INTRODUCTION: The incidence of acute eosinophilic pneumonia (AEP) among patients admitted with presumed community acquired pneumonia is uncertain, but AEP associated with shock is rare. [1] Medications can cause AEP with the pathophysiology attributed to acute hypersensitivity. [2] We report AEP possibly caused by duloxetine.
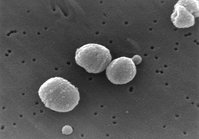
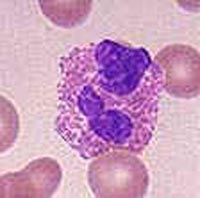
CASE PRESENTATION: A 30 year old Caucasian woman was admitted with five day history of fever, chills, dyspnea, cough, and nausea. She was diagnosed with pneumonia by chest x-ray and prescribed antibiotics one day prior to admission. Past medical history was significant for depression and chronic prescription narcotic use secondary to back pain. She was recently institutionalized for depression, weaned off narcotics, and prescribed duloxetine. Medications on admission were azithromycin, duloxetine, vitamin B12, multivitamin, and Garlic. She denied tobacco use but drank alcohol heavily prior to hospitalization for depression. She had no history of IV drug abuse or HIV exposures. She denied occupational, chemical, dust, or asbestos exposures. She had a parrot for five years, but no recent travel. On admission, the patient was in "mild distress" with temperature of 39.5[degrees]C, blood pressure 95/55 mmHg, heart rate 144 bpm, and respiratory rate 20. Her SpO2 was 90% on room air. Lung exam revealed diffuse crackles. She had 20.4 [10.sup.3]/uL white blood cells with 86% segmented neutrophils. Comprehensive metabolic panel and lactate were within normal limits. Admission ABG showed pH 7.44, PaCO2 30 mmHg, PaO2 49 mmHg and SaO2 84%. Blood cultures were ordered. The admission chest x-ray showed worsening consolidation bilaterally. She was placed on 4 liters oxygen, and ad-ministered ceftriaxone combined with azithromycin. The following day, her clinical course deteriorated with development of respiratory failure and shock. She was intubated and treated with vasopressors. Bronchoalveolar lavage showed no pathogens by stain or culture but revealed 80% eosinophils. Duloxetine was discontinued and methylprednisolone started. Antibiotics and vasopressors were discontinued after two days; the patient was extubated in three. She developed peripheral eosinophilia while still receiving methylprednisolone. She was discharged after eight hospital days on prednisone, fluoxetine, and gabapentin. As an outpatient, eosinophilia resolved then recurred. Eosinophilia finally normalized after fluoxetine was discontinued. Three weeks after discharge, repeat chest x-ray was normal and she was doing Pilates.
DISCUSSIONS: Acute eosinophilic pneumonia was first described as "double pneumonia" with respiratory failure.[3] The AEP diagnostic criteria[4] are: (1) Acute febrile illness < 5 days duration, (2) Hypoxemic respiratory failure, (3) Diffuse alveolar or mixed alveolar-interstitial chest X-ray infiltrates, (4) BAL eosinophils > 25%, (5) Absence of parasitic, fungal, or other infection, (6) Prompt and complete response to corticosteroids, (7) Failure to relapse after discontinuation of corticosteroids. This case fulfills these criteria, with duloxetine and secondarily fluoxetine the inciting agents. Medications are well known causes of eosinophilic pneumonia.[5] Venlafaxine was reported as an inciting agent in 2000. [6] Duloxetine and venlafaxine are similar in mechanism and pharmacodynamics. [7].
CONCLUSION: This may be the first report linking duloxetine with AEP. Cessation of exposure and corticosteroid treatment produced prompt and complete resolution of severe respiratory failure. The diagnosis of AEP was made only by bronchoalveolar lavage, emphasizing the importance of bronchoscopy in selected patients despite the risk imposed by severe hypoxemia.
REFERENCES:
[1] Buddharaju VL et al, Acute eosinophilic pneumonia associated with shock, Crit Care Med 1999;27(9):2014-2016.
[2] Badesch DB et al, Acute eosinophilic pneumonia: a hypersensitivity phenomenon? Amer Rev Respir Dis 1989;139:249-52.
[3] Ibid.
[4] Allen JN and Davis WB, Eosinophilic Lung Diseases, Am J Respir Crit Care Med 1994;150:1423-1438.
[5] http://www.pneumotox.com/indexf.php?fich=clin0&lg=en
[6] Fleisch MC et al, Eosinophilic pneumonia and respiratory failure associated with venlafaxine treatment, Eur Respir J 2000;15:205-208.
[7] Sharma A et al, Pharmacokinetics and Safety of Duloxetine, a Dual-Serotonin and Norepinephrine Reuptake Inhibitor, J Clin Pharmacol 2000;40:161-167.
DISCLOSURE: Antonio Salud II, None.
Antonio V. Salud II MD * Nathan Dean MD University of Utah, Salt Lake City, UT
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group