Rheumatoid arthritis is a systemic disease that may have pulmonary manifestations. We describe a ease of eosinophilic pneumonia as the primary presentation of rheumatoid arthritis. While several cases of acute and chronic eosinophilic pneumonia have been reported in patients with preexisting rheumatoid arthritis, this is the first ease reported in which the eosinophilic lung disease was the initial manifestation of systemic rheumatoid arthritis.
Key words: eosinophilic pneumonia; pulmonary; rheumatoid arthritis
**********
Eosinophilic pneumonias are characterized by the presence of cough, lung infiltrates, and pulmonary eosinophilia. There are two forms of eosinophilic pneumonia, acute and chronic. The latter has a slower onset, milder fevers, and less hypoxia than the acute form) Both tend to respond promptly to therapy with corticosteroids, although the chronic form often recurs once treatment is discontinued. While a majority of patients who develop these pneumonias have a history of atopy, the etiologies of these disorders are unknown. These pneumonias are typically diagnosed by clinical features, by the exclusion of underlying infection or drag reaction, and by finding parenchymal infiltration with eosinophils by transbronchial biopsy or wedge resection. We describe here a case of eosinophilic pneumonia as the initial presentation of a patient with rheumatoid arthritis.
CASE REPORT
A 39-year-old woman presented to her internist with a 5 day history of a hacking, dry cough. Despite initial treatment with albuterol and guaifenesin, followed by a 6 day course of erythromycin, her symptoms progressed to include night sweats, fatigue, pleuritic chest pain, and severe arthralgias and myalgias. A chest radiograph revealed a right upper lobe infiltrate that was suggestive of pneumonia, and after a 12-day course of treatment with levofloxacin failed to improve the symptoms, the patient was referred to a pulmonologist for further evaluation. Her medical history was notable for a positive purified protein derivative test result and 12 months of treatment with isoniazid in childhood. The medications used were albuterol, guaifenesin, levofloxacin, and an oral contraceptive.
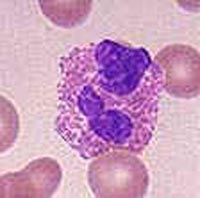
On presentation, the patient was ill-appearing, with a frequent. dry cough. She had a respiratory rate of 16 breaths/min, a temperature of 98.3[degrees]F, and bronchial breath sounds with egophony in the right upper and middle lung zones. There was no rash or palpable lymphadenopathy. The peripheral WBC count was 18,700 cells/[micro]L (neutrophils, 88%; lymphocytes, 8%; monocytes, 3%; eosinophils, 1%). As polyarthralgias progressed to polyarthritis, a rheumatologic workup revealed a sedimentation rate if 116, negative Lyme serology, positive antinuclear antibody (ANA) test result (titer, 1:40 with a diffuse pattern), negative anti-double strand DNA test result, and a markedly positive serum rheumatoid factor test result (titer, > 1:1,280). A chest CT scan (Fig 1) demonstrated dense consolidations in the posterior segment of the right upper lobe and superior segment of the right lower lobe, with air bronchograms and evidence of old granulomatous disease. Bronchoscopy revealed no endobronchial lesions or significant secretions, and the findings of BAL fluid cytology and cultures (including those for acid fast bacilli) were negative. Serology findings were negative fur coccidiomycosis, histoplasmosis, blastomycosis, parvovirus, pertussis, and mycoplasma pneumoniae, as was that for the anti neutrophil cytoplasmic antibody test. The patient was referred for video-assisted thoracoscopy for the tissue diagnosis of refractory pneumonia.
[FIGURE 1 OMITTED]
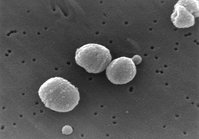
Wedge resection from the patient's right upper and lower lobes (Fig 2) revealed organizing pneumonitis with a prominent component of fibrinous exudates and numerous eosinophils, suggesting the presence of eosinuphilic pneumonia. The findings of tissue cultures, including acid-fast bacilli, were negative. The patient was started on a course of treatment with high-dose IV corticosteroids (initially 80 mg methylprednisolone daily), and her fever and pulmonary symptoms resolved within 4 days.
In the year since her presentation, the patient has not had a recurrence of her pulmonary: symptoms or infiltrates, but has had persistent polyarthritis despite several months of therapy with oral corticosteroids, rofecoxib, and hydroxychloroquine. Her course of treatment with corticosteroids was tapered off over a 6-month period, and she has been transitioned to therapy with methotrexate and etanercept to control her rheumatoid arthritis, with close follow-up given to her history of a positive purified protein derivative test result.
DISCUSSION
Rheumatoid arthritis is a systemic autoimmune disease associated with a number of pulmonary manifestations, including pleural disease, rheumatoid nodules, interstitial lung disease, pulmonary vascular disease, and airway involvement. (2) There have been a handful of ease reports in the English literature of acute eosinophilic pneumonia (one case) (3) and chronic eosinophilic pneumonia (five cases) (4-7) associated with rheumatoid arthritis (with varying degrees of peripheral eosinophilia and rheumatoid factor positivity). Many of these reports concerned patients with long-standing rheumatoid arthritis, in whom the medications used in the treatment of the arthritis may have contributed to the development of lung disease. In the most recent report, a 55-year old woman developed rheumatoid arthritis with peripheral eosinophilia coincident with the onset of eosinophilic pneumonia. (7) We describe the first report of a patient with rheumatoid arthritis, without peripheral eosinophilia, whose initial presentation was eosinophilic pneumonia. Although difficult to characterize as either acute or chronic eosinophilie pneumonia, this case is most consistent with the chronic variety,, given the subacute presentation, mild hypoxemia, and dense consolidations seen on chest imaging. However, in the year since her initial presentation our patient has not had any relapses of eosinophilic pneumonia, which is a common feature of the chronic subtype. This may be due to the uninterrupted use of immunosuppressive medications for the treatment of her persistent arthritic symptoms.
CONCLUSION
Several cases of eosinophilic pneumonia associated with rheumatoid arthritis have been described. We now include the ease of this patient wit h eosinophilic pneumonia as the initial presentation of the disease. Eosinophilic pneumonia should be considered as a diagnosis in a patient who presents with pulmonary infiltrates, fever, and joint symptoms consistent with rheumatoid arthritis.
REFERENCES
(1) Hayakawa H, Sate A, Toyoshima M, et al. A clinical study of idiopathic eosinophilic pneumonia. Chest 1994; 105:1462-1466
(2) Tanoue LT. Pulmonary manifestations of rheumatoid arthritis. Clin Chest Med 1998; 19:667-685
(3) Mehandru S, Smith RL, Sidhu GS, et al. Migratory pulmonary infiltrates in a patient with rheumatoid arthritis. Thorax 2002; 57:465-467
(4) Cooney TP. Interrelationship of chronic eosinophilic pneumonia, bronchiolitis obliterans, and rheumatoid disease: a hypothesis. J Clin Pathol 1981; 34:129-137
(5) Papiris SA, Maniati MA, Kalousis JV, et al. Chronic eosinophilic pneumonia in rheumatoid arthritis. Monaldi Arch Chest Dis 1995; 50:360-362
(6) Payne CR, Connelhm SJ. Chronic cosinophilie pneumonia complicating long-standing rheumatoid arthritis. Postgrad Med J 1980; 56:519-520
(7) Kwak JJ, Chang JE, Lee J, et al. Chronic eosinophilic pneumonia associated with an initiation of rheumatoid arthritis. Clin Rheumatol 2003; 22:240-243
* From the Divisions of Pulmonary, Critical Care, and Sleep Medicine (Drs. Norman and Roberts), and Rheumatology (Dr. Piecyk), Beth Israel Deaconess Medical Center, Boston, MA. Manuscript received December 2, 2003; revision accepted May 26, 2004.
Reproduction of dais article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@ehestnet.org).
Correspondence to: David Roberts, MD, FCCP, Division of Pulmonary, Critical Care, and Sleep Medicine (1), Beth Israel Deaconess Medical Center, E/KS-B23, 330 Brookline Ave, Boston, MA 02215; e-mail: dhrohert@bidmc.harvard.edu
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group