When is a cardiac patient's abnormality perfectly normal after all?
MRS. LOPEZ, BARELY 30 AND clearly in good physical condition, would not be put off. "The pain starts here," she said, pointing to the left of her breastbone, "where it shoots down my left hand and spreads like fire up my neck. I can't catch my breath. My heart goes boom-boom-boom all the time. It keeps getting worse. I've tried everything."
Her EKG was flat-out normal, and I held the tracing up for her to see.
"You're perfect," I announced. "And to my ears, your heart sounds normal."
"But I have mitral valve prolapse," she shot back.
"Mrs. Lopez," I said, "these days everyone has mitral valve prolapse."
Although only an inch or so wide, the mitral valve takes a constant beating. Its job is to let blood from the heart's left atrium flow into the left ventricle--without letting any leak back into the atrium. That's not easy The left ventricle contracts with so much force that, if the head were not in the way, it would squirt a fountain of blood about five feet high. To do its job right, the mitral valve must close tightly enough to keep the blood from rushing back into the left atrium during the left ventricle's contraction.
"Mrs. Lopez," I said, "do you ever feel tingling in your hands, sudden fatigue, or a sense of panic sometimes?"
"Yes," she said. "How did you know?"
"Because we see at least half a dozen cases like yours every day Many people have also been told they have mitral valve prolapse. But all it means is that one of your heart valves is different from some other people's. It does not mean your valve is abnormal, nor that your symptoms are necessarily related to your valve."
She didn't believe me.
"Some studies have found that up to 30 percent of young women have mitral valve prolapse," I added. "How can all these people be abnormal?"
"But the brother of a friend of mine ... I think he had what I have, and he dropped dead!"
"Did he have mitral valve prolapse?"
"I'm not sure."
"Where were your tests done?"
"Here."
"Let me pull your chart then. Maybe I can show you what they saw and ex. plain why there isn't a problem." The mitral valve takes its name from the shape of a bishop's miter. It has two flaps, made of endothelium and connective tissue, which open and close. Sometimes a strep infection can trigger an autoimmune assault that reduces these diaphanous flaps to calcified hulks. Before penicillin, rheumatic fever killed tens of thousands of young people a year and disabled many more. Doctors were all too familiar with the low rumbling murmur generated by blood tortuously flowing through a rheumatic valve. But the valve can produce a panoply of other hums, clicks, and whooshes. What did these sounds mean?
In 1917, America declared war on the Kaiser. More than a million young American men had to be cleared for combat. Doctors lined them up and listened to their hearts--and were shocked to find that one in 34 produced a rumbling sound called a heart murmur. Normal hearts, it was thought, were only supposed to go lub-dub, not lub-shoosb-dub. Turbulent blood flow, caused by narrowed or leaky valves, seemed the most logical explanation for the noise. But most of the men were healthy, with no history of rheumatic fever. So common were the murmurs that one of the leading clinicians of the time, Lewis Conner, declared that nine tenths of the murmurs detected in young adults were benign. Unless they were accompanied by such problems as an enlarged heart or poor exercise capacity, the murmurs in and of themselves were deemed meaningless noise, nothing more.
And there the question rested until the early 1960s, when researchers in South Africa took another look. Thanks to the advent of cardiac catheterization, doctors could see the heart valves in action. By threading a catheter through the femoral artery in the groin and pushing it up into the heart, they could squirt a radio-opaque dye into the heart that would illuminate the left ventricle's contours in X rays. They found that in some cases mitral murmurs and clicks were associated with too much stretching, even leaking, of the mitral valve's flaps. Instead of sealing shut against the ventricle's jet, the flaps tended to balloon back into the atrium.
A new condition was born: mitral valve prolapse. Soon it was cropping up everywhere. Cardiac referral centers started reporting dangerous heart arrhythmias, strokes, valve infections--even sudden death--in patients with mitral valve prolapse. Looking back, it's easy to see that the patients were highly preselected. Referred by their local doctors for serious cardiac symptoms, they could not be said to represent average people. But doctors were reluctant to ignore what seemed to be an alarming risk factor. At the same time, a quick and easy screening test came along: echocardiography While catheterizing a heart is expensive and sometimes risky, echocardiograms are a snap. Bounce sound waves off the heart, interpret the tracing, and you're done.
Enthusiastic echocardiographers started reporting prevalence rates of mitral valve prolapse of 10, 17, and 30 percent in studies of healthy young people. But no one had bothered to come up with a standard definition for diagnosing the condition. Most studies recruited no more than a few hundred patients. And, as one would expect from small studies, results were all over the map.
Most unscientific of all, a so-called mitral-valve-prolapse syndrome came into vogue. Many young people came to doctors complaining of tingling in the hands, anxiety, and shortness of breath. In the past diagnoses such as neurasthenia or hypoglycemia had been thrown at these ill-defined symptoms. Then the technical apparatus of echocardiograms provided a "hard" explanation. Yet just how a leaky valve causes all those symptoms remains a mystery Moreover, studies show that people with and without mitral valve prolapse suffer similar rates of palpitations and chest pain. But there is nothing more satisfying to doctors than an anatomic explanation for murky symptoms.
And what to do about the condition? The most common intervention is to prescribe antibiotics for patients undergoing such routine procedures as teeth cleaning. Bacteria released during these treatments can enter the bloodstream and infect a leaky valve. Thus the drugs can prevent endocarditis, infection of the heart lining and valves. But they are only necessary in the relatively few patients whose mitral valves are significantly thickened or leaky
Mrs. Lopez had been swept up in a tsunami of overdiagnosis. "Don't worry," we doctors say, clicking off our newest MRIS or echocardiograms, oblivious to the floodgates of panic we've just opened. "It's probably nothing."
Thirty minutes later, her chart came back. I flipped to the echo report. Her valves were normal in thickness and displayed barely a touch of prolapse. I pointed out a word to her: "mild." "Mrs. Lopez, there are lots of different kinds of heart problems. There is no such thing as a risk-free life, but I can assure you, your risk of dropping dead is very, very small. You know, doctors get carried away sometimes. We find little abnormalities and we don't know what they mean, but we want to be careful. Odd, tragic things happen sometimes, as with your friend's brother. We wish we could prevent them, so we cast wide nets. Unfortunately, lots of healthy people then get labeled as sick when they're not. You are not. It says so right here." I smiled reassuringly
To my great relief, she smiled back.
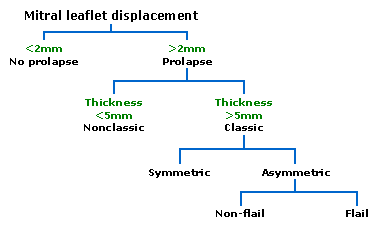
Four months later, the New England Journal of Medicine published a report on mitral valve prolapse. Armed with new, strict echocardiogram criteria, the authors had visited Framingham, Massachusetts--the site of a 51-year-old heart study--to look at 3,000 randomly selected townspeople. They found that the prevalence of definite prolapse (with severely thickened or billowing valve flaps) was only 2.4 percent.
But they also noted two more things. Depending on how the ultrasound beam is angled, one can "see" mitral valve prolapse in up to 50 percent of healthy people. Finally, they found that of all those with mitral-type murmurs, only about one in 10 had true prolapse. That distribution of risk mirrors what doctors had found in World War I. O
The case described in Vital Signs is based on a true story. Some details have been changed to protect the patient's privacy.
Tony Dajer has been a contributor to Vital Signs since 1989. He grew up in Puerto Rico and attended college and medical school in the United States. Dajer and his wife, an attorney, have three children, and the family alternates between living in France and in the United States. During the past five years, while the family home was in Paris, Dajer returned frequently for stints in the emergency room of New York University's Downtown Hospital. In August, the family moved back to the New York area. Dajer is at work on a book about medical mistakes.
COPYRIGHT 2000 Discover
COPYRIGHT 2000 Gale Group