Week after week in late 2003, Kija Ng'habi spent his mornings capturing mosquitoes. In the Tanzanian village of Lupiro, he and a colleague would go from house to house, noting where they'd found each live insect. In spite of the bed nets beneath which most of the houses' occupants slept, many mosquitoes had taken blood meals during the night. The two mosquito hunters frequently found red and bloated insects on the walls of the 10 homes in their survey.
After Ng'habi secured the day's catch in polystyrene cups covered with netting, he would return to the laboratory to count how many of the mosquitoes previously collected from each house had died since the day before. He'd also determine what had killed them. In all, the student researcher at Ifakara Health Research and Development Centre and his colleague Ernst-Jan Scholte of Wageningen University in the Netherlands caught and examined about 3,000 mosquitoes. "It was a tiresome job," Ng'habi says.
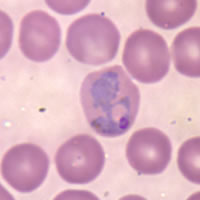
But the payoff may be great: a new weapon in the battle against malaria, which biting mosquitoes spread from person to person. Two papers by independent research teams in the June 10 Science indicate that fungi can either kill the mosquitoes or reduce the efficiency with which they transmit Plasmodium, the malaria parasite.
HASTENING DEATH In one of the Science papers, Ng'habi, Scholte, and their co-workers report that Anopheles mosquitoes from five of the houses in Lupiro, a hot spot for malaria, died sooner than did mosquitoes from the five other dwellings surveyed. The less robust insects came from homes in which the researchers had set out cloth sheets covered with spores of a fungus, known as Metarhizium anasopliae, that can lethally infect mosquitoes and some other insects. On contact, the spores germinate and penetrate the insect, then gradually spread throughout its body.
The other Science paper describes laboratory experiments by Andrew Read of the University of Edinburgh, Matt B. Thomas of the Imperial College London in Wye, and their colleagues also in the United Kingdom. They exposed Anopheles mosquitoes to various strains of fungi that have been used against locusts and other agricultural pests. Within 14 days of exposure to any of the six most effective strains, including one called Beauveria bassiana, 90 percent or more of the mosquitoes died. Of unexposed mosquitoes, only about 20 percent died in that same amount of time.
Even mosquitoes that did survive at least 2 weeks after exposure to the fungus appeared to have a reduced capacity to spread malaria, says Thomas. The group found that among mosquitoes that had fed on mice with malaria, those that were then exposed to B. bassiana fungi were later less likely to carry Plasmodium than were unexposed mosquitoes.
The 14-day mark is important because it takes about that long for the malaria parasite to reproduce and mature inside the insect and to become capable of spreading to a new human host. If the mosquito dies in the meantime, it can't transmit the disease.
According to both sets of authors, a fungus-based insecticide could be ready for widespread deployment in 3 to 5 years. M. anasopliae, like B. bassiana, already appears in approved agricultural pesticides used in parts of Africa.
The stakes are high. Each year, an estimated 700,000 to 3 million people die from malaria, and about 400 million cases occur worldwide. In regions where the parasitic disease is endemic, one infection blurs into the next. The average person in Lupiro annually receives 262 malaria-transmitting mosquito bites, says Ng'habi.
He, Scholte, and their colleagues calculate that outfitting all houses in Lupiro with spore-impregnated cloth sheets would reduce the average number of malaria-spreading mosquito bites to about 64 per person per year. A spore-containing spray that could be applied directly to interior surfaces of each vulnerable home would further reduce that number, they say.
REPLACEMENT TOOL Weapons currently in use against malaria include chemical insecticides that kill mosquitoes in the environment and bed nets, often impregnated with insecticide, that provide some protection for people as they sleep. But the insecticides carry environmental costs. DDT exemplifies this tradeoff (SN: 7/1/00, p. 12). Once considered a triumph of public health, it was later found to have detrimental effects on people and animals.
Chemical insecticides can also give rise to pesticide-resistant mosquitoes. Such resistance is "patchy across Africa, but it's definitely spreading," says Read. "There are mosquitoes around now that are resistant to the insecticides on bed nets."
"Fungi provide a very good alternative in places where resistance to the insecticides used on bed nets has already appeared," says evolutionary biologist Yannis Michalakis of the Research Institute for Development in Montpellier, France. Elsewhere, he adds, "the fungi and insecticide[-treated] bed nets could be used in combination."
Michalakis, who did not participate in either of the studies recently reported in Science, says that fungus-based insecticides are potentially "much more environmentally friendly" than chemical sprays.
Fungal sprays could nevertheless kill nontarget insect species, says Read, "out most of those are species people don't want anyway."
A number of obstacles remain. "We need to work on a formulation that makes spores survive longer in the field," says Bart G.J. Knols of Wageningen University, who was part of the Tanzanian study. In the current formulation, a solution mixed with a little vegetable oil, the spores appear to remain effective only for about 3 weeks, suggesting that frequent applications would be required. Most chemical treatments last for 6 months or more, Knols notes.
In time, Michalakis adds, either mosquitoes or malaria parasites could evolve ways to circumvent the new fungal tactic. The parasites might accelerate their development so that they could spread from a fungus-infected mosquito to a person before the insect carrier dies, for example. Also, mosquitoes might alter their behavior so that they become less likely to remain inside homes after feeding, thereby minimizing contact with the fungi.
Knols acknowledges those possibilities but he says that mosquitoes and the parasites are less likely to evolve resistance to an organism such as a fungus, which can evolve countermeasures in response, than they are to a chemical agent.
Such potential obstacles notwithstanding, Read sees good reason to pull out the stops in fighting malaria mosquitoes. "Hit these things with everything you've got," he says.
COPYRIGHT 2005 Science Service, Inc.
COPYRIGHT 2005 Gale Group