A 72-year-old man presented with acute pulmonary edema after having had fever and constitutional symptoms for one week. He was found to have severe mitral regurgitation associated with a ruptured mitral chord and infective endocarditis. The patient required medical treatment and subsequent mitral valve surgery.
A 32-year-old woman presented with palpitations and atypical chest pain. She had multiple systolic clicks on auscultation of the heart. Both of these patients had a diagnosis of mitral valve prolapse, but do they have the same disease?
The diagnosis of mitral valve prolapse is the most common valve diagnosis in primary care practice. Since its first description by Barlow and colleagues(1) in 1966, this disease entity has generated more than 4,000 scientific articles describing its high prevalence and a number of associated complications. In the echocardiographic literature, mitral valve prolapse was diagnosed in almost one third of young women, which would suggest that it is a normal variant. Yet mitral valve prolapse has been associated with complications such as cerebral embolic events, infective endocarditis, severe mitral regurgitation requiring mitral valve surgery and even sudden death. Mitral valve prolapse, a common entity linked with devastating complications, has caused much alarm and anxiety in patients and physicians alike.(2-4)
Fortunately, advances in our knowledge of the diagnosis and natural history of mitral valve prolapse have occurred in the past few decades. These advances have resulted in a more pragmatic view of this condition. First, it is now understood that the term "mitral valve prolapse" does not constitute a single disease entity but encompasses a wide spectrum of processes.(3,5,6)
At the far end of the spectrum, patients may have the true disease of mitral valve prolapse, with thickened, redundant, floppy mitral valve leaflets and myxomatous proliferation. These patients are usually older men or persons with connective tissue disease who are at risk for severe mitral regurgitation, chordal rupture, infective endocarditis and sudden death. At the other end of the spectrum, however, are younger patients with normal mitral valve morphology whose mitral valve "bows" into the left atrium during systole, associated with a systolic click on auscultation and meeting the echocardiographic criteria for prolapse. These patients should be considered "normal variants," for they are not at higher risk for complications.
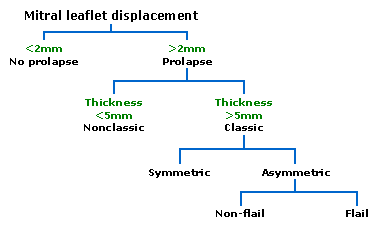
Secondly, problems with the echocardiographic diagnosis of mitral valve prolapse have occurred.(7) When two-dimensional echocardiography became widely utilized, the number of patients who were given the diagnosis of mitral valve prolapse became quite high, approaching almost 30 percent in young, otherwise healthy women.(8) These diagnoses were based on the appearance of the mitral valve in certain views, "bowing" into the left atrium. It has been subsequently established that the normal mitral annulus is shaped like a saddle, so the mitral valve leaflets in normal persons will appear to bulge into the left atrium on certain image views. Thus, the criteria for mitral valve prolapse on echocardiography should be a systolic displacement of at least 2 mm of one or both leaflets into the left atrium, and this should be visible in views other than the apical four-chamber view. By re-establishing the criteria for mitral valve prolapse on this basis of this knowledge, the prevalence of mitral valve prolapse becomes less than 3 percent of the general population.(9)
Mitral valve prolapse has been implicated as an etiology of other medical problems such as atypical chest pain, chronic fatigue disorder, anxiety with panic attacks and manic-depressive syndromes. As noted in the review by Bouknight and O'Rourke in this issue,(9) the association of common symptom complexes with the frequent diagnosis of mitral valve prolapse may be associated more with chance than a cause-and-effect relationship. Mitral valve prolapse has been associated with unexplained cerebroembolic events.(10) This association was based on case control studies in which the prevalence of mitral valve prolapse was determined in patients with a specific presenting complaint and compared with patients who did not have that complaint. In a recent study(11) using the new echocardiographic criteria for mitral valve prolapse, no relationship was identified between unexplained cerebroembolic events and the diagnosis of mitral valve prolapse. Thus, a search for the diagnosis of mitral valve prolapse to account for many of these presenting symptom complexes is not warranted.
Alternatively, patients who present with a loud holosystolic murmur of mitral regurgitation and the diagnosis of mitral valve prolapse should have a comprehensive cardiovascular evaluation. Longstanding mitral regurgitation creates a volume overload on the left ventricle, which eventually can lead to left ventricular systolic dysfunction and heart failure. Once the latter occur, the patient's outlook is poor. In some surgical institutions, it is now possible to perform valve repair rather than valve replacement in selected patients with mitral valve prolapse. This possibility has led some medical centers to recommend early, aggressive surgical intervention, even before the onset of symptoms. It is hoped that this strategy will prevent the problems associated with long-term volume overload and cardiac decompensation.(7)
Our approach to patients with the diagnosis of mitral valve prolapse has undergone significant change. The diagnosis of mitral valve prolapse should be based on the findings of a careful clinical examination, which is discussed in the article by Bouknight and O'Rourke.9 Echocardiography should be performed to confirm this diagnosis, using the newer echocardiographic criteria mentioned above. The echocardiographic report should also describe the morphology of the mitral valve apparatus so that the clinician can determine if a true pathologic disease is present or if this represents a normal variant.
Prophylaxis for infective endocarditis is warranted only in those patients with the true disease of thickened redundant mitral leaflets, mitral regurgitation, or both.(7) In the absence of clinical findings, echocardiography should not be performed to search for a diagnosis to account for symptoms such as anxiety attacks, atypical chest pain and chronic fatigue syndromes. Using this approach, many patients given the label of the "disease" of mitral valve prolapse may be reassured that they have a normal variant and an excellent prognosis for the future. It is to be hoped that with this information, the challenge of mitral valve prolapse may be resolved in the practice of medicine.
Dr. Nishimura is a professor of medicine at the Mayo Medical School and a consultant in cardiovascular medicine in the Division of Cardiovascular Diseases and Internal Medicine at the Mayo Clinic and Foundation, Rochester, Minn. Dr. Kidd is a family physician at the Whitewater Family Practice Clinic, Whitewater, Wis.
Address correspondence to R.A. Nishimura, M.D., Mayo Clinic, 200 First St., SW, Rochester, MN 55905.
REFERENCES
(1.) Barlow JB, Bosman CK. Aneurysmal protrusion of the posterior leaflet of the mitral valve. An auscultatory-electrocardiographic syndrome. Am Heart J 1966;71:166-78.
(2.) Wigle ED, Rakowski H, Ranganathan N, Silver MC. Mitral valve prolapse. Annu Rev Med 1976;27:165-80.
(3.) Nishimura RA, McGoon MD. Perspectives on mitral-valve prolapse. N Engl J Med 1999;341:48-50.
(4.) Leatham A, Brigden W. Mild mitral regurgitation and the mitral prolapse fiasco. Am Heart J 1980;99:659-64.
(5.) Nishimura RA, McGoon MD, Shub C, Miller FA Jr, Ilstrup DM, Tajik AK. Echocardiographically documented mitral-valve prolapse. Long-term follow-up of 237 patients. N Engl J Med 1985;313:1305-9.
(6.) Marks AR, Choong CY, Sanfilippo AJ, Ferre M, Weyman AE. Identification of high-risk and low-risk subgroups of patients with mitral-valve prolapse. N Engl J Med 1989;320:1031-6.
(7.) Bonow RO, Carabello B, de Leon AC, Edmunds LH Jr, Fedderly BJ, Freed MD, et al. ACC/AHA guidelines for the management of patients with valvular heart disease. Executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients With Valvular Heart Disease). J Heart Valve Dis 1998;7:672-707.
(8.) Freed LA, Levy D, Levine RA, Larson MG, Evans JC, Fuller DL, et al. Prevalence and clinical outcome of mitral-valve prolapse. N Engl J Med 1999;341:1-7.
(9.) Bouknight DP, O'Rourke RA. Current management of mitral valve prolapse. Am Fam Physician 2000; 61:3343-50,3353-4.
(10.) Barnett HJ, Boughner DR, Taylor DW, Cooper PE, Kostuk WJ, Nichol PM. Further evidence relating mitral-valve prolapse to cerebral ischemic events. N Engl J Med 1980;302:139-44.
(11.) Gilon D, Buonanno FS, Joffe MM, Leavitt M, Marshall JE, Kistler JP, Levine RA. Lack of evidence of an association between mitral-valve prolapse and stroke in young patients. N Engl J Med 1999;341:8-13.
COPYRIGHT 2000 American Academy of Family Physicians
COPYRIGHT 2000 Gale Group