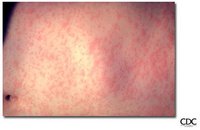
On March 12, 2004, a college student infectious with measles returned to Iowa from India by a commercial airliner (1); the case was subsequently linked to two other measles cases. This report updates information about this outbreak and provides details regarding vaccination, quarantine, and other measures used by Iowa public health authorities to interrupt disease transmission in a vulnerable population. The effective uses of quarantine and isolation during the outbreak underscore the utility of these public health tools in halting communicable disease transmission.
Immediately after being notified of the measles case, the Iowa Department of Public Health (IDPH) and local health departments in Iowa began using media releases, passenger lists, and interviews with the infected student to identify and contact persons potentially exposed to measles. Susceptible contacts (i.e., persons exposed and not fully vaccinated) were offered postexposure prophylaxis (PEP), either measles-mumps-rubella (MMR) vaccination within 72 hours of exposure or immune globulin (IG) within 6 days of exposure. Approximately 10 days later, measles cases were identified in two other Iowa residents: 1) a fellow airline passenger who previously had received two MMR vaccinations and 2) an unvaccinated close contact who had received postexposure MMR vaccination approximately 26 hours after contact with the first patient. Contacts of these two patients also were identified and offered PEP if they were deemed susceptible to measles infection. In public health immunization clinics specifically organized to vaccinate persons who had been exposed to measles, approximately 175 persons received postexposure MMR vaccination, and 20 received postexposure IG.
All three patients, who were moderately ill, were placed in voluntary isolation, which IDPH and local health departments monitored with home visits and telephone calls. Two susceptible health-care workers, who were exposed when the second patient sought medical care and who did not receive PEP within the recommended period, were placed in voluntary quarantine for 2 weeks, during which they did not leave their homes.
Two of the three measles patients were part of an insular community (estimated population: 2,000-3,000) with low vaccination rates (i.e., the community's K-12 school had a vaccination rate of 59% for vaccines required for school entry, including MMR). Community members held daily gatherings that provided opportunities for measles transmission to susceptible persons. PEP was offered to all susceptible persons in the community, and 56 accepted. Seven persons who had potentially been exposed to measles refused PEP, even though they were aware of the potential for being quarantined. Initially, all seven agreed to be quarantined in lieu of receiving vaccine, but because of their subsequent unwillingness to comply with voluntary quarantine, all seven were served by the local public health nurse with state-issued involuntary home quarantine orders, some with the assistance of local law enforcement officers. (Examples of Iowa's quarantine orders are available at http://www.idph.state.ia.us/adper/cade.asp.) Although none reported a history of full vaccination or symptomatic measles, within days of being quarantined, four of the seven were determined serologically to be immune and were released from quarantine; the other three completed their 2-week quarantine.
IDPH and the local health department monitored compliance with quarantine orders with at least daily unannounced home visits or telephone calls and released the persons from quarantine via oral communication. In the future, because of confusion about the exact time of day the quarantine should end, written release-from-quarantine notices will be served. No known breaks in quarantine occurred. None of those persons in quarantine acquired measles. No additional cases were reported.
Editorial Note: Use of vaccination, both pre- and postexposure, is the most common and preferred strategy for preventing transmission of measles (2). During this outbreak, Iowa public health officials first offered timely postexposure vaccination to susceptible persons who had close contact with a person infected with measles. However, when postexposure vaccination was refused, quarantine was used to reduce the risk of further transmission of measles to a vulnerable population.
An essential public health tool, rarely used in the last half century in the United States, quarantine is often confused with isolation, which is the restriction of movement of persons who are known to be infected with a communicable disease and who often are symptomatic. Quarantine reduces the risk of exposure to disease by separating and restricting the movement of persons who are not yet ill but who have been exposed to an infectious agent and might become infectious. Quarantine is more difficult to implement than isolation because the persons under quarantine are not symptomatic and thus have greater difficulty understanding the need for staying at home when compared with ill persons who need to be isolated.
Before antibiotics and vaccines, quarantine was used when direct medical countermeasures were not routinely available. However, quarantine often was implemented in a manner that equated disease with crime; consequently, quarantine acquired negative connotations associated with stigma and discrimination. For quarantine to be an effective and acceptable public health tool, these negative connotations must be overcome by applying the measure equally and fairly among all persons who have been exposed, and by using other approaches. These include providing education about the rationale for using quarantine; offering acceptable alternatives to quarantine, when feasible, such as postexposure vaccination or obtaining serologic proof of immunity; and applying due process measures, such as written notice and opportunities to appeal.
The use of quarantine to address public health problems demands a balancing of individual civil liberties with the collective needs of the public's health. Additional focus on the health, welfare, and social needs of persons subjected to quarantine is required. During the 2003 epidemic of severe acute respiratory syndrome (SARS), CDC listed 10 principles for modern quarantine (Box 1) (3,4).
BOX 1. Ten principles of modern quarantine
Modern quarantine is a collective action for the common good predicated on aiding persons infected or exposed to infectious agents while protecting others from the dangers of inadvertent exposure.
1. Used when exposed to highly dangerous and contagious diseases, when resources are available to implement and maintain, and when less restrictive means cannot accomplish the public health objectives.
2. Encompasses a wide range of strategies, from passive self-monitoring for symptoms to use of barriers limiting entry and exit to authorized persons.
3. Used in combination with other interventions and countermeasures to ensure that persons in quarantine or isolation are among the first to receive all supportive interventions available.
4. Ensures rapid isolation of infectious persons and separation from those merely exposed.
5. Lasts only as long as necessary to achieve epidemic control but no longer than the disease incubation period.
6. Does not have to be absolute to be effective; therefore, favors voluntary over compulsory approaches.
7. More likely to involve limited numbers of exposed persons in small areas than in a widespread geographic locale.
8. Requires clear understanding of the roles of jurisdictions and legal authorities.
9. Requires coordination and planning with multiple partners.
10. Requires education, trust, and participation of the general public.
In the United States, as in most countries of the world, government has the duty and legal power to address risks associated with persons whose freedom of movement might endanger the public's health. Under circumstances described in federal statute *, the U.S. government has the authority to detain persons for the control of communicable diseases. In particular, the U.S. government has the authority to isolate and quarantine persons to control the spread of selected communicable diseases specified by presidential executive order (5,6). In addition, all 50 states and the District of Columbia have the authority to detain persons under their own quarantine laws. In the event of an epidemic resulting from natural transmission or from deliberate introduction, both state and federal quarantine laws could be invoked to stem the spread of disease.
After the events of September 11, 2001, and in response to the draft Model State Emergency Health Powers Act (7), Iowa lawmakers reviewed the state's legal authority for public health emergency preparedness and response. In 2003, as a result of this review, the Iowa state legislature enacted new laws related to public health disaster preparedness. The new legislation included a provision authorizing IDPH to order quarantine in the event of a public health disaster ([dagger]). To implement this legislation and preexisting laws authorizing quarantine in nondisaster situations, IDPH adopted administrative rules governing the quarantine process. These rules became effective on March 10, 2004, only 2 days before the measles-infected student returned home to Iowa. Although the measles outbreak did not constitute a public health disaster under the 2003 statute, the state used the new quarantine process as outlined in its administrative rules to assist in containing the outbreak.
In 2003, the SARS outbreak triggered the widest use of quarantine globally since the influenza pandemic of 1917. Largely voluntary quarantine was used in Canada to keep approximately 20,000 persons in their homes for 10 days (8). For 27 persons who refused voluntary quarantine, public health officials issued legally enforceable quarantine orders. In certain cities in Asia (e.g., Beijing, Hong Kong, Singapore, and Taipei), quarantine authority was used to order thousands of persons to remain in their homes, an intervention that has been credited with helping to contain the outbreak (3). Although SARS did not spread within the United States, certain jurisdictions used quarantine authority to minimize the risk of spreading the virus (e.g., via unprotected health-care workers exposed to infectious SARS patients).
The scope and specifics of laws authorizing quarantine vary substantially by state. States that have not reviewed their quarantine laws might consider doing so by using a systematic approach covering essential features (e.g., quarantine, jurisdictional aspects, and due process) (Box 2). State and local health officials also might consider reviewing quarantine-related laws with their agencies' legal counsels, in coordination with law enforcement officials and the judiciary.
BOX 2. Essential questions to review regarding quarantine authority
Quarantine authority
* Who may declare a quarantine?
* Does a list of specific diseases exist for which a person can be quarantined?
* What is the process of initiating a quarantine?
* What is the penalty for violating a quarantine?
* How is the quarantine enforced?
* Is area quarantine authorized by law?
* Is group quarantine authorized by law?
Jurisdictional considerations
* Does the law clarify the relation between state and local jurisdictions in quarantine situations?
* Does the law clarify the coordination of quarantine authority among local jurisdictions?
* Does the law place any restrictions on coordination of quarantine authority between this state and the federal government?
Due process considerations
* What legal provisions exist for notice, hearing, consolidation of petitions, and legal representation?
* What provisions address confidentiality?
* Does the law contain any provisions addressing the use of habeas corpus?
* 42 U.S.C. [section] 264.
([dagger]) Iowa Code section 135.144 (2003 Suppl.), 139A.4, 139A.9, and 641 Iowa Administrative Code chapter 1.
References
(1.) CDC. Imported measles case associated with nonmedical vaccine exemption--Iowa, March 2004. MMWR 2004;53:244-6.
(2.) Heymann DL, ed. Control of communicable diseases manual. 18th ed. Washington, DC: American Public Health Association; 2004:353.
(3.) Cetron M, Maloney S, Koppaka R, Simone P. Isolation and quarantine: containment strategies for SARS 2003. SARS: emergence, detection, and response. In: Knobler S, Mahmoud A, Lemon S, Mack A, Sivitz L, Oberholtzer K, eds. Learning from SARS: preparing for the next disease outbreak--workshop summary. Washington, DC: National Academies Press; 2004:71-83.
(4.) CDC. Public health guidance for community level preparedness and response to severe acute respiratory syndrome (SARS). Atlanta, GA: US Department of Health and Human Services, CDC; 2004. Available at http://www.cdc.gov/ncidod/sars/guidance/index.htm.
(5.) Executive Office of the President. Executive Order 13295: revised list of quarantinable communicable diseases. Federal Register 2003;68: 17255. Available at http://www.cdc.gov/ncidod/sars/executiveorder040403.htm.
(6.) CDC. Questions and answers on legal authorities for isolation and quarantine. Atlanta, GA: US Department of Health and Human Services, CDC; 2004. Available at http://www.cdc.gov/ncidod/sars/quarantine qa.htm.
(7.) Gostin LO, Sapsin JW, Teret SP, et al. The Model State Emergency Health Powers Act: planning for and response to bioterrorism and naturally occurring infectious diseases. JAMA 2002;288:622-8.
(8.) Svoboda T, Henry B, Shulman L, et al. Public health measures to control the spread of the severe acute respiratory syndrome during the outbreak in Toronto. N Engl J Med 2004;350:2352-61.
Reported by: V McKeever, Jefferson County Public Health, Iowa; H Adams, JD, Office of the Iowa Attorney General; T Thornton, P Quinlisk, MD, Iowa Dept of Public Health. M Cetron, MD, Div of Global Migration and Quarantine, National Center for Infectious Diseases; R Goodman, MD, JD, F Shaw, MD, JD, A Moulton, PhD, Public Health Law Program, Office of the Chief of Public Health Practice; M Papania, MD, National Immunization Program, CDC.
COPYRIGHT 2004 U.S. Government Printing Office
COPYRIGHT 2004 Gale Group