People who make a particular form of an immune system protein have a heightened risk of developing old-age blindness, three teams of researchers report in an upcoming Science.
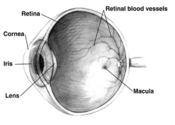
In a search for the factors underlying age-related macular degeneration--a deterioration of the eye that is the primary cause of vision loss in the elderly--the researchers have implicated one of several variants of the gene that encodes the protein called complement factor H, or CFH.
The scientists hypothesize that this version of CFH fails to rein in inflammatory proteins, the protein's normal role. This braking of inflammation is indispensable to the eyes of some elderly people, the new studies suggest.
As people age, microscopic damage accumulates in their eye tissues. In many people, this results in formation of drusen, a yellowish combination of fats, proteins, and cellular debris. In people with macular degeneration, large amounts of drusen destroy eye tissue.
Using blood samples, the researchers analyzed the genetics of macular degeneration patients and elderly people who didn't have the condition. "We scanned across the genome to see what contrasts there were ... and [the CFH gene] came up," says Yale University statistician Josephine Hoh.
Hoh's team found that people who inherit the variant of CFH have a risk of macular degeneration up to seven times as great as do people without the variant.
The other two groups of researchers took a slightly different approach, looking for differences specifically on chromosome 1 because earlier studies had hinted that a gene there was associated with macular degeneration. These teams turned up the same CFH variant reported by Hoh. They conclude that the variant boosts risk threefold and estimate that it could account for roughly half of all age-related macular degeneration cases.
Because drusen contains proteins produced by the complement branch of the immune system, scientists had suspected that the complement system plays a role in macular degeneration. Complement proteins orchestrate inflammation around sites of tiny eye injuries, walling them off and preventing infection.
Unfortunately, inflammation adds to drusen deposits in the eye and may further damage tissue, says Albert O. Edwards, an ophthalmologist at the Presbyterian Hospital of Dallas and a coauthor of one of the studies.
The new reports bolster the link between complement-protein genes and macular degeneration, says Stephen P. Daiger, a geneticist at the University of Texas Health Science Center in Houston. "Three independent studies using different sets of people point to the same location on the same gene," he says. "That's pretty persuasive."
Despite the new findings, the mechanism by which the CFH variant might lead to macular degeneration remains murky. Although that form of the gene "clearly puts you at risk," it's a common variant, notes Margaret A. Pericak-Vance of Duke University in Durham, N.C., who coauthored one of the studies. "Not everybody who carries it will have macular degeneration, and it certainly doesn't act alone."
The prevalence of the variant in the population remains unknown.
Experiments might clarify how a protein encoded by the variant causes or exacerbates macular degeneration and indicate whether anticomplement drugs would fight this cause of blindness, says eye surgeon Eric A. Postel of Duke.
Edwards predicts that, in the future, people will be screened for the gene variant if they are deemed at high risk of macular degeneration. Risk factors include drusen deposits, high blood pressure, smoking, and a close relative with the disease.
STATS
10 million
People in the United States with macular degeneration
COPYRIGHT 2005 Science Service, Inc.
COPYRIGHT 2005 Gale Group