INTRODUCTION: A female with multiple sclerosis presented to pulmonary clinic with a mediastinal mass.
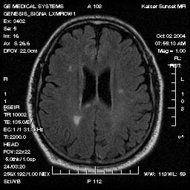
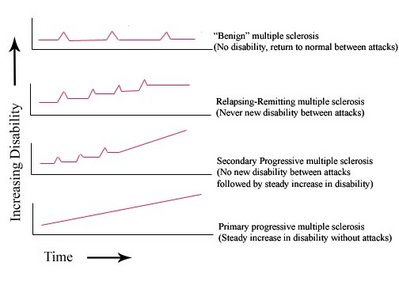
CASE PRESENTATION: A 52-year-old female was referred to pulmonary clinic having developed right-sided chest pain which radiated to both shoulders. The sensation was described as dull and pressure-like. The pain was pleuritic and made worse by swallowing both solids and Liquids. It was not exertional. A two week course of ibuprofen reduced, but did not eliminate the pain. There were no associated symptoms. She specifically denied cough, fevers, chills, night sweats, or weight loss. Her past medical history was significant for multiple sclerosis, diagnosed 28 years ago. The MS was well controlled with 30 mcg of weekly self-administered interferon-beta for the past three years. She had been very active, walking two miles daily without difficulty. The patient was afebrile, heart rate 84,blood pressure 126/80 in both arms respiratory rate 14, and pulse oximetry of 98% while breathing room air. There was no cervical or axillary lymphadenopathy. The lungs were clear to auscultation and heart exam was normal. Neurologic, musculoskeletal, and skin exams were unremarkable. Results of a CBC, serum chemistries, liver function tests, and serial troponins were all within normal limits. ECG showed normal sinus rhythm at a rate of 65. Chest radiograph showed a widened mediastinum and a small right pleural effusion. Computerized tomography of the chest revealed a 3cm mass in the superior mediastinum in addition to the small effusion. Positron emission tomography showed moderately intense tracer uptake in the mediastinum, corresponding to the lesion seen on CT. PPD testing was negative and a serum angiotensin converting enzyme level was normal at 20 IU/ml. Mediastinoscopy revealed multiple enlarged mediastinal and right paratracheal lymph nodes. Pathology showed non-caseating granulomas, and was consistent with sarcoidosis. Acid fast and fungal stains were negative for organisms. A diagnosis of sarcoidosis was made, possibly relating to her use of IFN-[beta]. This medication was discontinued. Repeat CT of the chest at six months demonstrated complete resolution of both the mediastinal lymphadenopathy and the right sided pleural effusion. Her MS remained stable after discontinuation of the IFN-[beta].
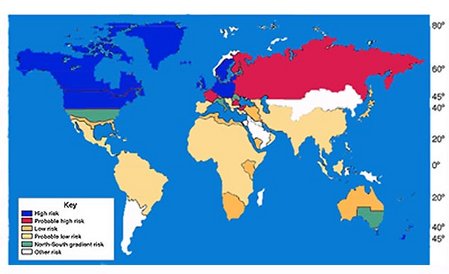
DISCUSSIONS: Sarcoidosis is a systemic granulomatous disease of unknown etiology. Common manifestations include hilar lymphadenopathy, pulmonary infiltrates, ocular and cutaneous lesions, although it can affect any organ system. Neurosarcoidosis rarely mimics multiple sclerosis, and this patient's clinical course was more suggestive of MS. Numerous reports have linked exogenously administered interferons to the development of sarcoidosis. The majority of cases involve patients using IFN-[alpha]; and ribavirin for chronic hepatitis C infection. Interferons are cytokine mediators involved in the early, innate immune response to viral pathogens. They are also crucial to the development of virus-specific adaptive immunity and can enhance antigen presentation to specific T cells. Type I interferons (IFN-[alpha] and IFN-[beta]) have been shown in vitro to promote Th1 cell differentiation. In sarcoidosis, an exaggerated Th1 immune response, to an unknown antigen, is thought to promote macrophage activation and result in the pathologic granulomatous response. This misdirected immune response results in tissue damage in the affected organs.
CONCLUSION: Sarcoidosis is a recognized complication of IFN-[beta] therapy. While the exact etiology of sarcoidosis remains unknown, this unusual ease provides evidence of a contributing role of interferon. The use of IFN-[beta] as a treatment for multiple sclerosis may be associated with an increased risk of sarcoidosis.
REFERENCES:
(1) Antoniou KM et al. Interferons and Their Application in the Diseases of the Lung. Chest, Jan 2003; 123:209-216.
(2) Marzouk K et al. Interferon-induced granulomatous lung disease. Current Opinion in Pulmonary Medicine 2004, 10:435-440.
(3) Sinigaglia F et al. Type I Interferons and the Th1/Th2 paradigm. Developmental and Comparative Immunology 1999. 23:657-663.
DISCLOSURE: Sean O'Reilly, None.
Sean O'Reilly MD * Alexander White MD Agustin Florian MD Tufts-New England Medical Center, Boston, MA
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group