Case Report
We describe a rare case of a 29-year-old woman with chronic eosinophilic pneumonia (CEP) presenting with massive bilateral pleural effusion leading to respiratory failure, a complication that was not reported before with CEP. The patient was successfully managed with ventilatory support and steroid therapy. On long-term follow-up, she remained well, receiving a low maintenance dose of prednisone without evidence of relapse of the disease. (CHEST 2001; 119:968-970)
Key words: chronic eosinophilic pneumonia; massive pleural effusion; respiratory failure.
Abbreviations: CEP = chronic eosinophilic pneumonia; HES = hypereosinophilic syndrome
Chronic eosinophilic pneumonia (CEP), a rare eosinophilic lung disease of unknown etiology, is characterized by peripheral blood eosinophilia, chest radiograph infiltrates, and prompt response to corticosteroid therapy.[1] The first detailed description of CEP was by Carrington et al in 1969.[2]
CEP most commonly affects women of middle age. The usual symptoms are cough, dyspnea, fever, and weight loss. We report a case of CEP presenting with massive, rapidly accumulating pleural effusion progressing to respiratory failure that, to our knowledge, has not been reported previously.
CASE REPORT
A 29-year-old nonsmoking woman presented with a 5-month history of shortness of breath and dry cough. She denied any history of fever, night sweats, or weight loss. She had no history of chest pain, palpitation, arthralgia, arthritis, or skin rash. There was no neurologic or GI symptoms and no travel history.
The patient was initially admitted to another Facility with the same symptoms and received a diagnosis of bronchial asthma and bilateral exudative pleural effusions requiting frequent uncomplicated therapeutic drainage. The original reported WBC wits 10,000 cells/[micro]L with 70% eosinophils; no pulmonary function tests were performed. However, pleural analysis was reported as clear and nonhemorrhagic, with 70% lymphocytes, 1% neutrophils, and 2% eosinophils. Pleural biopsy was reported to show nonspecific inflammatory reaction consisting mainly of eosinophils.
On admission at our hospital, she was afebrile, with a respiratory rote of 25 breaths/min and decreased chest expansion. Dullness to percussion wits noted with decreased air entry at the bases. The rest of the physical examination was unremarkable. The patient was receiving salbutamol and beclomethasone inhalers from the other facility.
Results of laboratory investigations are as follows: hemoglobin, 13.9 g/dL; WBC count, 9,300 cells/[micro]L; platelets, 360,000 cells/ [micro]L; and persistent eosinophilia of 1,800 to 3,200 cells/[micro]L. Basic biochemical profile and serum immunoglobulins, including IgE were normal. Serology for locally prevalent parasites (amebiasis, echinococcosis, leishmaniasis, and schistosomiasis) by enzyme-linked immunosorbent assay method was negative. Antinuclear antibody, antimitochondrial antibody, anti-smooth muscle antibody, and anti-double-strand DNA were negative. Rheumatoid factor was weakly positive. Repeated sputum microscopy and culture and polymerase chain reaction for Mycobacterium tuberculosis results were negative. Mantoux test was negative. Stool examinations for ova and parasites (namely trichinosis, echinococcus, and schistosomiasis) were negative. Pulmonary function tests showed a severe restrictive pattern (Table 1).
[TABULAR DATA 1 NOT REPRODUCIBLE IN ASCII]
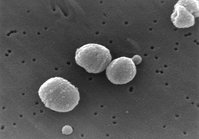
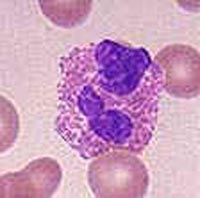
Chest radiography revealed bilateral pleural effusions with interstitial and airspace opacities in the lower third of the lungs (Fig 1). A CT scan of the chest demonstrated bilateral loculated pleural effusions; collapse and consolidation of the right lower, middle, and lingula lobes; and ground-glass opacities in the, right upper lobe (Fig 2). The pleural fluid protein was 4.3 g/dL, lactate dehydrogenase was 1,554 IU/L, and total WBC count wits 1,580 cells/[micro]L with 21% eosinophils and no abnormal cells. Pleural biopsy showed mixed inflammatory cell infiltrate with predominance of eosinophils. Echocardiographic findings were normal. Bone marrow examination showed 40% infiltration with eosinophils and a normal karyotype.
[Figures 1-2 ILLUSTRATION OMITTED]
The patient required repeated therapeutic pleural fluid drainage mitt insertion of a chest tube without clinical improvement because of rapid reaccumulation and loculation of the fluid. Respiratory failure occurred on day 3, and she required intubation and mechanical ventilation. Bronchoscopy demonstrated normal airways, and BAL revealed a WBC count of 5,100 cells/[micro]L with 80% eosinophils and a negative culture finding.
On the basis of the persistent peripheral eosinophilia, infiltrates on chest radiography, eosinophilic pleural effusion, high percentage of eosinophils in the BAL, and negative investigations for other causes of eosinophilia, the diagnosis of CEP was made.
The patient responded rapidly to treatment with IV methylprednisolone, 1 g/d; 3 days later, she was successfully extubated. Her treatment was changed to oral prednisolone, 40 mg/d, and she was discharged on the eighth hospital day.
On follow-up visits, the patient remained asymptomatic, and the prednisolone was tapered to 15 mg/d by 6 months and was stopped by 9 months, with chest radiography showing residual bilateral pleural thickening, and significant improvement on pulmonary function testing (Table 1). On follow-up, there was no relapse 4 months after discontinuation of steroid therapy.
DISCUSSION
Our patient satisfied the criteria for the diagnosis of CEP.[1] Pulmonary involvement may occur in 40% of patients with idiopathic hypereosinophilic syndrome (HES) and may therefore closely resemble CEP.[1,3] However, because of the absence of multiorgan involvement with signs of end-organ damage, one of the triad of HES,[3] and the characteristic radiologic findings of CEP in our patient, the diagnosis of HES was excluded. Bronchiolitis obliterans with organizing pneumonia may also mimic CEP, but the radiologic and BAL findings were incompatible with the diagnosis of bronchiolitis obliterans with organizing pneumonia.[1]
The onset of CEP is usually insidious, and symptoms are present for at least a few months before diagnosis, as in our patient. If the diagnosis is delayed, progression to respiratory failure may occur.[1] Bronchial asthma is present in about half of the cases.[4] Peripheral eosinophilia occurs in most patients with CEP and may be associated width elevated IgE levels. The latter may parallel the disease activity.[1] In 25% of patients with CEP, chest radiography shows the characteristic, extensive bilateral peripheral infiltrates, described as a photographic negative image of pulmonary edema.[5] This was not present in our patient.
Pleural effusion is uncommon in CEP. In a review of 19 cases of CEP, only 2 patients had pleural effusion, and in a multicenter study, 2 of 62 patients had bilateral small-size pleural effusions.[4,6] The mechanism of pleural effusion in CEP is unknown. However, it might be because of tissue damage induced by infiltration with eosinophils, antibody-mediated cellular toxicity, or the release of intracytoplasmic leukotriene that increases microvascular permeability.[1]
Our patient had severe restrictive lung disease, as reported in the majority of patients with CEP.[1] Durieu et al[7] found that 9 of 19 patients with CEP had restrictive abnormalities and 4 patients had obstructive abnormalities, and on long-term follow-up, 8 of the 19 patients showed complete recovery. The high diffusion capacity of the lung for carbon monoxide/alveolar volume ratio in our patient could be explained, initially, by the large pleural effusion, collapse and entrapment of the lungs, and, lately, by pleural thickening.[7-9]
Open lung biopsy is performed when the diagnosis is in doubt,[1] and this usually shows interstitial and alveolar infiltration with eosinophils, microabscesses, Charcot-Leyden crystals, and bronchiolitis obliterans. The prompt response to corticosteroids, as seen in our patient, is characteristic in CEP.[1] The prognosis of CEP is excellent, but there may be relapse of disease. Therefore, decreasing doses of corticosteroids are recommended for at least 6 to 19 months.[1]
CONCLUSION
Although not reported before, rapidly accumulating pleural effusions could be a presenting feature of CEP. Early recognition of this is important in view of the good response to treatment with corticosteroids.
REFERENCES
[1] Allen JN, Davis WB. Eosinophilic lung diseases. Am J Respir Crit Care Med 1994; 150:1423-1438
[2] Carrington CB, Addington, WW, Goff, AM, et al. Chronic eosinophilic pneumonia. N Engl J Med 1969; 980:787-798
[3] Fauci AS, Harley JB, Roberts WC, et al. The idiopathic hyperoesinophilic syndrome: clinical, pathophysiologic, and therapeutic considerations. Ann Intern Med 1982; 97:78-92
[4] Marchand E, Reynand-Gaubert M, Lauque D, et al. Idiopathic chronic eosinophilia pneumonia: a clinical and follow-up study of 62 cases. Medicine 1998; 77:299-312
[5] Gaensler EA, Carrington CB. Peripheral opacities in chronic eosinophilic pneumonia: the photographic negative of pulmonary edema. AJR Am J Roentgenol 1977; 128:1-13
[6] Jederlinic PJ, Sicilian L, Gaensler EA. Chronic eosinophilic pneumonia: a report of 19 cases and a review of the literature. Medicine 1988; 67:154-162
[7] Durieu J, Wallaert B, Tonnel AB. Long term follow-up of pulmonary function in chronic eosinophilic pneumonia. Eur Respir J 1997; 10:286-291
[8] Seigler D, Zorab PA. The influence of lung volume on gas transfer in scoliosis. Br J Dis Chest 1982; 76:44-50
[9] Miller A. Pulmonary function tests in clinical and occupational lung disease. Orlando, FL: Grune and Stratton, 1986; 147-148
(*) From the Department of Medicine, King Khalid National Guard Hospital, Jeddah, Saudi Arabia.
Manuscript received November 23, 1999; revision accepted August 15, 2000.
Correspondence to: Yaseen S. Samman, MD, FCCP, Department of Medicine, King Khalid National Guard Hospital, PO Box 9515, Jeddah 21423, Saudi Arabia; e-mail: Sammanys@ngha.med.sa
COPYRIGHT 2001 American College of Chest Physicians
COPYRIGHT 2001 Gale Group