Why are swallowing examinations important for persons who have developmental disabilities?
Between 39% and 56% of persons with disabilities have some difficulty in feeding (Denhoff, 1981; Love, Hagerman, & Taimi, 1980; Palmer, Thompson, & Linscheid, 1975; Thomas, Bax, & Jenkins, 1989). Many of these problems are associated with the swallowing process, the passage of substances through the pharynx and to the esophagus. Such problems are particularly prevalent in persons who have cerebral palsy, the most common cause of congenital neurogenic dysphagia (Christensen, 1989).
In persons who have severe neurodevelopmental disorders, a significant amount of impairment in swallowing and in the coordination of the processes of alimentation and ventilation may occur. The complex system of reflexes that coordinates the two functions may be disrupted to varying degrees in children with congenital neurogenic dysphagia. The resulting incoordination of the two functions can result in its mildest form in difficult swallowing or, in more severe cases, in recurrent and potentially life-threatening aspiration pneumonia.
Although swallowing difficulties are often recognized when coughing or choking occurs consistently during feeding, aspiration due to abnormal closure of the airways during swallowing may not necessarily lead to these responses. The more difficult-to-detect aspiration, called "silent" aspiration, may be particularly problematic. In their study of children undergoing videofluoroscopic swallow studies at the Children's Hospital of Buffalo, Arvedson, Rogers, Buck, Smart, and Msall (1992) found that of the 186 children they studied, 26% aspirated; of those aspirating, 94% showed no coughing or other obvious signs of aspiration.
For individuals who have severe developmental disabilities, as for other individuals, an instrumental swallowing exam would be indicated for diagnostic or treatment planning purposes when clinical examination suggests dysphagia and (a) the individual's nutritional or pulmonary status appears compromised or (b) the patient's complaints or symptoms are inconsistent with the findings of the clinical exam. An instrumental examination might also be indicated when clinical examination suggests dysphagia and (a) the patient has a medical diagnosis or condition associated with risk of dysphagia (e.g., craniofacial abnormalities, neurologic, pulmonary, or gastrointestinal disease), or (b) the patient is fully dependent' for feeding or oral care.
What is fiberoptic endoscopy and what are its advantages over other techniques for observing and evaluating swallowing?
As a supplement or alternative to videofluoroscopic modified barium swallow, and performed in conjunction with a careful clinical examination, fiberoptic endoscopy can serve as a valuable tool for evaluating dysphagia and for the detection of aspiration (Bastian, 1993; Langmore, Schatz, & Olson, 1991; Perie et al., 1998). At a cost of roughly half that of videofluoroscopy (Aviv et al., 1998), a fiberoptic endoscopic examination of swallowing can be performed by a speech-language pathologist (ASHA, 1995). In the procedure, a fiberoptic laryngoscope is typically passed transnasally to view the pharynx during the swallowing of foods of various consistencies. The procedure allows direct observation via video monitor, as well as videorecording, of pharyngeal activity, including bolus flow through the hypopharynx, movement of structures in reaction to or anticipation of the bolus, residue material within the hypopharynx or larynx, and other indices important to examination of the swallowing process. Of particular benefit is the ability to directly visualize aspiration before or after the swallow.
In our work, we have found that occasionally individuals with developmental disabilities who have had no difficulties identified in recent videofluoroscopic studies have had aspiration observed and documented via endoscopy.
Among 10 patients we have seen who had recently had videofluoroscopy, aspiration was documented by both videofluoroscopy and fiberoptic examination in six cases, detected by fiberoptic examination but not by videofluoroscopy in three cases, and by neither procedure in one case. In each of the cases in which aspiration was detected by fiberoptic examination, consensus was obtained from a second examiner, a pulmonary physician.
For the three individuals for whom aspiration was detected by fiberoptic examination but not by videofluoroscopy, it is likely that the videofluoroscopic studies did not provide a sufficient time sample for the detection of aspiration. If it were possible to lengthen the videofluoroscopic studies with this population. we might find that the videofluoroscopic studies would indeed detect the aspiration. However, the difficulties in maintaining the cooperation and appropriate positioning of persons who have developmental disabilities, as well as concerns about radiation exposure, create a particular problem in conducting lengthy videofluoroscopic examinations.
The ability to extend the fiberoptic examination over the course of a full meal holds particular benefit because (a) it becomes possible to observe swallowing as the structures associated with swallowing begin to fatigue, and (b) it is possible to observe the effects of postural change over time on swallowing. We have observed that over time we can intervene therapeutically to improve posture and, in turn, improve swallowing.
Unlike videofluoroscopy, fiberoptic endoscopy poses no risks of radiation exposure. Because of this advantage, repeated examinations as a means of monitoring the effects of interventions, as well as more lengthy examinations to view the effects of fatigue, are more feasible with endoscopy than with videofluoroscopy.
The relatively unrestrictive nature of the fiberoptic examination, allowing assessment of swallowing during positioning changes or other interventions, is a particularly valuable aspect of the procedure. Although videofluoroscopic studies have suggested that positioning might play a role in both oral and pharyngeal swallowing function (Larnert & Ekberg, 1995), researchers and clinicians have at times been hampered by the positioning demands of videofluoroscopic examination for persons with severe neuromuscular disease, sometimes requiring that the individual ingest the test substance while strapped to, and rotated in, a specially designed positioning chair (Cox & Petty, 1991). The fiberoptic examination, on the other hand, poses little restriction on seating or position and can typically be done in the individual"s wheelchair or other regular seating. For persons with severe physical disabilities due to cerebral palsy or other neurodevelopmental disorder, this flexibility in positioning is quite advantageous both for ease of administration and for conducting the examination in a sitting posture that is natural for the individual. As described above, the flexibility in positioning also provides the examiner with the opportunity to view swallows under different seating and postural conditions to test the effectiveness of treatment interventions involving posture or positioning.
One shortcoming of the fiberoptic examination is the lack of information it provides regarding the oral-motor stage of feeding (e.g., chewing, transfer of bolus). In order to fully understand any individual's feeding problems, whether results from developmental disability or not, it is important to examine the oral-motor and swallowing stages in tandem. Given the oral control problems faced by persons who have cerebral palsy and other neuromuscular disorders, it is of particular importance to conduct a careful clinical examination, possibly including videofluoroscopy as an adjunct.
Are there issues that require particular attention or special accommodations to be made when performing fiberoptic endoscopic examinations of swallowing with patients who have developmental disabilities?
The full benefits of the endoscopy can be realized only if the assessment situation is managed in a manner that takes into account the cognitive capacities, emotional needs, and, for some, spasticity and/or hypersensitivity of persons with these disabilities. A general protocol outlining the clinical aspects of the fiberoptic examination has been published (Langmore & McCulloch, 1997), but strategies for incorporating the clinical procedures into the broader assessment situation for persons with developmental disabilities have not been described.
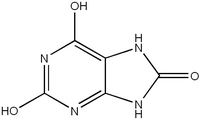
In the following sections, we present a few relatively simple steps that can be taken to maximize the effectiveness of the process and usefulness of the results. These recommendations are based on our experience in conducting 30 fiberoptic examination attempts with 27 patients (three individuals were studied twice) who have developmental disabilities. Although most of these patients had cerebral palsy, three patients had Lesch-Nyhan disease (a rare disorder involving an inborn error of purine metabolism), and others had Down syndrome, muscular dystrophy, or spina bifida. A broad range of ages, from 5 to 47, was included in our sample.
In conducting the examinations, we found that we were unable to begin the procedure on two of our patients, both with Down syndrome, due to agitation apparently associated with oral hypersensitivity. In three other patients, we found the need to limit the examination due to patient discomfort.
What are some of the areas in which special attention or accommodations might be helpful? In preparation for the fiberoptic examination, considerable attention must be paid to addressing the concerns and apprehensions of the individual and, if appropriate, of his or her parents or guardians. The typical parent of a child who has a developmental disability or other chronic neuromotor condition has witnessed his or her child undergo countless diagnostic, surgical, and treatment procedures. For such a parent, there is an appropriate tendency to discount procedures that he or she perceives to be uncomfortable and/or to be of limited benefit.
If the child has had no prior history of dysphagia, and without an understanding of the examination procedure, the thought of introducing an instrument via the child's nasal passages might indeed be regarded by the parent or guardian as unnecessarily intrusive. Without exception, the parents or guardians of our students for whom the fiberoptic examination was recommended spontaneously voiced concerns to the child's physician or speechlanguage pathologist about the possibility of discomfort during the introduction of the endoscope. Others expressed concern that the procedure would not yield worthwhile results because the presence of the endoscope would likely prevent their child from swallowing.
A process of educating the parent about dysphagia and its short and long-term effects in persons who have neurodevelopmental disorders is often sufficient to impress on the parents the value of the examination. Further, a discussion of the endoscopy as an alternative or adjunct to videofluoroscopy is necessary to ensure a full understanding of the available diagnostic options. We have found that providing opportunity for parents to view videotapes of endoscopic examinations done on persons other than their child provides them with a clearer picture of both the process and of the potential benefits of the procedure. Cast models of the nasal passages and of the larynx have also been helpful in explaining the route of the endoscope's introduction.
A similar process of education must occur for the individual who is to be examined as well. Among persons with developmental disabilities who have cognitive impairment, their ability to understand the purpose or process of the examination may be limited. Care must be taken to ensure their understanding of the process to whatever level is possible.
For those children or adults who have sufficient cognitive capacity, an educational process similar to that given to the parents or guardians might be provided. For younger children or those who have moderate or severe cognitive impairment, however, a thorough educational process might not be possible. Rather, a process of familiarizing the individual with the surroundings and the persons involved will be helpful in reducing his or her anxiety, and consequently in maximizing his or her cooperation. Exposing the individual to the room (and to the examiner if he or she is unfamiliar) in the hours or days preceding the examination is helpful in this regard.
Beyond educating the individual and his/her parents or guardians, it is often helpful to devise ways in which the child or young adult can exercise some control over aspects of the examination. The idea that a person's motivation and sense of well-being are mediated in part by the degree to which he or she feels a sense of control over the environment is supported by a vast body of psychological literature, particularly that stemming from the work of Seligman and his collaborators (Klein & Seligman, 1976; Miller & Seligman, 1975). We have found that allowing the individual some part in selecting the foods to be used, the color of the gown or protective cover, or any other aspect of the environment lends a sense of control over the process and, consequently, greater comfort.
How might the examination environment be modified to accommodate persons with developmental disabilities?
A room that is familiar to the individual should be used if possible, and as few staffpersons or observers as possible should be present. In our work, we have restricted, whenever possible, the staffpersons in the room to the speech-language pathologist or physician who is conducting the examination and a nurse to provide assistance to the examiner and reassurance to the child or young adult. Aside from these two individuals, we have found it useful in reducing anxiety for a parent or trusted staffperson to be present, and for younger children or those with severe cognitive deficits or special emotional needs to be seated in a parent's or caregiver@ s lap during the examination. It should be noted, however, that when seating the child in a manner other than that in which he or she normally feeds, the benefit of an examination that maximally reflects the child's regular swallowing function may be compromised.
For individuals for whom involuntary spastic movements of the arms make the examination difficult, an assistant may need to be available to ensure that gross movements don't reach the endoscope. Spasticity resulting in head movement can typically be controlled with the use of a collar designed for head positioning.
During the insertion of the endoscope, the distraction of a cartoon or other children's video might be helpful for younger children or those with more severe cognitive impairment. Other individuals, particularly young adults or adults with little or no cognitive impairment, might prefer the option of viewing the endoscopy itself via a monitor. The examiners at our facility have expressed that the ability to view the monitor seems to calm the patients. Even this simple provision may lend the individual an enhanced sense of participation in the process and, consequently, increased feelings of control. Of the students we have tested, roughly two-thirds have viewed the video monitor during the examination. Indeed, several of our students who are young adults have asked without prompting if they could view the monitors. None of the individuals who have watched the monitors have found the images to be disturbing or distressing. Staffpersons conducting the examinations have noted that when students watched the monitors, their apparent increase in comfort allowed longer examinations that produced more complete and clearer results.
Although watching either an entertaining video or the swallowing images might, for some persons, continue to be a helpful distraction throughout the examination, it might in some cases affect the exam negatively by distracting the person from the task of swallowing, thus increasing the chance of aspiration. The question also exists whether viewing the images of the swallow might provide feedback to the patient and change the swallow, thus rendering the results of lesser value for diagnostic purposes. Although these issues have not been investigated, they might prompt one to question whether the examination should be conducted with as little distraction as possible, or perhaps with levels of distraction roughly equivalent to those in the individual's normal eating environment.
If parents or guardians are present, they might be invited to watch the images on the monitor to get a real-time view of the swallowing process while hearing the examiner's initial description of the findings as the examination progresses. Three of the parents/guardians of our students who have been examined viewed the procedure via the video monitor and reported to find the video images, when carefully explained by the examiner, to be helpful in clarifying the swallowing difficulties their children were experiencing. In presenting a rationale for the use of endoscopy in the diagnosis of speech and language disorders, Kamell (1994) commented on the educational value of having the person examined and other interested individuals review video images following the procedure, and suggests that the video motivates individuals to follow through on treatment recommendations. How long does the exam take?
The length of the examination is, to a large extent, a function of the examiner's ability to maintain the individual's cooperation. The lengths of our examinations averaged 21 minutes (10-30 minutes). This amount of time generally allows an examination of the pooling of oral secretions, vocalization, the presentation of solids and liquids, and examination of the clearing process. For those individuals for whom cooperation and attention cannot be maintained for this length of time, a more focused examination targeted toward specific issues of concern can be conducted in 10 to 13 minutes. This brief exam would focus on examination of the structural condition of the pharynx and hypopharynx and on gauging the adequacy of the pharyngeal stage of swallow. It is sometimes possible at the outset of the examination to determine persons for whom the abbreviated exam will be necessary. As noted above, of 28 examinations conducted at our facility, only 3 needed to be limited in this way.
How can the individual's comfort be maintained?
Topical anesthesia to the nasal mucosa has been used by others in attempts to minimize discomfort of the introduction of the endoscope (Bastian, 1991, 1993; Ohmae, Logemann, Kaiser, Hanson, & Kahrilas, 1995; Williams, Farquharson, & Anthony, 1975). We, however, have found the introduction of the endoscope to be well tolerated and the administration of anesthesia unnecessary. A recent study supports our observation that anesthesia is generally not necessary, confirming that there is little added comfort with the use of topical anesthesia (Leder, Ross, Briskin, & Sasaki, 1997).
Neurological impairment may cause individuals who have developmental disabilities to over -respond to sensory information, as was most apparent in our two patients who have Down syndrome. These two patients showed significant agitation at the touch of the examiner. Often, such persons find a light touch to be more stimulating than a firmer touch. Therefore, when helping the individual to maintain head stability or when providing a reassuring touch to the shoulder, a firm touch might be preferable to a lighter one (Fraser, Hensinger, & Phelps, 1990). For others who are hypersensitive, the use of a Hensinger head support, a soft foam "wraparound" collar that may be attached by mount to a chair or wheelchair, can be a helpful means of providing stability without the need to provide headholding that might be disturbing to some. Hensinger supports are often used by persons with neurodevelopmental disorders to maintain a midline position during feeding.
With the increased agitation and lack of understanding of the examination process that are experienced by persons with developmental disabilities, it is particularly important with these persons to provide continuous verbal reassurance throughout the examination process. Status reports and praise help to calm and relax the individual.
What can be done after the exam to maximize its usefulness?
Ideally, the endoscopic examination is conducted with video and/or still photograph documentation. Although the child or young adult might have had opportunity to view the endoscope monitor throughout the examination. the ability to review a videotape of the examination while participating in a more in-depth discussion of the findings is extremely helpful for those who have sufficient cognitive capacity. The educational value of reviewing the videotape with the individual was clearly demonstrated when one young adult for whom pharyngeal paralysis was detected remarked, "Look at that! Why am I not coughing?" as he watched videotape of food substances entering his trachea. Research to more clearly define the educational value of reviewing the videotape with the individual, particularly with regard to promoting compliance with recommendations, would be beneficial.
Among the parents and guardians of our students, almost all viewed videotapes at some point after the evaluation. For one parent, the videotape was instrumental in facilitating the difficult decision to have her child undergo a gastrostomy. The videotape also allows opportunity to consult with other clinicians or physicians in arriving at clinical decisions, and it documents a baseline level of swallowing function for use in comparisons with future endoscopic findings.
Following endoscopic examinations, parents frequently express appreciation for having been involved in the process, and they express a better understanding of their child's particular difficulties. With regard to the individual's level of comfort and appreciation of the process, we find that our children and young adults who have had endoscopic examinations of swallowing are quite willing to undergo the procedure again if necessary. Three of our students, in fact, have made unsolicited requests to undergo the procedure again.
What are the risks associated with fiberoptic examination of swallowing with this population? Possible adverse events that have been associated with fiberoptic endoscopic examination of the swallowing process include mucosal perforation and bleeding, laryngospasm, and allergic reaction to topical anesthetics (ASHA, 1995), although no such adverse events occurred with our sample. Research has not addressed whether or not persons with developmental disabilities are at greater risk of adverse events during or resulting from the fiberoptic examination than are others. One might expect, however, that persons who have spasticity and/ or hyperreflexivity might be at increased risk of accidental perforation of the mucosal tissue due to sudden movement. As noted above, the use of a head support might be helpful in maintaining proper head position, thus minimizing risk of such an injury.
What conclusions can be drawn regarding the management of the fiberoptic examination environment when working with persons who have developmental disabilities?
We believe that with the use of fiberoptic endoscopic examination of swallowing with children or young adults who have developmental disabilities, certain accommodations when managing the examination process can maximize the likelihood of obtaining useful findings. Sensitive and thorough preparation of both the individual with suspected dysphagia and his or her parents or guardians, as well as management of the examination environment in a way that allows the individual's participation, reduces anxiety, increases cooperation, and promotes more effective implementation of interventions that might be recommended.
References
American Speech-Language-Hearing Association. (1995). ASHA desk reference, Vol. III: Speechlanguage pathology. Rockville, MD: Author.
Arvedson, J., Rogers, B., Buck, G., Smart, P., & Msall, M. (1992). Aspiration by children with dysphagia. Developmental Medicine and Child Neurology (Abstract), 34(9, Suppl. 66), 37.
Aviv, J. E., Kim, T., Sacco, R. L., Kaplan, S., Goodhard, K., Diamond, B., & Close, L. G. (1998). FEESST: A new bedside endoscopic test of the motor and sensory components of swallowing. Annals of Otology, Rhinology and Laryngology, 107,378-387.
Bastian, R. W. (1991). Videoendoscopic evaluation of individuals with dysphagia: An adjunct to the modified barium swallow. Otolaryngology-Head and Neck Surgery, 104,339-350.
Bastian, R. W. (1993). The videoendoscopic swallowing study: An alternative and partner to the videofluoroscopic swallowing study. Dysphagia, 8, 359-367.
Christensen, J. R. (1989). Developmental approach to pediatric neurogenic dysphagia. DYSPhagia, 3, 131-134.
Cox, M. S., & Petty, J. (1991). A videofluoroscopy chair for the evaluation of dysphagia in patients with severe neuromotor disease. Archives of Physical Medicine and Rehabilitation, 72, 157-159.
Denhoff, E. (1981 ). Current status of infant stimulation or enrichment programs for children with developmental disabilities. Pediatrics, 67, 32-37.
Fraser, B., Hensinger, R., & Phelps, J. (1990). Physical management of multiple handicaps: A professional's guide. Baltimore: Paul H. Brookes.
Karnell, M. P. (1994). Videoendoscopy: From velopharynx to larynx. San Diego, CA: Singular Publishing Group.
Klein, D. C., & Seligman, M. E. P. (1976). Reversal of performance deficits in learned helplessness and depression. Journal of Abnormal Psychology, 85, 11-26.
Langmore, S. E., & McCulloch, T. M. (1997). Examination of the pharynx and larynx and endoscopic examination of pharyngeal swallowing. In A. L. Perlman & K. Schulze-Delrieu (Eds.), Deglutition and its disorders (pp. 201226). San Diego, CA: Singular Publishing Group.
Langmore, S. E., Schatz, K., & Olson, N. (1991). Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Annals of Otology, Rhinology & Laryngology, 100, 67"81.
Larnert, G., & Ekberg, 0. (1995). Positioning improves the oral and pharyngeal swallowing
function in children with cerebral palsy. Acta Paediatrica, 84, 689-692.
Leder, S. B., Ross, D. A., Briskin, K. B., & Sasaki, C. T. (1997). A prospective, double-blind, randomized study on the use of topical anesthetic, vasoconstrictor, and placebo during transnasal flexible fiberoptic endoscopy. Journal of Speech, Language, and Hearing Research, 40, 1352-1357.
Love, R. J., Hagerman, E. L., & Taimi, E. G.
( 1980). Speech performance, dysphagia, and oral reflexes in cerebral palsy. Journal of Speech and Hearing Disorders, 45, 59-75.
Miller, W. PL, & Seligman, M. E. P. (1975). Depression and learned helplessness in man. Journal of Abnormal Psychology, 84, 228-23&
Ohmae, Y., Logemann, J. A., Kaiser, P., Hanson, D. G., & Kahrilas, P. J. (1995). Timing of glottic closure during normal swallow. Head and Neck, 17,394-402.
Palmer, S., Thompson, R. J., & Linscheid, T. R. (1975). Applied behavior analysis in the treatment of childhood feeding problems. Developmental Medicine and Child Neurology, 17,333-339.
Perie, S., Laccourreye, L., Flahault, A., Hazebroucq, V., Chaussade, S., & St. Guily, J. L. (1998). Role of videoendoscopy in assessment of pharyngeal function in oropharyngeal dysphagia: Comparison with videofluoroscopy and manometry. Laryngoscope, 108, 1712-1716.
Thomas, A. P., Bax, M. 0., & Jenkins, D. P. L. (1989). The health and social needs of young adults with physical disabilities. Oxford, UK: Spastics International Medical Publications.
Williams, G. T., Farquharson, 1. M., & Anthony, J. (1975). Fiberoptic laryngoscopy in the assessment of laryngeal disorders. Journal of LarYngology and Otology, 89, 299-316. Received March 29, 1999
Accepted September 7, 1999
Contact author: Larry Migliore, Director of Speech Therapy, Matheny School & Hospital, P.O. Box 339, Peapack, NJ 07977.
E-mail: research@matheny.org
Key Words: endoscopy, fiberoptic, swallowing, developmental disability, dysphagia
Lawrence E. Migliore
Frederic J. Scoopo
Kenneth L. Robey
Matheny Institute of Applied Research, Matheny School & Hospital, Peapack, NJ
Copyright American Speech-Language-Hearing Association Nov 1999
Provided by ProQuest Information and Learning Company. All rights Reserved