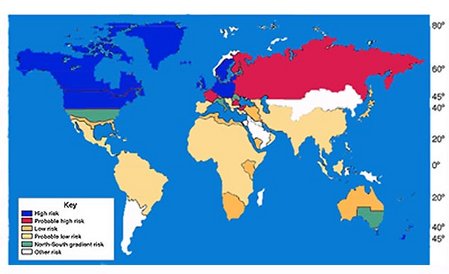
Multiple sclerosis (MS) is a chronic, often disabling disease of the central nervous system and is the most common cause of chronic neurological disability in young adults, affecting between 250,000 and 350,000 people living in the U.S. With an average age of 28 at the time of diagnosis, MS disrupts the careers of working-aged individuals, most commonly Caucasian women from northern European backgrounds. MS typically presents with a relapsing-remitting course. However, after a period of time averaging from five to 15 years, most experience a secondary progressive phase where the course changes to either a continuously progressing one or one that progresses between exacerbations (Polman & Uitdehaag, 2000).
MS occurs through a process of progressive destruction of the "white" matter in the nervous system--the myelin sheath that protects the nerves and allows for uninterrupted transmission of nerve impulses. This progressive demyelinization is initially an inflammatory process that ultimately leads to the destruction of the nerve. The initial inflammation is called an "exacerbation" and can often be treated using medications to reduce the residual damage. MS is now thought to be an autoimmune disorder, which develops from a complex interaction of early exposure to multiple viruses and genetic vulnerability. MS is characterized by a variable and complex array of symptoms including physical, sensory, and cognitive changes. These symptoms may vary from day to day and can present challenging barriers to participating in employment (Boyden, 2000; Herndon, 2000).
Several important trends have emerged in the last decade, including changing medical management, closer examination of issues related to employment, and trends in health care systems. These trends necessitate that rehabilitation professionals revisit or update their knowledge. The purpose of this article is to provide an overview of published literature that is pertinent to the employment of people with MS.
Trends in Medical Management
The past decade has brought important changes in medical management of MS. From the perspective of the neurologist, disease management has changed "from nihilism to reasonable optimism" (Comi, Colombo, & Martinelli, 2000). This increased optimism is the result of two important trends. First, improvements in magnetic resonance imaging (MRI) techniques have led to a better understanding of the nature and course of the disease. Second, using drugs that became available during the past decade can alter the course of the disease.
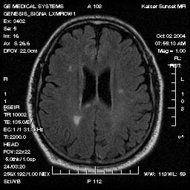
MRI as a Tool for Understanding MS
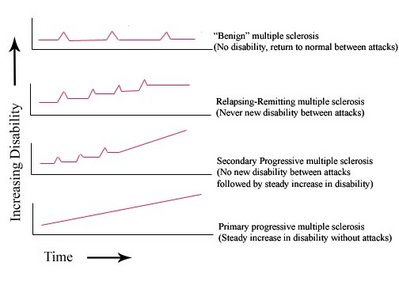
MRI involves the application of a powerful magnetic field to the body that causes cell nuclei to behave like tiny magnets. The signals are picked up by a very sensitive antenna and forwarded to a computer for processing. A variety of neuro-imaging methods are now available, which when taken together, provide a detailed understanding of the neuropathology associated with MS (Joy & Johnston, 2001). When first developed, MRI helped to identify sub-clinical lesions or lesions which had not yet resulted in apparent deficits leading to earlier diagnosis. More recently, MRI has been used to track changes in the brain over time and monitor the impact of drug treatment. Figure 1 illustrates the typical clinical course of relapsing-remitting and secondary progressive MS. Also noted are clinical and sub-clinical episodes of inflammation (exacerbations) along with the progression of axonal loss over time. Neuro-imaging techniques have allowed researchers to study how lesions evolve and resolve. They have also led to the appreciation that MS is not just a disease of myelin but that over time the brain atrophies and white cell matter between the lesions of MS may also be abnormal.
[FIGURE 1 OMITTED]
The correlation between conventional MRI and the functional status of an individual with MS has been described as "modest" (Miller, Grossman, Reingold, & McFarland, 1998). In research studies using MRI, areas of new lesions are often observed even when the individual under study is not experiencing any change in function and is considered to be in the remitting phase of the disease. These findings suggest a previously unsuspected level of activity and pathology throughout the course of the disease. In other words, the disease is active and progressive in a substantial number of individuals even during early stages of the disease when symptoms may be minimal. Miller and colleagues (1998) suggested several reasons for the lack of strong correlation between results of conventional MRI finding and level of functional disability, including problems with measurement error in quantifying MRI parameters; difficulty quantifying relapses; and the non-linearity of the Expanded Disability Status Scale (EDSS), a commonly used scale that measures both impairment and disability (Kurtzke, 1983). They (Miller et al, 1998) also suggested that MS is a very complex phenomenon in which specific aspects of the disability may not be simply or directly associated with underlying pathophysiology. Newer unconventional MRI strategies may provide a closer link between underlying pathology and clinical symptoms in MS (Matthews & Arnold, 2001).
The Emergence of Course-Altering Drugs
Until the last decade, drug management in MS has focused on relieving the symptoms of the disease, but not altering either the frequency of relapse or the rate of progression. In the 1990s, the term "disease-modifying therapy" began to emerge with the introduction of a number of drugs known as immunomodulatory agents, or the "ABC" drugs: Avonex[R], Betaseron[R], and Copaxone[R]. These drugs have been studied in carefully controlled clinical trials and have been shown to alter the clinical course of the disease by reducing the number and severity of attacks in individuals with relapsing-remitting MS (Comi, Colombo et al., 2000; Weinstock-Guttman & Jacobs, 2000). They have also been shown to alter disease features measured by MRI. When individuals taking the drugs are compared to controls, they have fewer new lesions, less brain atrophy, and reduced total burden of the disease.
The timing of intervention appears to be critical. Studies suggest the course-altering drugs are most effective in the early relapsing/remitting phase of the disease and are much less effective with progressive disease. There is a trend toward starting the drug early in an effort to prevent or reduce the early axonal damage that has been identified in MRI studies (Comi, 2000; Comi, Colombo et al., 2000). In a consensus statement, the U.S. National MS Society endorsed initiating pharmacological treatment as soon as a definite diagnosis of relapsing MS has been made ("US MS society urges early drug treatment," 1998).
Despite these encouraging advances, the drugs are costly and are not viewed as a cure for the disease. Researchers suggest that because of the heterogeneity of the myelin destruction process, no single agent will be sufficient to control the disease (Weinstock-Guttman & Jacobs, 2000). One of the medications requires self-injection, which limits the appeal for many. Side effects include flu-like symptoms (Gottber, Gardulf, & Fredrikson, 2000; Walther & Hohlfeld, 1999), and possible depression (Feinstein, 2000), which may also serve as barriers to use for some individuals.
Because it has been recognized for some time that MS disease activity is related to an autoimmune disease, medications used to suppress the proliferation of cells and cell products (antibodies) have been used to try to suppress disease (Edan, Miller, Clavet, Confavreaux, et at, 1997). Immunosuppressive drugs such as methotrexate, azathioprine, and cyclophosphamide are some of the oldest treatments for MS. In general, use of these medications has resulted in was some beneficial effects that are outweighed by negative side effects. The one exception is the more recently developed mitoxantrone (Novantrone) (Hartung, Gonsette, Konig, Kwiecinski, et al, 2002). This agent is a potent immunosuppresive medication effective in R-R and SP MS. However, it has a number of side effects including cardiotoxicity and generally cannot be used longer than a cumulative two, to two-and-a-half, lifetime years (Ghalie, Edan, Laurent, Mauch, et al, 2002).
Stem Cell Transplants
A promising new technique for the treatment of MS is autologous blood (haemopoietic) stem cell transplantation (HSCT) (Comi, Kappos et al., 2000; Kay, 2002). The technique involves destruction of the immune cells thought to be responsible for demyelenation of the nerve fibers, followed by transplantation of the patient's own haemopoietic stem cells that develop into new immune cells within days of transplantation (Kay, 2002). Reconstruction of the immune system in this way may result in permanent remission of the disease (Comi, Kappos et al., 2000). Previous studies have shown encouraging results with stabilization or improvement of symptoms and disease course in over 75% of patients who received HSCT (Fassas et al., 2000; Fassas et al., 1997). A new study at the University of Washington is showing similar results with over 75% of the patients showing a stabilized disease course after receiving the treatment (Kay, 2002). The technique is currently being tested only on patients with the most severe symptoms and who have not responded to conventional therapies for MS (Fassas et al., 2000; Fassas et al., 1997; Kay, 2002). Researchers anticipate that future studies of this treatment will include individuals with the progressive form of MS who are in earlier stages of the disease (Kay, 2002).
Wellness Approaches to Management
Maintaining healthy lifestyle habits, including healthy diet, adequate rest, relaxation, and other forms of self-regulation have a role in management of MS and can help individuals with MS to maintain maximum function despite the disease (Kraft & Catanzaro, 1996; Stuifbergen & Roberts, 1997). Research also indicates that exercise (Petajan et al., 1996; Ponichetera-Mulcare, 1993), communication/social support (Maybury & Brewin, 1984; Wineman, 1990), and coping with stress, particularly the stress of uncertainty (Murray, 1995), may facilitate overall health. Drugs have not been universally useful for MS fatigue, but have been of benefit to some that use them. Rest, sleep, positive experiences, sex, moderate exercise, relaxation, prayer, and cool water have all been reported to help with MS fatigue in the consumer literature (King, 1995). Moderate exercise improves strength, ability to perform common daily activities, and has a significantly positive impact on the physical and psychosocial well-being of individuals with MS (Kraft, Alquist, & de Lateur, 1996).
Changing Health Care Policies
Two important trends have emerged recently in the area of health care policy--the outcomes research movement and the new perspective on health and disablement spearheaded by the World Health Organization (WHO). Both of these trends are driven by a person-centered approach to health care.
The Outcomes Research Movements
The modern outcomes measurement movement began in the 1980s and reflects a need to document the benefits of health services. The measurement of outcomes is particularly important in chronic conditions such as MS where services cannot reasonably be expected to result in a "cure" of the condition. The movement shifted the focus of attention away from the disease and to the recipient of the service (Reiser, 1993). This consumer-based perspective is fundamental to the measurement of functioning, health status, and quality of life. The movement recognized that only an individual living with the condition could decide if a treatment was successful.
Both functional status and quality of life are considered "end results" of health services (Patrick & Chiang, 2000). Functional status usually focuses on observable activities and may or may not include the perspective of the person with a disability. In contrast, quality of life can only be judged by the individual experiencing the disease and includes contexts outside of health care. Researchers have developed hundreds of ways of measuring these constructs. Some scales apply generically across all populations while others are disease specific. The SF-36 is the most widely used generic measure of health status (McHorney, Ware, & Raczek, 1993). It contains 36 items in eight health dimensions: physical functioning, role limitations due to physical problems, bodily pain, general health perceptions, vitality, social functioning, role limitations due to emotional problems, and mental health.
As researchers study quality of life of individuals with MS, they find that the relationship between health status and quality of life is not a simple one (Ford, Gerry, Johnson, & Tennant, 2001). Although MS certainly has an impact on quality of life, poorer health status does not necessarily result in a poorer quality of life. This potential inconsistency has been called the disability paradox: Why do many people with serious and persistent disabilities report that they experience a good or excellent quality of life when to many external observers quality of life appears to be impaired (Albrecht & Devlieger, 1999)? One possible explanation of the disability paradox is that quality of life measures may reflect both adjustment to the disease and shifting of roles.
Trends in Employment
Employment Status and Its Impact on Society
Approximately 70% to 80% of people with MS are unemployed five years after diagnosis (O'Day, 1998). In spite of advances in the medical treatment of MS, the availability of adaptive technology, and the passage of the Americans with Disabilities Act ("Americans with Disabilities Act (ADA)," 1990), the unemployment rate of people with MS has remained high. Many people with MS retire prematurely and experience significant consequences with respect to quality of life, including financial security. A commonly reported pattern is to move from a higher-demand position held at the onset of symptoms to a position that places lesser demands on the individual, and then move to retirement or unemployment (Jackson, Quaal, & Reeves, 1991).
Premature retirement takes a significant economic toll on both the individual with MS and society (Hassink, 1993). Minden, Marder, Harrold, and Dor (1993) estimated the direct and indirect costs of MS in the U.S. and reported average lifetime losses at $495,845 per person with MS, and $1,500 for every American with a total impact on the national economy of $420 billion. Even though financial losses are considerable, financial difficulties are only some of the potential consequences of premature retirement. On average, people with MS who work consistently report higher quality of life, more effective social supports, and better perceived health when compared to people with MS with similar physical and cognitive impairments who no longer work (Kraft & Catanzaro, 1996).
More than 90% of people with MS have a history of employment (LaRocca & Hall, 1990) and 40% of people living with MS who are unemployed report that they would like to return to work (LaRocca, Kalb, Scheinberg, & Kendall, 1985). The reasons for this discrepancy between the desire to work and employment rate are multiple. In general, two types of barriers to finding and maintaining gainful employment interact: individual or personal barriers and societal or programmatic barriers. We reviewed both types of barriers briefly, followed by an overview of intervention programs that have been developed to address these barriers.
Individual or Personal Barriers to Employment
Individual or personal factors reside within the person with MS and include characteristics of the disease, such as the type and severity of symptoms, as well as a lack of education, and other well-documented reasons for unemployment (Beatty, Blanco, Wilbanks, & Paul, 1995). Individual factors clearly play a key role in reducing access to employment, and participants in various surveys of people living with MS have attributed their unemployment to a variety of functional limitations. The proportion of people who attribute their premature retirement to symptoms of MS ranges from 40% (Kornblith, LeRocca, & Baum, 1986) to 99% (Verdier-Taillefer et al., 1995). We review each of the most commonly reported symptoms of MS in the following section. It is important to note that these symptoms combine in numerous ways and influence each other in a very complex manner.
Fatigue. Fatigue has been recognized as one of the major issues for individuals living with MS (Bakshi et al., 2000; Ford, Trigwell, & Johnson, 1998; Freal, Kraft, & Coryell, 1984). The fatigue may be experienced differently by people with MS than people in general. Their fatigue may occur more quickly or even suddenly, more frequently, and more severely. For many, fatigue is chronic, and exacerbates other MS symptoms (Hubsky & Sears, 1992; Krupp, Alvarez, LaRocca, & Scheinberg, 1988). Sustained cognitive activity may also lead to fatigue and decreased cognitive performance (Krupp & Elkins, 2000). People living with MS may need assistance learning to manage fatigue, but rarely is the information on interventions for managing fatigue provided, and individuals must learn strategies by trial and error (Hubsky & Sears, 1992).
Changes in cognition and communication. Issues related to cognition and communication may play a more important role in explaining the unemployment rate among people with MS than had been previously thought (LaRocca, Kalb, & Gregg, 1996; Yorkston et al., 2001). Neurocognitive impairment in people with MS was evident in several areas, including verbal fluency, information processing speed, selected measures of memory, and cognitive flexibility (Zakzanis, 2000). Estimates of the proportion of individuals with MS experiencing cognitive difficulties vary depending on how estimates are made. Estimates of cognitive deficits that are based on conversation or simple screening examinations are not sensitive to subtle changes and may underestimate occurrence. Self-reports of a large group of individuals with MS indicated that 38% reported significant cognitive problems (Sullivan, Edgley, & Dehoux, 1990). When neuropsychological testing was used to estimate the occurrence of cognitive changes, prevalence rates ranged from 50% to 70% (Heaton, Nelson, Thompson, Burks, & Franklin, 1985; Rao, Leo, Bernardin, & Unverzagt, 1991).
Cognitive problems may interfere with employment, activities of daily living, communication, maintenance of social support, and quality of life (Foley et al., 1994; Gilchrist & Creed, 1994; Kujala, Portin, & Ruutiainen, 1996a, 1996b; Rao, Leo, Ellington et al., 1991). Beatty et al. (1995) compared people living with MS who were still working with those who had retired prematurely and found that people living with MS who were still working had fewer cognitive deficits, and concluded that cognitive impairment can be as or more disabling than the physical limitations people with MS experience. In their comparison of people classified as cognitively intact or impaired, Rao et al. (1991) found that while the groups were not differentiated based on physical disability and duration of illness, the group with cognitive impairments were more likely to be unemployed, socially isolated, and restricted in their activities of daily living.
Many people with MS experience difficulties with communication. A variety of communication disorders have been identified in individuals with MS including dysarthria, aphasia, and cognitive impairment affecting communication (Achiron et al., 1992; Arnett, Rao, Hussain, Swanson, & Hammeke, 1996; Kujala et al., 1996a; Lethlean & Murdoch, 1993; Olmas-Lau, Ginsberg, & Geller, 1977; Wallace & Holmes, 1993). Self-report questionnaires about communication difficulties associated with MS indicate that approximately 25% to 45% of the respondents noted changes in speech and/or communication (Beukelman, Kraft, & Freal, 1985; Hartelius & Svensson, 1994). Yorkston at al. (2001) reported that even when communication impairments were relatively mild, participation in life activities was greatly affected. Participants in the study also reported that both their communication ability and capacity to participate varied from day to day and felt that old communication strategies no longer worked well. Until recently, the literature has focused on dysarthria, a speech disorder that affects about half of individuals with MS (Yorkston, Beukelman, Strand, & Bell, 1999). Cognitive deficits associated with MS have been studied more extensively than communication deficits, and with a few notable exceptions (Foley et al., 1994; Wallace & Holmes, 1993), the impact of cognitive deficits on communication has not been studied.
Depression. Psychological distress, including depression, is more prevalent in individuals with MS than in the general public (Kraft, Freal, & Coryell, 1986; Patten & Metz, 1997; White, Catanzaro, & Kraft, 1993). The most commonly reported affective disturbance in MS is Major Depressive Disorder (MDD) (Rao, Huber, & Bornstein, 1992; Scott, Price, McConnell, & Land, 1996). MDD is a psychological disorder characterized by depressed mood or loss of interest or pleasure that is not directly caused by a general medical condition. It is associated with a variety of emotional and physical symptoms, such as weight loss or gain, insomnia or hypersomnia, psychomotor retardation or agitation, loss of energy and concentration, feelings of worthlessness and hopelessness, and thoughts of suicide or death. Studies estimate that MDD affects from 27% to 54% of individuals living with MS and the estimates of the lifetime prevalence of MDD range from 40% to 60% (Fassbender et al., 1998; Minden & Schiffer, 1990). This is in sharp contrast to the lifetime frequency of major depression of 9.7% in the general population (Wells, Golding, & Burnam, 1988), and other comparable disorders with similar levels of functional impairment (Minden & Schiffer, 1990; Rao et al., 1992; Schubert, 1993).
Many individuals with MS show mild to moderate psychological distress that does not meet full DSM-IV criteria for Major Depressive Disorder (Fassbender et al., 1998). Emotional distress may include subclinical levels of depressive symptoms, anxiety, psychosocial stress, and other mood complaints. The uncertain course of MS, as well as the effects of the disease on functioning, cognition, relationships, and work, likely contributes to psychological distress and difficulties in coping. Psychological distress, including depression, is often under-diagnosed and undertreated in MS (Minden, Orav, & Reich, 1987; Mohr, Goodkin, Likosky, Beutler et al., 1997; Mohr, Goodkin, Likosky, Gatto et al., 1997; Sullivan, Weinshenker, Mikail, & Edgley, 1995; White et al., 1993). It has been estimated that as many as 50% of those suffering depressive symptoms may go undetected during a standard MS medical evaluation (Sullivan et al., 1995).
Pain. MS-related chronic and acute pain is experienced by approximately 55% of people living with MS (Moulin, 1989; Moulin, Foley, & Ebers, 1988). Two-thirds of all people with MS experience MS-related chronic or acute pain sometimes during the course of the disease (Maloni, 2000). Several types of pain have been described, including facial pain, limb pain, musculoskeletal pain, and headache. Chronic pain has been commonly defined as any pain that persists longer than one month. Chronic pain does not appear to be related to the disease duration, degree of disability, depression, or cognitive deficits (Maloni, 2000; Stenager, Knudsen, & Jensen, 1991). Approximately 70% of all individuals living with MS who experience pain suffer from chronic pain. Pain is typically treated by medications. Many individuals also seek alternative therapies, such as acupuncture, transcutaneus electric nerve stimulation (TENS), massage, and dorsal column stimulation (Maloni, 2000). Other techniques, such as Tai Chi, meditation, hypnotherapy, and biofeedback may also increase quality of life and reduce pain (Dane, 1996; Maloni, 2000; Sutcher, 1997).
The effect of temperature on symptoms. Clinicians estimate that the incidence of heat intolerance might be as high as 80% (Guthrie & Nelson, 1995). In a survey conducted by Gulick (1989), participants listed warm temperatures among other conditions that impede their ability to work. Individuals with MS report that hot weather worsens their existing symptoms, contributes to the development of new signs and symptoms, and causes them to feel sluggish and exhausted (Freal et al., 1984; Guthrie & Nelson, 1995; Kraft & Alquist, 1996). Lowering of body temperature in individuals with temperature-sensitive MS symptoms appears to improve symptoms and overall functioning (Coyle, Krupp, Doscher, Deng, & Milazzo, 1995; Flesner & Lindencrona, 1999; Kraft & Alquist, 1996; Watson, 1959).
Bowel and bladder. Bladder dysfunction is one of the top five most prominent MS symptoms affecting overall quality of life as perceived by people with MS (Rothwell, McDowell, Wong, & Dorman, 1997). Approximately 5% of people with MS present with bladder dysfunction, and prevalence increases as the disease progresses. Joy and Johnston (2001) suggest that 90% of people with MS experience bladder dysfunction at some point; detrusor hyperreflexia, detrusor sphincter dyssynergia, and detrusor areflexia are the three most common types. The impact of this symptom on people with MS is generally severe and may be devastating, disrupting social, vocational, and sexual activities. Causes of the symptom are related to the stage of MS, location of MS lesions, and medications. Treatments for bladder dysfunction depend on the cause and severity of the symptom and include fluid intake monitoring, medications, pelvic muscle exercises, intermittent catheterization, indwelling catheter, and surgical intervention.
Bowel dysfunction in MS occurs less frequently than bladder dysfunction, affecting from 52% - 68% of people with MS (Chia et al., 1995; Hinds & Wald, 1989). This prevalence is much higher than that of the general population, and people with MS view bowel dysfunction as one of their most problematic symptoms (Rothwell et al., 1997). Because of its impact on the integrity of gastrointestinal function, bowel disturbance impairs critical physiologic processes such as the absorption of water, electrolytes, and nutrients during digestion. The most common symptoms associated with bowel dysfunction are constipation, seen in 50% of people with MS, and fecal incontinence, seen in 30%. Monitoring dietary intake, timed evacuation, adequate hydration, physical exercise, and avoiding chronic use of laxatives are all part of a good bowel program and are key to minimizing the negative impact of bowel dysfunction (Kraft, 1998b, 2000).
Limitations in mobility. Limitations in mobility due to weakness, fatigue, spasticity or ataxia are a significant concern for people with MS (Joy & Johnston, 2001; Rosenblum & Saffir, 1998). People typically describe loss of balance and/or coordination as the first signs of mobility problems. Ataxia may cause staggering, and cerebellar dysfunction may result in sudden losses of balance and frequent falls (Morrison, 1999). In addition, lower leg weakness can put undue stress on the back, causing additional strain and injury (Morrison, 1999). Difficulty walking or standing may present significant barriers in the workplace for people with MS (Joy & Johnston, 2001; Kraft, 1981). Many people who can walk short distances with little or no assistance require a scooter or wheelchair for ambulating longer distances (Kraft, 1998a). Therefore, aids and accommodations that minimize physical fatigue and disability at work are particularly important for people with MS (Joy & Johnston, 2001).
Numerous assistive technologies, including canes, walkers, orthotic devices, and specialized scooters or wheelchairs are available to help mitigate the impact of mobility difficulties on daily life and employment (Joy & Johnston, 2001; Kraft, 1981). Exercise and physical therapy have also been shown to have a positive impact on the coordination and mobility of people with MS (Kraft et al., 1996). Some medications such as clonazepam or hydroxyzine are helpful for controlling ataxia and spasticity, however, their use for motor disorders is limited due to side effects such as drowsiness and increased fatigue (Rosenblum & Saffir, 1998).
Spasticity. Spasticity and contractures are significant problems for people with MS (Kraft, 1981; LaBan, Martin, Pechur, & Sarnacki, 1998). Spasticity can prevent joints from moving through the normal range of motion and contribute to decreased mobility, increased fatigue, and problems maintaining employment (Kraft, 1981; LaBan et al., 1998). Severe spasticity may increase the probability of decubitus ulcers and bladder and bowel problems (Kraft, 1981; LaBan et al., 1998). Treatment of moderate spasticity may include physical therapy, stretching, exercise, and medications such as diazepam, dantrolene, clonidine, tizanidine and threonine (Kraft, 1998a; LaBan et al., 1998; Rosenblum & Saffir, 1998). However, elimination of spasticity is not necessarily recommended. For example, reducing rather than eliminating spasticity may help stabilize lower limbs and reduce disability (Kraft, 1998a). Severe spasticity may require implantation of a baclofen pump or surgical intervention (Kraft, 1998a; Rosenblum & Saffir, 1998).
In summary, physical and cognitive impairments and symptoms associated with MS have been repeatedly identified as significant barriers to full employment (Edgley, Sullivan, & Dehoux, 1991; Jongbloed, 1996; O'Day, 1998). More recently, the impact of cognitive and communication difficulties on employment has been recognized (LaRocca et al., 1996; Yorkston et al., 2001). Effective interventions must address the full range of functional limitations. In addition to providing interventions at the individual level, as a society we need to address barriers that reside outside of individuals with MS and are related to policies, attitudes, and knowledge about MS.
Societal and Programmatic Barriers to Employment
In the last decade, more studies have examined the role of societal and programmatic barriers to employment in MS. Societal factors, such as environmental barriers, attitudes of health care workers and the public, and a lack of accommodation in the workplace serve as significant barriers to employment for people living with MS (Roessler, 1996; Rumrill, 1996a, 1996b, 1996c; Rumrill, Steffen, & Kaleta, 1996).
Social attitudes. When people living with MS encounter difficulties at work, their support networks generally tend to discourage them from working (O'Day, 1998). Physicians may prescribe unemployment as a management strategy for fatigue or other MS-related symptoms (Rumrill, 1996a). Well-intentioned family members and employers also advise people with MS to leave employment as a way of dealing with issues of fatigue, pain, and stress. Considering the consequences of premature retirement and reduced participation in general, with respect to financial security, social interaction, health status, psychological adjustment, and quality of life, it may be far more beneficial to assist those individuals with MS who wish to continue employment with aggressive accommodation strategies than to counsel them to leave employment.
Financial and health care benefits. Financial difficulties are of significant concern to people living with MS, (Aronson, 1997) and decisions with respect to employment are frequently made based on valid concerns related to the fear of losing health care benefits, uncertainty of finding and maintaining stable employment, and ability to earn enough to cover disability-related expenses. Thus the current policies related to portability of health insurance, Medicare, Medicaid, and federal and personal long-term disability benefits may serve as powerful disincentives to return to employment (Johnson, 1984; Rumrill et al., 1996).
Workplace accommodations. Specific accommodations, including physical access to the workplace, working part-time, flexible work schedules, creating opportunities for intermittent rest, providing assistance with physically taxing duties, adaptive technology, sit-down jobs, and control over the pace of work have often not been available to people with MS (Jackson et al., 1991; Jongbloed, 1996; Kornblith et al., 1986; O'Day, 1998; Robinson, 2000). Workers with MS also report that employer attitudes toward employees with MS and misconceptions about MS on the part of co-workers affect their ability to remain employed (O'Day, 1998; Robinson, 2000). Often, co-workers and supervisors either do not understand the effects of the illness or fail to appropriately adjust work demands to match the abilities of the employee with MS (Robinson, 2000). A lack of knowledge about MS and negative attitudes on the part of employers often interact with the fact that many people living with MS are not aware of their rights to workplace accommodation, do not know what kinds of accommodations might be helpful, or request accommodations too late for them to be effective.
Project Alliance (Rumrill, 1996c) identified physical fatigue and cognitive impairment as the major reasons for job-related difficulties. Consequently, simple work site modifications or assistive technology may not be adequate to support maintenance or reentry to employment for a group with an incidence of neuropsychological impairment ranging between 43-65% (Rao, Leo, Bernardin et al., 1991). Additional support may be needed to assist people with MS with finding and maintaining employment. Despite the growing acknowledgment of the impact of cognitive impairment in MS, very little attention has been paid to developing and implementing cognitive rehabilitation interventions tailored specifically to MS (Prosiegel & Michael, 1993).
Vocational rehabilitation. Many people living with MS may also be eligible for services from the vocational rehabilitation system. Following enactment of the Rehabilitation Act of 1978, which required that people with severe disabilities receive priority for vocational rehabilitation services provided under the federal-state system, the National MS Society advocated for increased VR services to people with MS and entered into an agreement with the Rehabilitation Services Administration and the Council of State Administrators of Vocational Rehabilitation to increase access for people with MS. Evaluations over the next 10 years revealed that people with MS had been accepted for VR services at a higher rate (Kallos, Geneive, Struening, & Andrews, 1987). However, when Kraft at al. (1986) surveyed 656 individuals with MS, they found that respondents reported significant unmet needs with respect to counseling and vocational rehabilitation, and LaRocca and Hall (1990) reported that people with MS represented less than one percent of VR's successful case closures in 1984. According to the Rehabilitation Services Administration, people with MS accounted for fewer than 1/10th of 1% of all vocational rehabilitation closures nationally in 1999. One of the reasons for this may be that VR services are prioritized using criteria that include the severity of the person's disability, and symptoms of MS may not present severe functional limitations at any given point in time (Schapiro, 1994). In a qualitative study conducted by O'Day (1998), participants with MS reported that when they decided to pursue vocational rehabilitation they were denied services without thorough evaluation or were provided services in an untimely or inconsistent manner (O'Day, 1998).
Intervention Programs
It is the interaction between the individual and programmatic factors that contributes to work disability among people with MS. Successful interventions need to take into account the full range of functional limitations and programmatic barriers.
Considering the variety of symptoms that people with MS experience and the programmatic and societal forces that work against employment of people with MS, it is perhaps not surprising that intervention programs that sought to re-establish or maintain employment of people with MS have met with mixed results. Rumrill (1996) reviewed prior demonstration projects developed to improve work access for individuals with MS. These projects included MS Back to Work: the 1980 Operation Job Match; the 1983 Job Raising Program; the 1993 Return to Work Program; and the 1994 Career Possibilities Project (Rumrill et al., 1996). More recently, findings and recommendations from the multi-site Project Alliance (1996), a National Multiple Sclerosis Association project, have become available. The earlier Job Match program involved job-seeking skills training and an MS-specific job bank for matching job candidate to job. Later projects moved toward more job-seeking skills and job-search skills implementation with an increasing emphasis on group member empowerment strategies, placement planning, and strategizing accommodations for barrier removal with less emphasis on direct placement assistance. Most programs have targeted those who already are unemployed. The Job Raising Program (LaRocca & Hall, 1990) included a program for individuals with MS who were employed. Of those individuals with MS who were employed when they entered Job Raising, 87% either retained their jobs or obtained new jobs (Hall, 1990, 1991, 1992; LaRocca & Hall, 1990).
LaRocca et al. (1996) developed and implemented a medical-community job-retention model for people with MS who were at risk for losing their jobs. While the program ran well and the authors concluded that a combined medical-community job-retention program was feasible, the results were disappointing. The authors reported that people with MS did not generally take advantage of job-retention services until an employment crisis developed, and did not adopt a preventative attitude, preferring not to think about anticipating and heading off future problems. Suggestions for effective early intervention programs included the following: (a) providing information about the types of problems they may encounter in the future and providing information about the providers who can be of help when a crisis develops; and (b) making available practical programs of cognitive rehabilitation and counseling to help people deal with psychological problems, especially cognitive changes. Project Alliance (Rumrill, 1996c) took a pro-active stance in the vocational rehabilitation of adults with MS, i.e., to prevent job loss or resignation through early interventions, including negotiation with an employer and accommodation recommendations. Although most participants did not complete the entire intervention, among those who did, the job retention rate was approximately 80% (Rumrill, 1996c).
Conclusions and Recommendations
People with MS are healthier, more secure financially, more socially active, and report a higher perceived quality of life when they are employed. With the well-documented efficacy of course-altering medications and wellness approaches, people with MS in general can anticipate a more predictable and gradual decline in function with fewer exacerbations. Unfortunately, a high percentage of people with MS are unemployed. Some people may not be participating in employment for reasons independent of their MS, while for others, the primary barriers are related to their MS functional limitations. For many, it is likely that the interaction between functional limitations and psychosocial variables have resulted in reduced participation in employment. The attitudes of professionals interacting with people with MS may well contribute to excessive disability with respect to employment. For example, health care workers may not inquire about cognitive and/or fatigue limitations, or be familiar with accommodation strategies that address these limitations. They also may inaccurately equate employment with stress and recommend termination of employment. Employers may not appreciate the residual capacity to participate in employment and/or the complexity of MS. Vocational rehabilitation counselors may not understand the cognitive and fatigue limitations or have the knowledge and/or skill to develop aggressive, early accommodations to help preserve employment.
Implications for Practice
We noted that course altering medications provided early on, and aggressive management of exacerbations, have been found to slow the progression of MS and reduce the number of functional limitations experienced by people with MS. It is important that rehabilitation counselors and other professional assist their clients in obtaining the most current MS medical treatment. Early and aggressive medical management may delay the progression of physical and cognitive limitations and preserve the potential to continue or re-enter employment.
It is also critical that rehabilitation counselors understand the degree to which cognitive changes can be disabling in the workplace for people living with MS. When assistance with accommodations for cognitive changes is acceptable to the worker with MS, the rehabilitation counselor or professional will be most helpful if adequate neuropsychological data are available to inform the design of the accommodations. Accommodations may involve not only modification of the job, but re-structuring the engagement of tasks to allow for enhanced pacing, matching complex tasks with the times in the day when the employee feels fresher cognitively, managing the overall economy of energy, etc.
It appears that people with MS may move toward retirement or disengagement from employment prematurely. Providing counseling and other early interventions may be useful, although it is not clear from the literature how effective this will be.
Finally, for rehabilitation counselors and professionals to serve as effective advocates, they must stay abreast of the rapid changes in medical treatment of MS. For example, as the course altering medications move toward non-injectable administration, they may be palatable to a broader group of people living with MS.
Future Research
In addition to examining the effects of physical and cognitive impairments, and societal and programmatic factors on employment of people with MS, understanding the insider's perspective is particularly critical in the development of successful interventions for individuals with chronic disease. Failure to appreciate this viewpoint can interfere with the rehabilitation process (Yorkston et al., 2001). While large-scale surveys have been useful in outlining the type and extent of barriers to employment faced by people with MS, they cannot provide information about the more subtle barriers people with MS face and about their decision-making processes related to employment. Studies on employment and MS that have used qualitative research methodology, such as unstructured or semi-structured interviews, have provided informative and insightful descriptions and additional explanations of when, how, and why people living with MS typically make important decisions related to employment (Jongbloed, 1996; O'Day, 1998; Robinson, 2000). Further qualitative research is needed to understand more clearly the perspective of people with MS as they experience changes in function; make adaptations in their roles at home, in the community, and at work; and interact with employers, health care workers, vocational rehabilitation professionals, and others.
References
Achiron, A., Ziv, I., Djaldetti, R., Goldberg, H., Kuritzky, A., & Melamed, E. (1992). Aphasia in multiple sclerosis: Clinical and radiologic correlations. Neurology, 42(11), 2195-2197.
Albrecht, G. L., & Devlieger, P. J. (1999). The disability paradox: High quality of life against all odds. Social Science and Medicine, 48, 977-988.
Americans with Disabilities Act (ADA). (1990). 42 U.S.C. 12101-12213.
Arnett, P. A., Rao, S. M., Hussain, M., Swanson, S. J., & Hammeke, T. A. (1996). Conduction aphasia in multiple sclerosis: A case report with MRI findings. Neurology, 47(2), 576-578.
Aronson, K. J. (1997). Quality of life among persons with multiple sclerosis and their caregivers. Neurology, 48(1), 74-80.
Bakshi, R., Shaikh, A. S., Miletich, R. S., Czarnecki, D., Dmochowski, J., Henson, Janardhan, V., Dubey, N., & Kinkel, R. P. (2000). Fatigue in multiple sclerosis and its relationship to depression and neurologic disability. Multiple Sclerosis, 6(3), 181-185.
Beatty, W. W., Blanco, C. R., Wilbanks, S. L., & Paul, R. H. (1995). Demographic, clinical and cognitive characteristics of multiple sclerosis patients who continue to work. Journal of Neurologic Rehabilitation, 9(3), 167-173.
Beukelman, D. R., Kraft, G. H., & Freal, J. (1985). Expressive communication disorders in persons with multiple sclerosis: A survey. Archives of Physical Medicine and Rehabilitation, 66(10), 675-677.
Boyden, K. M. (2000). The pathophysiology of demyelination and the ionic basis of nerve conduction in multiple sclerosis: An overview. Journal of Neuroscience Nursing, 32(1), 49-53.
Classification Assessment Surveys and Terminology Team. (2001). ICIDH-2: International classification of functioning, disability and health: World Health Organization.
Chia, Y., Fowler, C. J., Kamm, M. A., Henry, M. M., Lemieux, M. C., & Swash, M. (1995). Prevalence of bowel dysfunction in patients with multiple sclerosis and bladder dysfunction. Journal of Neurology, 242, 105.
Comi, G. (2000). Why treat early multiple sclerosis patients? Current Opinion in Neurology, 13, 235-240.
Comi, G., Colombo, B., & Martinelli, V. (2000). Prognosis-modifying therapy in multiple sclerosis. Neurological Sciences, 21, S893-899.
Comi, G., Kappos, L., Clanet, M. G., Ebers, G., Fassas, A., Fazekas, F., Filippi, M., Hartung, H. P., Hertenstein, B., Karussis, D., Martino, G., Tyndall, A., van der Meche, F. g. A., & Group, B.-M. S. (2000). Guidelines for autologous blood and marrow stem cell transplantation in multiple sclerosis: A consensus report written on behalf of the European group for blood and marrow transplantation and the European Charcot Foundation. Journal of Neurology, 247, 376-382.
Compston, A., & Coles, A. (2002). Multiple sclerosis. The Lancet, 359(9313), 1221-1231.
Coyle, P. K., Krupp, L. B., Doscher, C., Deng, Z., & Milazzo, A. (1995). Clinical and immunological effects of cooling in multiple sclerosis. Annals of Neurology, 38, 312.
Dane, J. (1996). Hypnosis for pain and neuromuscular rehabilitation with multiple sclerosis. Case summary, literature review and analysis of outcomes. The International Journal Of Clinical And Experimental Hypnosis, 44(3), 208-231.
Devlieger, P. J. (1999). From handicap to disability: Language use and culture meaning in the united states. Disability and Rehabilitation, 21(7), 346-354.
Edan, G, Miller, D, Clanet, M, Confavreux, C, Lyon-Caen, O, Lubetzki, C, Brochet, B, Berry, I, Rolland, Y, Froment, J, Cabanis, E, Iba-Zizen, M, Gandon, J, Lai, H, Moseley, I, Sabouraud, O. (1997). Therapeutic effect of mitoxantrone combined with methylprednisolone in multiple sclerosis: a randomised multicentre study of active disease using MRI and clinical criteria. Journal of Neurosurgery, Neurology, and Psychiatry, 62(2), 112-118.
Edgley, K., Sullivan, M. J., & Dehoux, E. (1991). A survey of multiple sclerosis: Ii. Determinants of employment status. Canadian Journal of Rehabilitation, 4(3), 127-132.
Fassas, A., Anagnostopoulos, A., Kazis, A., Kapinas, K., Sakellari, I., Kimiskidis, V., Smias, C., Elefteriades, N., & Tsimourtou, V. (2000). Autologous stem cell transplantation in progressive mulitple sclerosis--an interim analysis of efficacy. Journal of Clinical Immunology, 20(1), 24-30.
Fassas, A., Anagnostopoulos, A., Kazis, A., Kapinas, K., Sakellari, I., Kimiskidis, V., & Tsompanakou, A. (1997). Peripheral blood stem cell transplantation in the treatment of progressive multiple sclerosis: First results of a pilot study. Bone Marrow Transplantation, 20, 631-638.
Fassbender, K., Schmidt, R., Mofsner, R., Kischka, U., Kuhnen, J., Schwartz, A., & Hennerici, M. (1998). Mood disorders and dysfunction of the hypothalamic-pituitary-adrenal axis in multiple sclerosis. Archives of Neurology, 55(1), 66-72.
Feinstein, A. (2000). Multiple sclerosis, disease modifying treatments and depression: A critical methodological review. Multiple Sclerosis, 6(343-348).
Flesner, G., & Lindencrona, C. (1999). The cooling-suit: A study of ten multiple sclerosis patients' experience in daily life. Journal of Advanced Nursing, 29(6), 1444-1453.
Foley, F. W., Dince, W. M., Bedell, J. R., LaRocca, N. G., Kalb, R., Caruso, L. S., Smith, C., & Shnek, Z. M. (1994). Psychoremediation of communication skills for cognitively impaired persons with multiple sclerosis. Journal of Neurologic Rehabilitation, 8(4), 165-176.
Ford, H., Trigwell, P., & Johnson, M. (1998). The nature of fatigue in multiple sclerosis. Journal of Psychosomatic Research, 45(1), 33-38.
Ford, H. L., Gerry, E., Johnson, M. H., & Tennant, A. (2001). Health status and quality of life of people with multiple sclerosis. Disability and Rehabilitation, 23(12), 516-521.
Frattali, C. (1998). Measuring outcomes in speech-language pathology. New York: Thieme Medical Publishers.
Freal, J. E., Kraft, G. H., & Coryell, J. K. (1984). Symptomatic fatigue in multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 65(3), 135-138.
Ghalie, R., Edan, G., Laurent, M., Mauch, E., Eisenman, S., Hartung, H., Gonsette, R., Butine, M., Goodkin, D. (2002). Cardiac adverse effects associated with mitoxantrone (Novantrone) therapy in patients with MS. Neurology, 59(6), 909-913.
Gilchrist, A. C., & Creed, F. H. (1994). Depression, cognitive impairment and social stress in multiple sclerosis. Journal of Psychosomatic Research, 38, 193-201.
Gottber, K., Gardulf, A., & Fredrikson, S. (2000). Interferon-beta treatment for patients with multiple sclerosis: The patient's perceptions of side-effects. Multiple Sclerosis, 6, 349-354.
Gulick, E. E., Yam, M., & Touw, M.M. (1989). Work performance by persons with multiple sclerosis: Conditions that impede or enable the performance of work. International Journal of Nursing Studies, 26(4), 301-311.
Guthrie, T. C., & Nelson, D. A. (1995). Influence of temperature changes on multiple sclerosis: Critical review of mechanisms and research potential. Journal of Neurological Science, 129(1), 1-8.
Hall, H. L. (1990). Multiple sclerosis intervention model: Final report. New York: National Multiple Sclerosis Society.
Hall, H. L. (1991). Report for NMSS services committee. New York: National Multiple Sclerosis Society.
Hall, H. L. (1992). Job raising program data update. New York: National Multiple Sclerosis Society.
Hartelius, L., & Svensson, P. (1994). Speech and swallowing symptoms associated with Parkinson's disease and multiple sclerosis: A survey. Folia Phoniatrica et Logopaedica, 46, 9-17.
Hartung, H., Gonsette, R., Konig, N., Kwiecinski, H., Guseo, A., Morrissey, S., Krapf, H., Zwingers, T. (2002). Mitoxantrone in progressive multiple sclerosis: a placebo-controlled, double-blind, randomised, multicentre trial. Lancet, 360(9350), 2018-2025.
Hassink, G., Manegold, U., & Poser, S. (1993). Early retirement and occupational rehabilitation of patients with multiple sclerosis. Rehabilitation, 32(2), 139-145.
Herndon, R. M. (2000). Pathology and pathophysiology. In J. S. Burkes & K. P. Johnson (Eds.), Multiple sclerosis: Diagnosis, medical management, and rehabilitation (pp. 35-45). New York: Demos.
Heaton, R. K., Nelson, L. M., Thompson, D. S., Burks, J. S., & Franklin, G. M. (1985). Neuropsychological findings in relapsing-remitting and chronic progressive multiple sclerosis. Journal of Consulting and Clinical Psychology, 53, 103-110.
Hinds, J. M., & Wald, A. (1989). Colonic and anorectal dysfunction associated with multiple sclerosis. American Journal of Gastroenterology, 84(6), 587.
Hubsky, E. P., & Sears, J. H. (1992). Fatigue in multiple sclerosis: Guidelines for nursing care. Rehabilitation Nursing, 17(4), 176-180.
Jackson, M. F., Quaal, C., & Reeves, M. A. (1991). Effects of multiple sclerosis on occupational and career patterns. Axon, 13(1), 16-17, 20-22.
Johnson, K. L. (1984). Incentives and disincentives in the vocational rehabilitation process. Washington, D.C.: National Institute for Handicapped Research.
Jongbloed, L. (1996). Factors influencing employment status of women with multiple sclerosis. Canadian Journal of Rehabilitation, 9, 213-222.
Joy, J. E., & Johnston, R. B. (Eds.). (2001). Multiple sclerosis: Current status and strategies for the future. Washington, D.C.: National Academy Press.
Kallos, J., Geneive, L., Struening, E., & Andrews, H. (1987). The role of advocacy groups in vocational rehabilitation service delivery to the severely disabled: A comparison between multiple sclerosis and other disorders. J Neurologic Rehabilitation, 2(1), 13-20.
Kay, L. (2002, April 17). Stem cell therapy may help multiple sclerosis. The Los Angeles Times.
King, M. (1995). Fatigue--a medical overview shows the many aspects of this problem. Inside MS, 13(3).
Kornblith, A. B., LeRocca, N. G., & Baum, H. M. (1986). Employment in individuals with multiple sclerosis. International Journal of Rehabilitation Research, 9(2), 155-165.
Kraft, G. H. (1981). Multiple sclerosis. In W. Stolov & M. Clowers (Eds.), Handbook of severe disability (pp. 111-118). Washington, D.C.: U.S. Department of Education.
Kraft, G. H. (1998a). Forward. In G. Kraft & R. S. Taylor (Eds.), Multiple sclerosis: A rehabilitative approach (Vol. 9, #3, pp. xi-xiii). Philadelphia: W. B. Saunders and Co.
Kraft, G. H. (1998b). Rehabilitation principles for patients with multiple sclerosis. The Journal of Spinal Cord Medicine, 21(2), 117-120.
Kraft, G. H. (2000). Rehabilitation still the only way to improve function in multiple sclerosis. The Lancet, 354, 2016.
Kraft, G. H., & Alquist, A. D. (1996). Effect of microclimate cooling on physical function in multiple sclerosis. Multiple Sclerosis: Clinical and Laboratory Research, 2(2), 114-115.
Kraft, G. H., Alquist, A. D., & de Lateur, B. J. (1996). Effect of resistive exercise on physical function in multiple sclerosis (ms). Veterans Affairs Rehabilitation Research and Development Progress Reports, 33(June), 328-329.
Kraft, G. H., & Catanzaro, M. L. (1996). Living with multiple sclerosis: A wellness approach. New York: Demos.
Kraft, G. H., Freal, J. E., & Coryell, J. K. (1986). Disability, disease duration, and rehabilitation service needs in multiple sclerosis: Patient perspectives. Archives of Physical Medicine and Rehabilitation, 67, 164-168.
Krupp, L. B., Alvarez, L. A., LaRocca, N. G., & Scheinberg, L. (1988). Fatigue in multiple sclerosis. Archives of Neurology, 45, 435-437.
Krupp, L. B., & Elkins, L. E. (2000). Fatigue and declines in cognitive functioning in multiple sclerosis. Neurology, 55(7).
Kujala, P., Portin, R., & Ruutiainen, J. (1996a). Language functions in incipient cognitive decline in multiple sclerosis. Journal of Neurological Sciences, 141, 79-86.
Kujala, P., Portin, R., & Ruutiainen, J. (1996b). Memory deficits and early cognitive deterioration in ms. Acta Neurologica Scandinavica, 93(5), 329-335.
Kurtzke, J. F. (1983). Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (edss). Neurology, 33, 1444-1452.
LaBan, M. M., Martin, T., Pechur, J., & Sarnacki, S. (1998). Physical and occupational therapy in the treatment of patients with multiple sclerosis. In G. H. Kraft & R. S. Taylor (Eds.), Multiple sclerosis: A rehabilitative approach (Vol. 9, #3, pp. 603-614). Philadelphia: W.B. Saunders.
LaRocca, N., & Hall, H. (1990). Multiple sclerosis program: A model for neuropsychiatric disorders. New Directions for Mental Health Services, 45, 49-64.
LaRocca, N., Kalb, R., & Gregg, K. (1996). A program to facilitate retention of employment among persons with multiple sclerosis. Work, 7, 37-46.
LaRocca, N., Kalb, R., Scheinberg, L., & Kendall, P. (1985). Factors associated with unemployment of patients with multiple sclerosis. Journal of Chronic Disease, 38(2), 203-210.
Lethlean, J. B., & Murdoch, B. E. (1993). Language problems in multiple sclerosis. Journal of Medical Speech/Language Pathology, 1(1), 47-59.
Maloni, H. W. (2000). Pain in multiple sclerosis: An overview of its nature and management. Journal of Neuroscience Nursing, 32(3), 139-152.
Matthews, P. M., & Arnold, D. L. (2001). Magnetic resonance imaging of multiple sclerosis: New insights linking pathology to clinical evolution. Current Opinion in Neurology, 14, 279-287.
Maybury, C., & Brewin, C. (1984). Social relationships, knowledge and adjustment to multiple sclerosis. Journal of Neurology, Neurosurgery, and Psychiatry, 47, 372-376.
McHorney, C. A., Ware, J. E., & Raczek, A. E. (1993). The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care, 31, 247-263.
Miller, D. H., Grossman, R. I., Reingold, S. C., & McFarland, H. F. (1998). The role of magnetic resonance techniques in understanding and managing multiple sclerosis. Brain, 121(Pt 1), 3-24.
Minden, S., Marder, W., Harrold, L., & Dor, A. (1993). Multiple sclerosis. A statistical portrait. Cambridge: Abt Associates Inc.
Minden, S. L., Orav, J., & Reich, P. (1987). Depression in multiple sclerosis. General Hospital Psychiatry., 9, 426-434.
Minden, S. L., & Schiffer, R. B. (1990). Affective disorders in multiple sclerosis: Review and recommendations for clinical research. Archives of Neurology, 47, 98-104.
Mohr, D. C., Goodkin, D. E., Likosky, W., Beutler, L., Gatto, N., & Langan, M. K. (1997). Identification of beck depression inventory items related to multiple sclerosis. Journal of Behavioral Medicine, 20(4), 407-414.
Mohr, D. C., Goodkin, D. E., Likosky, W., Gatto, N., Baumann, K. A., & Rudick, R. A. (1997). Treatment of depression improves adherence to interferon beta-1b therapy for multiple sclerosis. Archives of Neurology, 54(5), 531-533.
Morrison, W. (1999). Multiple sclerosis: An overview for nurses. Axon, March, 55-61.
Moulin, D. E. (1989). Pain in multiple sclerosis. Neurologic Clinics, 7(2), 321-330.
Moulin, D. E., Foley, K. M., & Ebers, G. C. (1988). Pain syndromes in multiple sclerosis. Neurology, 38, 1830-1834.
Murray, T. J. (1995). The psychosocial aspects of multiple sclerosis. Neurologic Clinics, 13(1), 197-223.
O'Day, B. (1998). Barriers for people with multiple sclerosis who want to work: A qualitative study. Journal of Neurological Rehabilitation, 12(3), 139-146.
Olmas-Lau, N., Ginsberg, M., & Geller, G. (1977). Aphasia in multiple sclerosis. Neurology, 27, 623-626.
Patrick, D. L., & Chiang, Y. P. (2000). Measurement of health outcomes in treatment effectiveness evaluations: Conceptual and methodological challenges. Medical Care, 38(9 Suppl), 1114-1125.
Patten, S. B., & Metz, L. M. (1997). Depression in multiple sclerosis. Psychotherapy and Psychosomomatics, 66, 286-292.
Petajan, J. H., Gappmaier, E., White, A. T., Spencer, M. D., Mino, L., & Hicks, R. W. (1996). Impact of aerobic training on fitness and quality of life in multiple sclerosis. Annals of Neurology, 39, 432-441.
Polman, C., & Uitdehaag, B. M. J. (2000). Drug treatment of multiple sclerosis. British Medical Journal, 321, 490-494.
Ponichetera-Mulcare, J. A. (1993). Exercise and multiple sclerosis. Medicine and Science in Sports and Exercise, 25, 451-465.
Prosiegel, M., & Michael, C. (1993). Neuropsychology and multiple sclerosis: Diagnostic and rehabilitative approaches. Journal of Neurological Sciences, 115 Suppl, S51-54.
Rao, S. M., Huber, S. J., & Bornstein, R. A. (1992). Emotional changes with multiple sclerosis and parkinson's disease. Journal of Consulting and Clinical Psychology, 60(3), 369-378.
Rao, S. M., Leo, G. J., Bernardin, L., & Unverzagt, F. (1991). Cognitive dysfunction in multiple sclerosis: I. Frequency, patterns and predictions. Neurology, 41, 658-691.
Rao, S. M., Leo, G. J., Ellington, L., Nauertz, T., Bernardin, L., & Unverzagt, F. (1991). Cognitive dysfunction in multiple sclerosis: II. Impact on employment and social functioning. Neurology, 41, 692-696.
Reiser, S. J. (1993). The era of the patient: Using the experience of illness in shaping the missions of health care. JAMA, 269(8), 1012-1017.
Robinson, J. E. (2000). Access to employment for people with disabilities: Findings of a consumer-led project. Disability and Rehabilitation, 22(5), 246-253.
Roessler, R. (1996). The role of assessment in enhancing the vocational success of people with multiple sclerosis. Work, 6, 191-201.
Rosenblum, D., & Saffir, M. (1998). Therapeutic and symptomatic treatment of multiple sclerosis. In G. Kraft & R. S. Taylor (Eds.), Multiple sclerosis: A rehabilitative approach (Vol. 9, #3, pp. 587-601). Philadelphia: W.B. Saunders.
Rothwell, P. M., McDowell, Z., Wong, C. K., & Dorman, P. J. (1997). Doctors and patients don't agree: Cross sectional study of patients' and doctors' perceptions and assessments of disability in multiple sclerosis. British Medical Journal, 314, 1580.
Rumrill, P. D. (1996a). Employment and multiple sclerosis: Policy, programming, and research recommendations. Work, 6, 205-209.
Rumrill, P. D. (1996b). Employment issues and multiple sclerosis. New York: Demos.
Rumrill, P. D. (1996c). Project alliance final performance report. New York: National Multiple Sclerosis Society.
Rumrill, P. D., Steffen, J., & Kaleta, K. (1996). Job placement interventions for people with multiple sclerosis. Work, 6, 167-175.
Schapiro, R. T. (1994). Symptom management in multiple sclerosis (2nd edition ed.). New York: Demos.
Schubert, D. S. F., R.H. (1993). Increased depression in multiple sclerosis patients: A meta-analysis. Psychosomatics, 34(2), 124-130.
Schwartz, C. E., Foley, F. W., Rao, S. M., Bernardin, L. J., Lee, H., & Genderson, M. W. (1999). Stress and course of disease in multiple sclerosis. Behavioral Medicine, 25(3), 110-116.
Scott, T. F., Price, T. R., McConnell, H., & Land, D. (1996). Characterization of major depression symptoms in multiple sclerosis patients. The Journal of Neuropsychiatry and Clinical Neurosciences, 8(3), 318-323.
Stenager, E., Knudsen, L., & Jensen, K. (1991). Acute and chronic pain syndromes in multiple sclerosis. Acta Neurologica Scandinavica, 84, 197-200.
Stuifbergen, A. K., & Roberts, G. J. (1997). Health promotion practices of women with multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 78(12 Suppl 5), S3-9.
Sullivan, M. J., Edgley, K., & Dehoux, E. (1990). A survey of multiple sclerosis. Part i: Perceived cognitive problems and compensatory strategies use. Canadian Journal of Rehabilitation, 4(2), 99-105.
Sullivan, M. J., Weinshenker, B., Mikail, S., & Edgley, K. (1995). Depression before and after diagnosis of multiple sclerosis. Multiple Sclerosis, 1(2), 104-108.
Sutcher, H. (1997). Hypnosis as adjunctive therapy for multiple sclerosis. American Journal of Clinical Hypnosis, 39(4), 283-290.
US MS society urges early drug treatment. (1998). Scrip(2381), 21.
Verdier-Taillefer, M. H., Sazdovitch, V., Borel, F., Cesaro, P., Kurtz, A., Millet, M. F., Roullet, E., & Mareau, R. (1995). Occupational environment as risk factor for unemployment in multiple sclerosis. Acta Neurologica Scandinavica, 92(1), 59-62.
Wallace, G. L., & Holmes, S. (1993). Cognitive-linguistic assessment of individuals with multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 74, 637-643.
Walther, E. U., & Hohlfeld, R. (1999). Multiple sclerosis: Side effects of interferon beta therapy and their management. Neurology, 53, 1622.
Watson, C. W. (1959). Effects of lowering body temperature on the symptoms and signs of multiple sclerosis. New England Journal of Medicine(261), 1253-1259.
Weinstock-Guttman, B., & Jacobs, L. D. (2000). What is new in the treatment of multiple sclerosis? Drugs, 59(3), 401-410.
Wells, K. B., Golding, J. A., & Burnam, M. A. (1988). Psychiatric disorder in a sample of the general population with and with our chronic medical conditions. American Journal of Psychiatry, 145, 976-981.
White, D. M., Catanzaro, M. L., & Kraft, G. H. (1993). An approach to the psychological aspects of multiple sclerosis: A coping guide for health care providers and families. Journal of Neurolgic Rehabilitation, 7(2), 43-52.
Wineman, N. M. (1990). Adaptation to multiple sclerosis: The role of social support, functional disability, and perceived uncertainty. Nursing Research, 39(5), 294-299.
Yorkston, K. M., Beukelman, D. R., Strand, E. A., & Bell, K. R. (1999). Management of motor speech disorders in children and adults. Austin, TX: Pro-Ed.
Yorkston, K. M., Klasner, E. R., & Swanson, K. M. (2001). Communication in context: A qualitative study of the experiences of individuals with multiple sclerosis. American Journal of Speech-Language Pathology, 10(2), 126-137.
Zakzanis, K. K. (2000). Distinct neurocognitive profiles in multiple sclerosis subtype. Archives of Clinical Neuropsychology, 15(2), 115-136.
Kurt L. Johnson
University of Washington
Dagmar Amtmann
University of Washington
Kathryn M. Yorkston
University of Washington
Estelle R. Klasner
University of Washington
Carrie M. Kuehn
University of Washington
Kurt L. Johnson, Ph.D., Division of Rehabilitation Counseling, Department of Rehabilitation Medicine, School of Medicine, Box 356490, University of Washington, Seattle, WA 98195. Email: kjohnson@u.washington.edu
COPYRIGHT 2004 National Rehabilitation Association
COPYRIGHT 2004 Gale Group