Meningitis
Meningitis is inflammation of the membranes (meninges) covering the brain and the spinal cord. Although the most common causes are infection (bacterial, viral, fungal or parasitic), chemical agents and even tumor cells may cause meningitis. Meningitis can produce a wide range of symptoms including fever, headache or confusion and in extreme cases, deafness, brain damage, stroke, seizures or even death. Encephalitis and brain abscess can complicate infective meningitis. more...
Features
The classical symptoms of meningitis are headache, neck stiffness and photophobia (the trio are called "meningism"). Fever and chills are often present, along with myalgia. An altered state of consciousness or other neurological deficits may be present depending on the severity of the disease. In meningococcal meningitis or septicaemia, a petechial rash may appear. A lumbar puncture to obtain cerebrospinal fluid (CSF) is usually indicated to determine the cause and direct appropriate treatment.
Convulsions are a known complication of meningitis and are treated with appropriate anti-seizure drugs such as phenytoin.
Diagnosis
Most important in the diagnosis of meningitis is examination of the cerebrospinal fluid. A lumbar puncture should be performed promptly whenever the diagnosis of meningitis is suspected. The opening pressure is recorded and the cerebrospinal fluid sample is taken for microscopic examination (complete blood count with differential), chemical analysis (glucose and protein) and microbiology (gram staining and bacterial cultures).
In patients with focal neurological deficits or signs of increased intracranial pressure, a CT scan of the head should be obtained to help determine if there is a raised intracranial pressure that might cause a serious or fatal brain herniation during lumbar puncture. In the absence of these signs, a CT scan is unnecessary and should not delay lumbar puncture and initiation of antibiotic therapy.
Pathophysiology
Meningitis and encephalitis are usually caused by viruses or bacteria. Most often, the body’s immune system is able to contain and defeat an infection. But if the infection passes into the blood stream and then into the cerebrospinal fluid that surrounds the brain and spinal cord, it can affect the nerves and travel to the brain and/or surrounding membranes, causing inflammation. This swelling can harm or destroy nerve cells and cause bleeding in the brain.
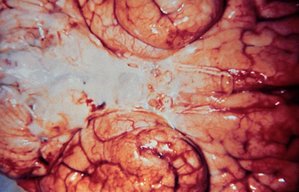
Pathology
Purulent (suppurative) leptomeningitis is a diffuse purulent inflammation. The leptomeninges (arachnoida and piamater) contain purulent exudate (pus): leukocytes (neutrophils), fibrin, germs, proteins, necrotic debris. Blood vessels in the subarachnoidian space and those intracerebral are congested and neutrophil margination is present.
Causes
Infectious
- G020: Viruses are the most common cause of meningitis.
- G00-G01: Major bacteria that cause Bacterial meningitis are Neisseria meningitidis (meningococcus), Streptococcus pneumoniae (pneumococcus), and Haemophilus influenzae. Less-common bacterial causes include Listeria monocytogenes, Staphylococcus and Escherichia coli. In developing countries, Mycobacterium tuberculosis is a common cause of bacterial meningitis. Streptococcus agalactiae is an important cause of neonatal meningitis associated with a high mortality rate.
- G021:In immunocompromised patients, fungal meningitis may occur, typically caused by Cryptococcus neoformans.
Read more at Wikipedia.org