Objective: We assessed the efficacy of a non-platinum-containing doublet chemotherapy of gemcitabine and vinorelbine as induction therapy prior to surgical resection in patients with stage IB-IIIA and selected stage IIIB non-small cell lung cancer (NSCLC). The primary clinical end point was radiographic disease response rate, and the secondary end points were pathologic response rate, treatment-related toxicity, surgical resectability and outcome, and overall and disease-free survival.
Methods: Patients underwent staging with CT of the chest and upper-abdomen, whole-body F-18 fluorodeoxyglucose positron emission tomography, bronchoscopy, and mediastinoscopy. The patients had to have medically and surgically resectable disease. Chemotherapy consisted of gemcitabine, 1,000 mg/[m.sup.2], and vinorelbine, 25 mg/[m.sup.2], administered on days 1, 8, 22, and 29. Imaging studies were repeated between days 43 and 50. Disease response was assessed by response evaluation criteria in solid tumors, and patients with resectable disease were offered surgery between days 50 and 70. Patients were followed up every 3 months for 2 years with chest CT.
Results: Between January 2000 and March 2004, 27 patients with stage IB NSCLC, 15 patients with stage II NSCLC, and 20 patients with stage III NSCLC were entered. After induction chemotherapy 34% (95% confidence interval [CI], 23 to 48%) had an objective radiographic response, 2% had a complete pathologic response, 90% underwent thoracotomy, and 77% underwent a complete resection. There were four deaths in the 6-week period following surgery, and there were no deaths related to chemotherapy. There were no unexpected morbidities from surgery or chemotherapy. The 1-year and 2-year overall survival rates were 80% (95% CI, 68 to 88%) and 65% (95% CI, 50 to 76%), and the median overall survival was 38.2 months.
Conclusions: Induction chemotherapy with gemcitabine and vinorelbine results in 1-year and 2-year survival rates and a median survival time comparable to those obtained with platinum-containing doublets. However, it appears to be less efficacious in terms of radiographic and pathologic response rates compared with platinum-containing chemotherapy doublets.
Key words: gemcitabine; neoadjuvant chemotherapy; non-small cell lung cancer; phase II trial; vinorelbine
Abbreviations: CI = confidence interval; CR complete response; DFS = disease-free survival; NSCLC = non-small cell lung cancer; OS = overall survival; pCR = pathologic complete response; PET = positron emission tomography; PR = partial response
**********
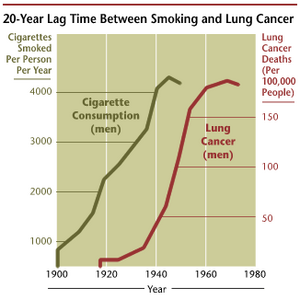
Lung cancer is a major public health problem, with an annual incidence of 170,000 to 180,000 cases and an estimated 163,500 deaths in 2005 in the United States alone. Non-small cell lung cancers (NSCLCs) represent approximately 75% of all lung cancers. Surgery with curative intent is feasible in one third of all patients with NSCLC. Of those, one third will survive 5 years and one sixth will survive 10 years. (1) The 5-year survival for resected lung cancer patients has a wide range, and it is shortest in those with involvement of mediastinal lymph nodes. Even small tumors of < 3 cm in diameter will result in 5-year survival rates of only 55% if accompanied by hilar lymph node involvement (T1N1). (2) Patients with ipsilateral mediastinal lymph node involvement, ie, N2 disease, have a 5-year survival rate of < 20%. (2)
The most common cause of death for patients after complete resection is disease recurrence outside of the field of surgical resection. Approximately 30% of patients with stage I and 60% of patients with stage II NSCLC may have involvement of mediastinal lymph nodes by molecular techniques. (3,4) Circulating cancer cells have been detected in peripheral venous blood of lung cancer patients. (5) Eradication of this early metastatic disease may potentially translate into a decreased incidence of recurrence in distant sites, thereby prolonging survival.
Adjuvant chemotherapy has been shown to be efficacious in prolonging survival. (6-8) The administration of chemotherapy prior to surgery (neoadjuvant or induction chemotherapy) is an alternate approach with the potential for higher rates of patient acceptability than adjuvant chemotherapy.
We conducted a phase II study of neoadjuvant chemotherapy with gemcitabine and vinorelbine in patients with resectable stage IB-IIIA and selected IIIB NSCLC (T4N0-2M0, satellite malignancy in the same lobe as the primary only) to assess the efficacy of a non-platinum doublet on the primary clinical study end point disease response (radiographic complete response [CR] and partial response [PR]) and the secondary end points (pathologic complete response [pCR] at surgery, disease-free survival [DFS], and overall survival [OS]).
MATERIALS AND METHODS
Patients with histologically confirmed NSCLC and stage IB (T2N0M0), IIA (T1N1M0), IIB (T2N1M0 and T3N0M0), or IIIA (T3N1M0 and T1-3N2M0) NSCLC were eligible for study participation. Patients with two lesions in one lobe (T4; stage IIIB) were also eligible, provided a lobectomy would encompass the satellite nodules. Patients with N2 disease were eligible if they were considered surgically resectable, ie, multistation lymph nodal involvement and bulky single-station lymph adenopathy were excluded (the largest N2 node diameter in this trial was 3.4 cm). Staging was determined by history, physical examination, routine laboratory evaluation, CT of the chest and upper-abdomen, whole-body F-18 fluorodeoxyglucose positron emission tomography (PET), bronchoscopy, and mediastinoscopy. ECG and pulmonary function tests were required. MRI of the brain was done on all patients with stage III disease, and MRI was performed in those with stage I or II disease only if clinically indicated. Patients were required to have had no prior therapy for lung cancer and could not have any other active cancer within 2 years except for non-melanoma skin cancers. The patients were required to be [greater than or equal to] 18 years of age, have a performance status of 0 to 1 by Eastern Cooperative Ontology Croup criteria, and have adequate hematologic, renal, and hepatic/function. Patients were required to have measurable or evaluable disease by response evaluation criteria in solid tumors. (9) Pregnancy was an exclusion, as were psychological, familial, sociologic, or geographic conditions that would not permit weekly medical follow-up or compliance with the study protocol. The study was approved by the Institutional Review Boards of participating institutions, and informed consent was obtained from all patients.
Eligible patients received preoperative chemotherapy with gemcitabine, 1,000 mg/[m.sup.2], and vinorelbine, 25 mg/[m.sup.2], administered on days 1, 8, 22, and 29; ie, two 3-week courses of chemotherapy. No dose escalation was allowed. Subsequent doses of chemotherapy were modified for toxicity if appropriate. All toxicities were graded according to common toxicity criteria (CTC version 2.0; National Cancer Institute; Bethesda, MD). Following chemotherapy, CT scans of chest and upper abdomen, whole-body PET scan, and pulmonary, function tests were repeated between days 43 and 50. Radiographic response was determined using response evaluation criteria in solid tumors. Patients with resectable disease had thoracotomy between days 50 and 70. Patients with unresectable disease and those with incomplete resection were treated at the discretion of their physician.
Surgery consisted of lobectomy or pneumonectomy with mediastinal lymph node dissection. For right-sided lesions, mediastinal lymph nodes included stations 2R, 4R, 7, 8, 9 and 10R; for left-sided lesions, mediastinal lymph nodes included 4L, 5, 6, 7, 8, 9, and 10L. Segmentectomy and wedge resection in place of lobectomy were not permissible for patients undergoing potentially curative resection.
Patients with complete resections had no further treatment. The use of postoperative radiation to the mediastinum in patients with N2 disease was left to the discretion of the treating physician. A total of four patients received adjuvant postoperative radiation, and a total of nine patients received curative-intent radiation for a less-than-complete surgical resection. All patients were followed up with interval history, physical examination, and CT scans at 3-month intervals for 2 years and thereafter every 6 months for disease recurrence.
Statistical Considerations
Confidence intervals (CIs) for proportions were computed using the method of Clopper and Pearson. Probabilities of OS and DFS were estimated using the method of Kaplan and Meier. Ninety-five percent CIs for these probabilities were estimated by adding and subtracting 1.96s to the estimated probability, where s was an estimate of the SE, computed using the Greenwood formula. OS was estimated from the date of diagnosis to the date of death or last observation. Those alive when last observed were considered right-censored as of that date. DFS was estimated for those with complete resection from the date of resection to the date of recurrence, death, or last observation. Those alive and disease free when last observed were considered right-censored as of that date. All statistical calculations were performed using statistical software (SAS version 9.1; SAS Institute; Cary, NC).
RESULTS
From January 2000 to March 2004, 62 patients were entered. The median age was 65 years (range, 32 to 82 years). Forty-five were men, and 17 were women. Pretreatment stages were IB (n = 27), IIA (n=2), IIB (n=13), IIIA (n=15), and IIIB (n = ,5). Adenocarcinoma was the most frequent histology (52%). Performance status was 0 in 33 patients and 1 in 29 patients. Seven patients reported weight loss, and 55 patients did not.
Induction Chemotherapy
Forty-two patients (68%) received all chemotherapy without dose reductions or close delays. Fifteen patients had either dose reductions or dose delays, and 5 patients had less than two induction cycles. Of these, two patients had increases in liver enzymes after day 1 and day 22, one patient progressed after day 15, one patient had grade 4 febrile neutropenia after day 8, and one patient did not wish to receive further chemotherapy after day 8.
Radiographic Response to Chemotherapy
Radiographic PRs were observed in 34% of patients (95% CI, 23 to 48%). There were no radiographic CRs (95% CI, 0 to 6%). Stable disease was noted in 53% (95% CI, 39 to 65%), and disease progression was noted in 13% (95% CI, 6 to 9.4%) of patients (Table 1). Response was not assessed in one patient who had liver enzyme elevation after the first dose of chemotherapy, disease stage IB, and a complete tumor resection.
Pathologic Response to Chemotherapy
Pathologic response of the primary tumor to induction chemotherapy was evaluated on standard hematoxylin-eosin histopathology on the 54 patients who underwent tumor resection. The percentage of necrosis and fibrosis was determined in increments of 5%, and it ranged from 0 to 95% (< 50% in 40 patients, > 50% in 12 patients, and not evaluable in 2 patients). A [greater than or equal to] 95% proportion of necrosis/sclerosis was observed in one patient (2%; 95% CI, 0 to 10%).
Mediastinal lymph nodes collected during mediastinoscopy were positive for metastatic disease in 13 patients on initial staging. In addition, one patient had aortopulmonary lymph nodal disease by CT and PET criteria. Eleven of these 14 patients underwent thoracotomy, and N2 nodes were positive in 9 patients and negative in 2 patients. In 48 patients, mediastinal lymph nodes were negative for metastatic disease on initial staging. Forty-five patients underwent thoracotomy, and N2 nodes were negative in 38 patients and positive in 7 patients.
Surgical Treatment
Fifty-six of 62 patients (90%) underwent thoracotomy. A complete resection was achieved in 48 patients (77%), including 24 of 27 patients with stage I disease, 11 of 15 patients with stage II disease, and 13 of 20 patients with stage III disease. Six patients had an incomplete resection, and two patients had no resection. The types of resection included lobectomy in 37 patients (left lower lobe [n = 2], left upper lobe [n = 11], right lower lobe [n = 7], right middle lobe [n = 1], right upper lobe [n = 16]), bilobectomy in 3 patients (right lower and middle lobe [n = 2], right upper and middle lobe [n = 1]), pneumonectomy in 13 patients (left-sided [n = 10], right-sided [n = 3]), and segmentectomy in 1 patient (right upper lobe; the patient had unresectable N2 disease at thoracotomy).
Treatment-Related Complications
Table 2 summarizes significant toxicities during chemotherapy. Grade 3 and 4 hematologic toxicities were noted in 17 patients. Five patients had febrile neutropenia, with documented infection in two patients (colitis in both). Severe anemia and thrombocytopenia were noted in two patients; two patients required transfusions. There were no deaths from hematologic toxicities.
Among nonhematologic toxicities, severe phlebitis was noted in one patient. Nausea and vomiting were uncommon. Short-lived myalgia and fatigue were noted in two patients. One patient had an eightfold increase in aspartate aminotransferase and alanine aminotransferase after the first dose of chemotherapy. There were no predisposing factors, and ultrasonography of the liver was normal. The patient did not receive further chemotherapy and was taken directly to surgery after recovery of liver function tests in 4 weeks. A second patient had a fourfold elevation in aspartate aminotransferase and alanine aminotransferase after day 8 of treatment. Laboratory tests normalized after 14 days, and the patient admitted use of alcohol.
Surgical Morbidity and Mortality
Four of the 54 patients with surgical resection died 11 to 40 days after surgery. The cause of death was respiratory failure in two patients; both had a right-sided pneumonectomy. One patient died from congestive heart failure. One patient died from pulmonary lymphangitic progression of squamous cell carcinoma found at autopsy, which was not noted at the time of surgical resection.
Survival
The index date for survival analysis was March 4, 2005, with a median follow-up time of 23.6 months. One-year OS was 80% (95% CI, 68 to 88%); 2-year OS was 65% (95% CI, 50 to 76%). The median OS time was 38.2 months (95% CI, 24.3 to [infinity] months; Fig 1). The 1-year DFS was 65% (95% CI, 49 to 77%), and the 2-year DFS was 49% (95% CI, 32 to 64%). The median DFS time was 21.4 months (95% CI, 12.9 to [infinity] months; Fig 2).
[FIGURES 1-2 OMITTED]
Variables Associated With Patient Outcome
Complete surgical resection was the most important variable associated with survival. Comparing the OS of patients with complete resection (n = 48) with those who had incomplete or no resection (n = 14), we found 1-year and 2-year survival rates of 87% (95% CI, 78 to 97%) and 74% (95% CI, 64 to 87%) for the former and 55% (95% CI, 28 to 82%) and 28% (95% CI, 0 to 58%) for the latter patients, respectively. The median OS time for patients with complete resection has not been reached (95% CI, 25.1 to [infinity] months), and it was 15.4 months (95% CI, 9.3 to 30.3 months) for those with incomplete resection (p = 0.004) [Fig 3]. Although a trend toward improved patient outcome for those with a radio-graphic response to chemotherapy was noted (Fig 4), this difference did not reach statistical significance (p = 0.25 for OS; p = 0.16 for DFS).
[FIGURES 3-4 OMITTED]
Patients with adenocarcinoma (n = 32) had a better OS (p = 0.08) than patients with other histopathologic subtypes (n = 30). Lifetime never-smokers (n = 5) had a better survival (p = 0.08) than ever-smokers (n =57). Women (n= 17) lived longer (p = 0.08) than men (n = 45). Disease stage (I vs II vs III) was not significantly associated with OS or DFS. Data are summarized in Table 1.
DISCUSSION
The study is the first to use a non-platinum doublet for induction chemotherapy in resectable NSCLC. The combination of vinorelbine and gemcitabine was well tolerated, and there was no chemotherapy-related mortality. Ninety percent of patients underwent thoracotomy, and 77% had a complete tumor resection. The 1-year and 2-year survival rates of 80% and 65% (87% and 74%, respectively, for patients with complete resections) and median survival time of 38.2 months were not different from those reported with platinum-containing regimens for a comparable group of patients (a summary of selected reports is provided in Table 3). (10-14) However, we observed a low pCR rate, and the clinical response rate of 34% was lower than rates reported for platinum-containing regimens in phase II and III studies. (10-14)
In recent prospective studies, (10-14) induction chemotherapy resulted in radiographic response rates of 56 to 70% (95% CI, approximately 46 to 83%) with a CR of 1.1 to 7.8% and a PR of 55 to 64% in patients with stage IB-IIIA (T2N0, T1-2N1 and T3N0, T3N1 and T1-3N2) with two to three cycles of a platinum agent combined with gemcitabine, paclitaxel, or docetaxel. Patients with pathologically proven N2 disease were reported to have negative N2 nodes on resection in approximately 50% of cases. A complete pathologic remission, defined as [greater than or equal to] 95% of each examined specimen consisting of fibrosis and necrosis, occurred in 6 to 16% of patients (95% CI, approximately 0 to 23%). The 1-year survival was approximately 77% (95% CI, approximately 71 to 83%), and the 2-year survival was approximately 59% (95% CI, approximately 52 to 66%). Disease progression during treatment was observed in 2 to 10% of patients, and a complete surgical resection was achieved in 70 to 92% of patients. (10-12,14)
We believed that it was important to devise a less toxic, yet efficacious regimen that is well tolerated and can be administered in an expedited fashion to allow surgery to be performed as early as possible. The two drugs in this study, gemcitabine and vinorelbine, have been studied in NSCLC. As single agent, gemcitabine has resulted in response rates of 20 to 30% in advanced-stage patients, and it is well tolerated. (15-17) Likewise, vinorelbine has resulted in response rates of 20 to 30% in advanced-stage patients, and it is well tolerated. (18) In combination, the two drags have shown overall response rates ranging from 13 to 73% in previously untreated patients with stage IV NSCLC. (19-26) Grade 3/4 hematologic toxicity is the most notable side effect of this regimen, and treatment-related mortality is very low. In our study, grade 3/4 toxicities were observed in "2,5 patients (40%) and consisted of neutropenia in 17 patients. A study (11) using platinum-based neoadjuvant chemotherapy reported grade 3/4 toxicity rates of approximately 60%, suggesting that the two-drug combination used here is better tolerated than platinum-based therapy.
pCR has been regarded as an important factor predictive of survival for NSCLC patients receiving induction chemotherapy followed by surgical resection. (27) Published rates of pCR range from 6 to 16% in prospective studies. (10-12,14) However, it is of note that in a large retrospective case series (13) of 446 patients treated mainly with platinum-containing regimens, the pCR rate was 4.5%. Thus, the relatively low pCR rate of 2% in our study is not unusual and cannot necessarily be attributed to the lack of a platinum agent in our regimen. In addition, it is possible that additional cycles of induction therapy may yield higher response rates. We used two cycles, while most previous studies used three cycles, flowever, the OS and DFS achieved with our regimen is equivalent to that reported by others.
The absence of disease in mediastinal lymph nodes at the time of surgery has been reported to be a strong predictor of survival. (14,28,29) In a study by the Southwest Oncology Group, (28)s the strongest predictor of survival after thoracotomy was the absence of tumor in the mediastinal lymph nodes (3-year survival of 44% vs 18%; p = 0.0005). In the long-term follow-up ease series by Martin et al, (13) 198 of 227 patients (87%) with N2 disease preoperatively had residual N2 disease at surgical resection. Neither the type of induction chemotherapy nor the use of preoperative radiation impacted survival in their study. In a multivariate analysis, complete tumor resection was significantly (p = 0.002) associated with survival, while N2 disease at surgery and pCR were not significantly associated with survival. Among a total of 198 patients with N2 disease at resection, those with a complete resection (n = 144) achieved a median survival of 20.7 months (95% GI, 14.8 to 26.5 months; 31% 3-year survival and 19% 5-year survival), which was significantly (p = 0.002) better than the survival of patients with incomplete or no resection (n = 54). Thus, a ease was made for complete resection in persistent N2 disease. This conclusion was echoed in a study of preoperative chemotherapy and radiation for stage IIIA/B NSCLC by Grunenwald et al. (30) In patients with complete resection despite positive mediastinal lymph nodes, the survival was better than in patients without surgical resection (p [less than or equal to] 0.0001). In our study, complete surgical resection was the best predictor of favorable outcome (p = 0.004), while disease stage was not (p = 0.24). A meaningful subgroup analysis of outcome for the 14 patients with N2 disease and complete resection (n = 6) vs incomplete resection (n = 8) cannot be performed because of the small numbers. In summary, a complete surgical resection appears to be the single most valuable parameter for a favorable outcome of patients.
To date, chemotherapy containing a platinum agent is considered to be the standard of care for patients with NSCLC (National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology, March 2005). However, in four randomized phase III trials (26,31-33) that compared platinum-containing regimens to a non-platinum regimen for patients with advanced disease, the non-platinum regimen was equivalent in efficacy and had less toxicity. Specifically, in the phase III randomized study of 287 patients by Laack et al, (26) a direct comparison between gemeitabine/vinorelbine with or without cisplatin did not result in an overall or progression-free survival benefit for patients receiving cisplatin. However, the overall response rate was significantly (p = 0.004) better for patients receiving cisplatin, while the rate of toxicity was significantly higher. Finally, in a randomized phase II study (25) of four regimens (gemeitabine/vinorelbine with or without carboplatin and gemeitabine/paclitaxel with or without carboplatin), all four regimens yielded comparable survival rates, while objective response rates were higher (34 to 42%) in the platinum-containing regimens as compared to the non-platinum regimens (both 29%). The combination of gemeitabine and vinorelbine had the least toxicity. Identical conclusions were reached in a recent metaanalysis (34) of platinum-containing vs non-platinum-containing chemotherapy in advanced NSCLC. Our results of gemeitabine and vinorelbine as induction chemotherapy prior to resection show the same trend, ie, a lower response rate than platinum-containing regimens, a better toxicity profile, and comparable OS. However, since this is the first report of such therapy administered as induction treatment prior to surgical resection, we suggest that confirmatory trials be done prior to using nonplatinum-containing neoadjuvant therapy outside of a clinical trial setting.
ACKNOWLEDGMENT: We wish to thank Amber Sapp and Carol Sherer for data management and clinical research support.
REFERENCE8
(1) Ruckdeschel JC, Schwartz AG, Bepler G, et al. Cancer of the lung: NSCLC and SCLC. In: Abeloff MD, Armitage JO, Niederhuber JE, et al, eds. Clinical oncology. Philadelphia, PA: Elsevier, 2004; 1649-1743
(2) Mountain C. Revisions in the international system for staging lung cancer. Chest 1997; 111:1710-1717
(3) Ahrendt SA, Yang SC, Wu L, et al. Molecular assessment of lymph nodes in patients with resected stage I non-small cell lung cancer: preliminary results of a prospective study. J Thorac Cardiovasc Surg 2002; 123:466-474
(4) D'Cunha J, Corfits AL, Herndon JE, et al. Molecular staging of lung cancer: real-time polymerase chain reaction estimation of lymph node micrometastatic tumor cell burden in stage I non-small cell lung cancer: preliminary results of Cancer and Leukemia Group B Trial 9761. J Thorac Cardiovasc Surg 2002; 123:484-491
(5) Peek K, Sher Y, Shih J, et al. Detection and quantitation of circulating cancer cells in the peripheral blood of lung cancer patients. Cancer Res 1998; 58:2761-2765
(6) Le Chevalier T. Results of the randomized International Adjuvant Lung Cancer Trial (IALT): cisplatin-based chemotherapy (CT) versus no CT in 1867 patients with resected non-small cell lung cancer [abstract]. Proc Am Soc Clin Oncol 2003; 22:2
(7) Winton TL, Livingston R, Johnson D, et al. A prospective randomized trial of adjuvant vinorelbine and cisplatin in completely resected stage IB and II non-small cell lung cancer Intergroup JBR. 10 [abstract]. Proc Am Soc Clin Oncol 2004; 22:7018
(8) Strauss GM, Herndon J, Maddaus MA, et al. Randomized clinical trial of adjuvant chemotherapy with paclitaxel and carboplatin following resection in stage IB non-small-cell lung cancer: report of the Cancer and Leukemia Group B protocol 9633 [abstract]. Proc Am Soc Clin Oncol 2004; 23:7019
(9) Therasse P, Arbuck SG, Eisenhauer EA, et 'al. New guidelines to evaluate the response to treatment in solid tumors: European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 2000; 92:205-216
(10) van Zandwijk N, Smit EF, Kramer GW, et al. Gemcitabine and cisplatin as induction regimen for patients with biopsyproven stage IIIA N2 non-small-cell lung cancer: a phase II study of the European Organization for Research and Treatment of Cancer Lung Cancer Cooperative Group (EORTC 08955). J Clin Oncol 2000; 18:2658-2664
(11) Pisters KM, Ginsberg RJ, Giroux DJ, et al. Induction chemotherapy before surgery for early-stage lung cancer: a novel approach. Bimodality Lung Ontology Team. J. Thorac Cardiovasc Surg 2000; 119:429-439
(12) Depierre A, Milleron B, Moro-Sibilot D, et al. Preoperative chemotherapy followed by surgery compared with primary surgery in resectable stage I (except T1N0), II, and IIIa non-small-cell lung cancer. J Clin Oncol 2002; 20:247-253
(13) Martin J, Ginsberg R, Venkatraman ES, et al. Long-term results of combined-modality therapy in resectable nonsmall-cell lung cancer. J Clin Oncol 2002; 20:1989-1995
(14) Bettieher DC, Schmitz SFH, Toetsch M, et al. Mediastinal lymph node clearance after docetaxel-cisplatin neoadjuvant chemotherapy is prognostic of survival in patients with stage IIIA pN2 non-small-cell lung cancer: a multicenter phase II trial. J Clin Oncol 2003; 21:1752-1759
(15) Shepherd FA. Phase II trials of single agent activity of gemcitabine in patients with advanced non-small cell lung cancer: an overview. Anticancer Drugs 1995; 6(Suppl6): 19-25
(16) Shepherd FA, Abratt RP, Anderson H, et al. Gemcitabine in the treatment of elderly patients with advanced non-small cell lung cancer. Strain Oncol 1997; 24(Suppl7):750-755
(17) Johnson DH. Gemcitabine for the treatment of non-small cell lung cancer. Ontology 2001; 3(Suppl):33-39
(18) Gridelli C, Cigolari S, Gallo C, et al. Activity and toxicity of gemeitabine and gemeitabine plus vinorelbine in advanced non-small-cell lung cancer elderly patients: phase II data from the Multicenter Italian Lung Cancer in the Elderly Study randomized trial. Lung Cancer 2001; 31:277-284
(19) Lorusso V, Carpagnano F, Frasei G, et al. Phase I/II study of gemcitabine plus vinorelbine as first-line chemotherapy of non-small-cell lung cancer. J Clin Oncol 2000; 18:405-411
(20) Gridelli C, Frontini L, Perrone F, et al. Gemcitabine plus vinorelbine in advanced non-small-cell lung cancer: a phase II study of three different doses. Br J Cancer 2000; 83:707-714
(21) Chen YM, Perng RP, Yang KY, et al. A multicenter phase II trial of vinorelbine plus gemcitabine in previously untreated inoperable (stage IIIB/IV) non-small-cell lung cancer. Chest 2000; 117:1583-1589
(22) Lilenbaum R, Cano R, Schwartz M, et al. Gemcitabine and vinorelbine in advanced non-small-cell lung carcinoma. Cancer 2000; 88:557-562
(23) Krajnik G, Mohn-Staudner A, Thaler J, et al. Vinorelbine gemeitabine in advanced non-small-cell lung cancer: an AASLC phase II trial; Austrian Association for the Study of Lung Cancer phase II trier. Ann Oneol 2000; 11:993-998
(24) Baron F, Cueva J, Grana B, et al. Gemcitabine plus vinorelbine for the treatment of advanced non-small-cell lung cancer. Eur J Cancer 2001; 87:1381-1384
(25) Greco FA, Gray JR, Thompson DS, et al. Prospective randomized study of (bur novel chemotherapy regimens in patients with advanced non-small-cell lung carcinoma. Cancer 2002; 95:1279-1285
(26) Laack E, Diekgreber N, Mueller R, et al. Randomized phase III study of gemcitabine and vinorelbine versus gemcitabine, vinorelbine, and cisplatin in the treatment of advanced non-small-cell lung cancer: from the German and Swiss Lung Cancer Study Group. J Clin Oncol 2004; 22:2348-2356
(27) Pisters KM, Kris MG, Gralla RJ, et al. Pathologic complete response in advanced non-small-cell lung cancer following preoperative chemotherapy: implications for the design of future non-small-cell lung cancer combined modality trials. J Clin Oncol 1993; 11:1757-1762
(28) Albain KS, Rusch VW, Crowley JJ, et al. Concurrent cisplatin/ etoposide plus chest radiotherapy followed by surgery for stages IIIA (N2) and IIIB non-small-cell lung cancer: mature results of Southwest Oncology Group phase II study 8805. J Clin Oncol 1995; 13:1880-1892
(29) Bueno R, Richards WG, Swanson SJ, et al. Nodal stage alter induction therapy for stage IIIA lung cancer determines patient survival. Ann Thorac Surg 2000; 70:1826-1831
(30) Grunenwald DH, Andre F, Le Peehoux C, et al. Benefit of surgery after chemoradiotherapy in stage IIIB (T4 and/or N3) non-small-cell lung cancer. J Thorac Cardiovasc Surg 2001; 122:796-802
(31) Georgoulias V, Papadakis E, Alexopoulos A, et al. Platinum-based and non-platinum-based chemotherapy in advanced non-small-cell lung cancer: a randomized multicentre trial. Lancet 2001; 357:1478-1484
(32) Kosmidis P, Mylonakis N, Nicolaides C, et al. Paclitaxel plus carboplatin versus gemeitabine plus paclitaxel in advanced non-small-cell lung cancer: a phase III randomized trial. J Clin Oncol 2002; 20:3578-3585
(33) Smit EF, van Meerbeeck JPAM, Lianes P, et al. Three-arm randomized study of two cisplatin-based regimens and paclitaxel plus gemcitabine in advanced non-small-cell lung cancer: a phase III trial of the European Organization for Research and Treatment of Cancer Lung Cancer Group EORTC 08975. J Clin Oncol 2003; 21:3909-3917
(34)d D'Addario G, Pintilie M, Leighl NB, et al. Platinum-based versus non-platinum-based chemotherapy in advanced non-small-cell lung cancer: a meta-analysis of the published literature. J Clin Oncol 2005; 23:1-11
* From the H. Lee Moffitt Cancer Center and Research Institute (Drs. Sommers, Robinson, Sharma, Cantor, and Bepler), Tampa, FL; and Roswell Park Cancer Institute (Drs. Ranmath and Nwogu), Buffalo, NY.
This work was support by grants from Glaxo-Smith-Kline to Dr. Ramnath and Eli Lilly to Dr. Bepler.
Manuscript received March 23, 2005; revision accepted May 24, 2005.
Reproduction pf this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Gerald Bepler, MD, PhD, H. Lee Moffitt Cancer Center and Research Institute, Thoraic Oncology Program, MRC-4W, 12902 Magnolia Dr, Tamap, FL 33612: e-mail: beplerg@moffitt.usf.edu
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group