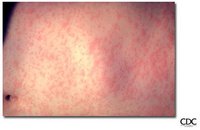
Measles continues to be a leading cause of childhood morbidity and mortality in developing countries and an outbreak threat in the majority of countries. In 2000, measles was considered the fifth leading cause of childhood mortality, and the World Health Organization (WHO) estimated that approximately 777,000 measles-associated deaths occurred worldwide. In 2001, WHO and the United Nations Children's Fund (UNICEF) developed a 5-year strategic plan, endorsed by the World Health Assembly in 2003, to reduce measles mortality by 50% by 2005 (relative to 1999 estimates) and to achieve and maintain interruption of indigenous measles transmission in large geographic areas with established measles elimination goals. This plan included strengthening routine vaccination coverage, providing a second opportunity for measles immunization to children, improving measles case management, and improving surveillance with laboratory confirmation of suspected measles cases (1). To date, four of six WHO regions have established measles elimination targets: the Americas Region (AMR) by 2000, the European Region (EUR) by 2010, the Eastern Mediterranean Region (EMR) by 2010, and the Western Pacific Region (WPR) by 2012. The remaining two WHO regions, the African (AFR) and South East Asian (SEAR) regions, are continuing work toward the measles mortality reduction goal. Likewise, to reduce the burden of disease from congenital rubella syndrome (CRS), currently estimated at 100,000 cases per year worldwide, several countries have developed or continue to develop rubella control programs, and AMR and EUR have established regional rubella elimination and CRS reduction goals, respectively. Because improved global surveillance is essential for monitoring progress toward mortality reduction and elimination of these diseases, WHO established the Measles and Rubella Laboratory Network (LabNet) in 2003 to promote case identification and confirmation. This report provides an update on the development of LabNet during January 2004--June 2005 and describes the geographic distribution of measles and rubella virus genotypes as of June 2005.
LabNet
On the basis of the model provided by the WHO Polio Laboratory Network, WHO established the Global Measles Laboratory Network (GMLN) in 2000 to 1) provide laboratory confirmation of initial measles cases during outbreaks, 2) collect baseline measles genotype information on the regional distribution of circulating viruses useful in establishing transmission pathways of disease spread, and 3) monitor the success of vaccination campaigns and the integrity of elimination programs (2). Because of the similar nature of clinical surveillance and diagnostic assay procedures, GMLN also provided diagnostic support for rubella control programs and has since evolved into LabNet.
Clinical recognition of cases has low positive predictive value when the incidence of measles and rubella is low. Thus, LabNet selected highly sensitive and specific, commercially available, IgM enzyme immunoassays (EIAs) for laboratory confirmation of suspected cases of measles and rubella. LabNet includes IgM testing laboratories serving 162 countries and is still expanding. A total of 705 laboratories participate in the network, which consists of three global specialized laboratories, 16 regional reference laboratories, 178 national laboratories, and 508 subnational laboratories. More than 86,000 serum samples were tested for IgM for measles and rubella in 2004, often meeting result-reporting targets of at least 80% within 7 days of receiving the sample (Table).
The network has expanded in all WHO regions since 2003 but particularly in the WPR and AFR regions. In September 2005, WPR adopted the goal of measles elimination, with strengthening of laboratory testing as a key component of its measles surveillance strategy. AFR has implemented strategies for measles mortality reduction and has established laboratory-based surveillance before, or at times coincident with, countries beginning measles supplementary immunization activities. Thirty-six of 46 AFR countries have established measles laboratories as part of LabNet, with staff who have received training from regional or global laboratories. LabNet has been developed with a long-term objective of responsiveness to developing public health priorities in the WHO regions. For example, the laboratory network established in AMR supports 1) pursuing regional elimination goals for rubella and CRS and 2) continuing case-based investigations of measles now that elimination of indigenous measles from the region has been achieved.
Performance Monitoring
A comprehensive system for monitoring indicators of laboratory performance, including proficiency testing and annual laboratory accreditation by WHO and/or regional laboratories, has been implemented in all regions. Six quality indicators * are monitored during the 12-month review period, and a comprehensive onsite review of laboratory activities, procedures, and communication links is performed every 2-3 years. All regions have begun this process, with priority given to regions with a high burden of measles, such as AFR, SEAR, and EMR. Sixty-two (43%) of 144 national and regional reference laboratories in these three regions have been assessed, with only one failing to receive accreditation.
The IgM proficiency testing program is in its fifth year, and more than 160 panels of 20 sera will be distributed in 2005. Analysis of the 2004 measles proficiency panel resulted in 90% of 100 national laboratories achieving the pass score of at least 90%. Laboratories that fail the test are visited by WHO laboratory program officials. Problems usually are identified rapidly, deficiencies are corrected, and the laboratories are permitted to attempt the proficiency tests again.
Alternative Specimen Collection
LabNet is active in developing new techniques to improve laboratory surveillance. Dried blood and oral fluid samples as an alternative to serum have been evaluated recently for measles and rubella testing. These sampling techniques might be useful when countries have difficulty in collecting venepuncture blood from infants or transporting samples under conditions of reverse cold chain to a testing laboratory. Good concordance of both oral fluid and dried blood samples with parallel serum samples was documented for measles using commercially available assays (WHO, unpublished data, 2005); however, limited data are available for rubella. IgM in dried blood and oral fluid is stable at (68[degrees]F [20[degrees]C]) for up to 1 week; however, additional data are needed regarding stability at higher temperatures.
Virus Characterization
Because molecular epidemiologic techniques provide an important tool for tracking viral transmission pathways, LabNet also supports genetic characterization of currently circulating strains of measles and rubella viruses. LabNet has standardized the nomenclature and laboratory procedures used to describe the genetic characteristics of wild-type measles (3-6) and rubella viruses (7,8); these protocols are included in all WHO-sponsored laboratory training courses. This standardization has allowed sharing of virologic surveillance data among laboratories and permitted efficient communication of these data throughout the measles and rubella control programs.
WHO currently recognizes 23 genotypes of measles virus. Although virologic surveillance for measles is still incomplete, a pattern for the global distribution of genotypes within disease-endemic regions is emerging (Figure 1). In countries that have not yet interrupted measles transmission, the sequence analysis of measles isolates has revealed a limited geographic distribution of genotypes, whereas in countries that have eliminated measles, several genotypes have been detected in association with limited outbreaks, reflecting the various imported sources of these viruses.
[FIGURE 1 OMITTED]
The systematic nomenclature for wild-type rubella viruses developed in 2004 and 2005 is an important advance in virologic surveillance for rubella. Seven genotypes and three additional provisional genotypes of rubella virus are recognized by WHO (Figure 2). These genotypes are classified into two clades (i.e., groups of similar genotypes), designated 1 and 2; clade 2 viruses have not been found circulating in the western hemisphere. Although knowledge concerning the geographic distribution of rubella genotypes has progressed substantially since 2003, the genotypes of rubella viruses present in many countries and regions remain unknown. LabNet encourages the collection and storage of viruses for genetic characterization.
[FIGURE 2 OMITTED]
Acknowledgments
This report is based on data contributed by the member laboratories of the WHO Global Measles and Rubella Laboratory Network. PM Strebel, MBChB, DA Featherstone, Immunization, Vaccines, and Biologicals, WHO, Geneva, Switzerland. L Cairns, MD, V Dietz, MD, Global Measles Br, Global Immunization Div, National Immunization Program, CDC.
Editorial Note: Measles and rubella elimination and control programs depend on effective global surveillance. LabNet promotes case identification and confirmation, thus improving the quality of disease surveillance and furthering progress toward elimination of these diseases. The development of LabNet has progressed rapidly during the past 5 years. More than 190 national and regional reference laboratories have been equipped and trained to perform IgM ELISA procedures, and the number of measles serum samples tested in 2004 has increased 32% compared with 2003. Many countries have taken the opportunity to use this capability and expand their laboratory-based surveillance by testing for diseases endemic in their respective regions that have similar clinical features (e.g., dengue, parvovirus B19, and HHV-6) or where similar diagnostic assays might be used (e.g., yellow fever and Japanese encephalitis). Virologic surveillance data, when analyzed in conjunction with standard epidemiologic data, can help document viral transmission pathways and aid in case classification. If baseline information regarding circulating genotypes is available, molecular epidemiologic data can also help to document the elimination of endemic transmission and, therefore, provide a means to measure the effectiveness of control programs. Virologic surveillance has provided evidence of the interruption of endemic transmission of measles virus in the western hemisphere (9) and rubella virus in the United States (10). However, epidemiologic and molecular surveillance activities, coupled with active vaccination programs, must be continued as long as the threat of disease importation exists.
As new laboratories are established, surveillance improves, and laboratory workloads increase, important challenges remain in maintaining quality and meeting the resource needs of the measles and rubella LabNet. These challenges include identifying funding resources for laboratory supplies for measles and rubella testing and encouraging countries to integrate these costs into national surveillance budgets whenever possible. In addition, partners must pursue a means of 1) gaining access to data from laboratories in countries with extensive private laboratory structures for measles and/or rubella surveillance and 2) expanding the quality-assurance program for all laboratories within LabNet, including those at the subnational level. ([dagger])
References
(1.) World Health Organization. Measles mortality reduction and regional elimination strategic plan 2001-2005. Geneva, Switzerland: World Health Organization; 2001. WHO/V&B/01/13.
(2.) Featherstone D, Brown D, Sanders R. Development of the Global Measles Laboratory Network. J Infect Dis 2003; 187(Suppl 1):S264-9.
(3.) World Health Organization. Standardization of the nomenclature for describing the genetic characteristics of wild-type measles viruses. Wkly Epidemiol Rec 1998;73:265-9.
(4.) World Health Organization. Nomenclature for describing the genetic characteristics of wild-type measles viruses (update), part I. Wkly Epidemiol Rec 2001;76:241-7.
(5.) World Health Organization. Nomenclature for describing the genetic characteristics of wild-type measles viruses (update), part II. Wkly Epidemiol Rec 2001;76:249-51.
(6.) World Health Organization. New genotype of measles virus and update on global distribution of measles genotypes. Wkly Epidemiol Rec 2005;80:347-51.
(7.) World Health Organization. Standardization of the nomenclature for genetic characteristics of wild-type rubella viruses. Wkly Epidemiol Rec 2005;80:126-32.
(8.) World Health Organization. Rubella nomenclature meeting recommendations. Geneva, Switzerland: World Health Organization; 2004. Available at http://www.mayeticvillage.com/who-rubellagenotype. User name: rubella; password: rubella.
(9.) CDC. Progress toward measles elimination--Region of the Americas, 2002-2003. MMWR 2004;53:304-6.
(10.) CDC. Achievements in public health: elimination of rubella and congenital rubella syndrome--United States, 1969-2004. MMWR 2005; 54:279-82. * Annual accreditation requires meeting the following six criteria: 1) test results are reported on at least 80% of received samples within 7 days of receipt, 2) serologic/reverse-transcriptase polymerase chain reaction (RT-PCR) tests are performed on at least 100 specimens annually, 3) accuracy of diagnostic assays for measles and rubella IgM or RT-PCR identification is at least 90%, 4) internal quality control procedures for IgM assays are in place, 5) proficiency test score of at least 90% on WHO-distributed serum panel is achieved, and 6) the score from the annual onsite review of laboratory operating procedures and practices is at least 80%.
([dagger]) In accordance with the consensus of the Third WHO Global Measles and Rubella Laboratory Network Meeting held in Geneva, Switzerland, on August 25-26, 2005. The meeting was attended by representatives from all the global specialized and regional reference laboratories in LabNet, laboratory coordinators from all six WHO regions, and key partners.
PA Rota, PhD, JP Icenogle, PhD, JS Rota, MPH, WJ Bellini, PhD, Div of Viral and Rickettsial Diseases, National Center for Infectious Diseases, CDC.
COPYRIGHT 2005 U.S. Government Printing Office
COPYRIGHT 2005 Gale Group