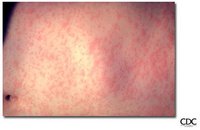
On May 29, 2005, the Indiana State Department of Health (ISDH) was notified of suspected measles in a female Indiana resident aged 6 years who was hospitalized in Cincinnati, Ohio, where she had been visiting relatives. Serologic analyses performed by the Ohio State Department of Health Laboratory and a private reference laboratory confirmed the diagnosis of measles. The hospital in Cincinnati and the girl's parents told ISDH she had been at a church gathering in northwestern Indiana on May 15 where a fellow attendee had been ill. This fellow attendee was an adolescent girl aged 17 years, an Indiana resident who had not been vaccinated for measles and who had worked during May 4-14 as a missionary in an orphanage and hospital in Bucharest, Romania, where a large measles outbreak was subsequently reported. The teen had returned to the United States with prodromal fever, cough, conjunctivitis, and coryza, traveling on international and" domestic commercial airliners on May 14. The next day the teen attended the church gathering along with others who had not been vaccinated because of nonmedical exemptions. Family members recalled that the teen had a rash on May 16; measles was diagnosed retrospectively, and the teen was identified as the index patient. An outbreak investigation was conducted by ISDH and CDC. This report summarizes 1) the results of that investigation, which identified 34 persons with measles, including three who required hospitalization, 2) the measures taken to control and prevent measles transmission, and 3) recommendations to prevent future cases of measles. Persons with measles were defined as having generalized maculopapular rash, fever of [less than or equal to] 101[degrees]F ([less than or equal to] 38.3[degrees]C), and at least one of the following: cough, coryza, or conjunctivitis. Measles cases were either laboratory-confirmed or met the clinical case definition and were linked epidemiologically to a patient with confirmed measles. Onset of rash for the 34 persons identified with measles occurred during May 16-June 24 (Figure). Of the 34 cases, 33 (97%) were in church members who acquired disease either through direct exposure to the index patient or household exposure to a person with measles who had been exposed to the index patient. The remaining case was in a phlebotomist, with rash onset on June 24, who worked in an Indiana hospital where one of the measles patients had been admitted; however, exposure of the phlebotomist to any of the patients in the outbreak was not identified. The phlebotomist had received 1 dose of measles-containing vaccine (MCV) as a child, according to a school record.
Among the measles patients, 33 were residents of Indiana and one resided in Illinois. Patients ranged in age from 9 months to 49 years (median age: 12 years); vaccination with MCV was documented for two (6%) persons, one who had received 1 dose, and one who had received 2 doses. Of the 34 cases, 14 (41%) were laboratory confirmed either by serologic testing that detected measles-specific IgM antibodies, polymerase chain reaction analysis of urine specimens, or both; the other 20 cases were in patients with rash illness who were linked epidemiologically to the confirmed cases. Three (9%) of the 34 patients were hospitalized, two (aged 6 and 45 years) with dehydration and one (aged 34 years) with pneumonia who required 6 days of ventilator support. Among the 31 nonhospitalized patients, complications included 16 cases of diarrhea and two cases of otitis media.
The outbreak was controlled by multiple actions taken by state and local health departments in Indiana, Ohio, and Illinois. These measures included 1) voluntary isolation of patients, 2) tracing of potentially exposed patient contacts by local and state health departments in all three states and by staff members at hospitals in Indiana and Ohio, 3) administering vaccine and immunoglobulin to susceptible contacts, 4) voluntary home quarantine among those who refused vaccination, 5) checking immune status of health-care workers, 6) alerting hospitals to the measles outbreak and urging physicians to report all suspected cases, and 7) increasing media attention to health risks posed to the community by persons who refuse vaccination.
Editorial Note: The measles outbreak described in this report was the largest in Indiana since 1990 and the largest in the United States since 1996 (1,2). The outbreak resulted from a gathering of church members who had not been vaccinated for measles and could have been prevented if the index patient had been adequately vaccinated before traveling to Romania.
Measles is a highly infectious acute viral illness that can cause severe pneumonia, diarrhea, encephalitis, and death. Although an effective vaccine has been available since 1963, an estimated 30-40 million measles cases and 530,000 deaths from measles occur annually worldwide (3). Ongoing measles transmission has been eliminated in the United States by high vaccination levels (4). Of 540 measles cases in the United States during 1997-2001, 362 (67%) were linked to imports (i.e., 196 imported cases, 138 cases epidemiologically linked to imported cases, and 28 cases associated with an imported measles virus genotype), and most measles cases could have been prevented (5).
Because the disease is endemic or epidemic in many parts of the world (63, the Advisory Committee on Immunization Practices (ACIP) recommends that all persons who travel internationally be vaccinated for measles to reduce the risk for infection among travelers (7). ACIP further recommends that all preschool children in the United States receive 1 dose of MCV and all school-aged children receive 2 doses of MCV. Although all states require 2 doses of MCV for children attending school, nonmedical exemptions are permitted by certain states, including Indiana. Persons choosing a nonmedical exemption from vaccination are approximately 22 times more likely to acquire measles than persons who are vaccinated (8). Parents and persons who opt out of vaccination should be aware of the risk that this practice places upon their children and their community. Communities of persons who have not been vaccinated can make intensive measles-containment activities necessary (9).
ACIP also recommends that persons who work in medical facilities be vaccinated for measles (10). The Indiana outbreak, in which a hospital worker contracted measles, demonstrates the need for health-care facilities to be aware of the vaccination status of their workers and require written documentation of vaccination history.
The Indiana outbreak could have been prevented by adherence to long-standing ACIP recommendations calling for measles vaccination of 1) international travelers, 2) children, and 3) health-care workers. The serious illnesses that resulted from this outbreak and the size and scope of activities and resources required to contain it underscore the need to adhere to these recommendations to sustain elimination of measles in the United States.
Acknowledgments
This report is based, in part, on contributions by the Tippecanoe County Health Dept, Lafayette, Indiana; Immunology and Virology Laboratories, Epidemiology Resource Center, Immunization Program, Indiana State Dept of Health. Hamilton County General Health District, Cincinnati Health Dept, Ohio. Illinois Dept of Health.
References
(1.) Yip FY, Papania MJ, Redd SB. Measles outbreak epidemiology in the United States, 1993-2001. J Infect Dis 2004;189(Suppl 1):S54-60.
(2.) CDC. Epidemiology of measles--United States, 2001-2003. MMWR 2004;53:713-6.
(3.) World Health Organization. Measles: fact sheet no. 286. Geneva, Switzerland: World Health Organization; 2005. Available at http:// www.who.int/mediacentre/factsheets/fs286/en.
(4.) CDC. National, state, and urban area vaccination coverage among children aged 19-35 months United States, 2004. MMWR 2005;54:717-21.
(5.) Papania MJ, Seward JE Redd SB, Lievano E Harpaz R, Wharton M. Epidemiology of measles in the United States, 1997-2001. J Infect Dis 2004;189(Suppl l):S61-8.
(6.) World Health Organization. Measles reported cases. Geneva, Switzerland: World Health Organization; 2005. Available at http:// www.who.int/immunization_monitoring/en/globalsummary/ timeseries/tsincidencemea.htm.
(7.) CDC. Measles, mumps, and rubella--vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 1998;47 (No. RR-8).
(8.) Feikin D, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RF. Individual and community risks of measles and pertussis associated with personal exemptions to immunization. JAMA 2000;284:3145-50.
(9.) Dayan GH, Ortega-Sanchez IR, LeBaron CW, Quinlisk MP, Iowa Measles Response Team. The cost of containing one case of measles: the economic impact on the public health infrastructure--Iowa, 2004. Pediatrics 2005;116:e1-4.
(10.) CDC. Immunization of health-care workers: recommendations of the Advisory Committee on Immunization Practices (ACIP) and the Hospital Infection Control Practices Advisory Committee (HICPAC). MMWR 1997;46(No. RR-18).
Reported by: W Staggs, MS, C Graves, MD, D Ellsworth, MEd, R Teclaw, DVM, PhD, Indiana State Degt of Health. G Dayan, MD, S Redd, MD, C LeBarotz, MD, Epidemiology and Surveillance Div, National Immunization Program; A Parker, MSN, MPH, EIS Officer, CDC.
COPYRIGHT 2005 U.S. Government Printing Office
COPYRIGHT 2006 Gale Group