Women typically have been counseled to avoid using psychiatric medications during pregnancy because of either known or unknown risks of prenatal exposure to these medications. But data suggest that pregnancy does not protect women from new onset or relapse of psychiatric disorders.
This is particularly true for women who have disorders such as schizophrenia or bipolar illness, which is also now treated with antipsychotics. Women with schizophrenia who stop their antipsychotics are at a great risk for relapse, which often leads to behaviors harmful to them and their fetuses.
So what do we know about the reproductive safety of the older typical antipsychotics and the newer atypical antipsychotics?
The latter are becoming first-line treatment for many people with schizophrenia because they do not have some of the side effects of the older medications and because they appear to result in better acute and long-term responses. They are also increasingly being used for a range of other psychiatric disorders, including obsessive-compulsive disorder, posttraumatic stress disorder, anxiety disorders, and depression.
Most of the available reproductive safety data come from literature on the typical antipsychotics and are several decades old. These data suggest that there is no increased risk of congenital malformations associated with first-trimester exposure to high-potency antipsychotics such as haloperidol (Haldol) or midpotency antipsychotics such as perphenazine (Trilafon). There also appear to be no safety issues when these drugs are used in labor and delivery or post partum, and some literature suggests that these agents are not problematic when used during lactation.
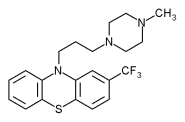
So the standard approach in our clinic is to continue treatment in patients who are dependent on a typical high-potency antipsychotic, such as haloperidol, fluphenazine hydrochloride (Prolixin, Permitil), or trifluoperazine (Stelazine), or a midpotency antipsychotic.
We avoid using low-potency antipsychotics, such as chlorpromazine because of hypotension and other side effects, and a suggestion that they might be linked to a slightly increased risk of malformations.
Unfortunately, we have only sparse data on the reproductive safety of the currently available newer compounds, clozapine (Clozaril), risperidone (Risperdal), olanzapine (Zyprexa), quetiapine (Seroquel), and ziprasidone (Geodon). We typically suggest that pregnant women who require antipsychotics and are on an atypical agent should switch to one of the older drugs. We also recommend that they not breast-feed while on an atypical agent until we have better safety data.
Some patients who do not respond to treatment with typical antipsy-chotics but respond only to an atypical agent. We have followed a small number of such patients who have stayed on the atypical drug during pregnancy and so far have not observed any unexpected problems.
The manufacturer of olanzapine maintains a registry of fewer than 100 women exposed to this drug during pregnancy So far there is no evidence of an increased risk for congenital malformations or other problems.
Obtaining more data on the reproductive safety of these newer antipsychotics is becoming even more important because atypical agents are increasingly being used for psychiatric disorders in women who may be more likely to bear children, such. as those with anxiety or mood disorders, compared with those with schizophrenia.
We may be seeing more women on these drugs becoming pregnant, because they have less of an impact on fertility than the older drugs, which increase prolactin secretion. With the exception of risperidone, which causes relatively high rates of hyperprolactinemia, ziprasidone, quetiapine, olanzapine, and clozapine are prolactin sparing compounds.
An option for a woman with bipolar disease who is taking an atypical antipsychotic is to switch her to lithium during pregnancy Even though lithium is a teratogen, we know that the absolute risk of having a child with Ebstein's anomaly after first-trimester exposure is about 1 in 1,000 to 1 in 2,000.
Since we basically know nothing about the reproductive safety of atypical antipsychotics, I would rather see a woman who has been on a drug like olanzapine or quetiapine for bipolar disease switched to lithium during pregnancy since it has a known teratogenic potential.
DR. LEE COHEN is a psychiatrist and director of the perinatal psychiatry program at Massachusetts General Hospital, Boston.
COPYRIGHT 2001 International Medical News Group
COPYRIGHT 2001 Gale Group