joints. The joints were red and hot, and there was synovitis. Other joints were unaffected. Her erythrocyte sedimentation rate and C reactive protein concentration were increased to 86 mm in the first hour and 81 mg/l respectively. Uric acid concentration was normal and x ray films showed soft tissue swelling only with no chondrocalcinosis. Clopidogrel was stopped.
One week later the pruritus had settled and the joint pain had improved. Repeat testing of inflammatory markers confirmed the improvement.
Case 2
A 63 year old man was referred with three episodes of chest discomfort on exertion. He was an ex-smoker and had a six year history of mild type 2 diabetes mellitus. In 1984 he had an uncomplicated subarachhoid haemorrhage. He took lisinopril 20 mg once daily and long acting diltiazem 200 mg once daily.
Severe coronary artery disease in a left dominant system was found at cardiac catheterisation. He underwent coronary artery bypass grafting. He was allergic to aspirin so was prescribed clopidogrel 75 mg once daily in addition to lisinopril.
Three weeks later he presented to his doctor with severe pain of his right knee. The knee was tender, and he was unable to bear weight on the leg. There was tenderness, heat, and swelling over the quadriceps tendon proximal to the patella. His erythrocyte sedimentation rate was mildly increased to 47 mm in the first hour. His serum urate concentration was normal. Clopidogrel was discontinued, and the symptoms resolved.
To our knowledge arthritis has not been described as a side effect of clopidogrel, and the manufacturer knows of only one case. The two cases we describe had acute musculoskeletal inflammation and increased concentrations of inflammatory markers. We recommend that clopidogrel be considered as a potential cause of arthritis.
COPYRIGHT 2000 British Medical Association
COPYRIGHT 2000 Gale Group