We describe a rare case of apocrine adenoma of the breast in a 45-year-old man. The patient presented with a tender lump in his left breast that had been present for 6 months. A mammogram identified a 3-mm nodular density in the breast, which was described as a hypoechoic nodule on ultrasound. Microscopic examination of tissue from an excisional biopsy revealed a 3-mm group of benign glands with abundant granular, eosinophilic cytoplasm and apical luminal blebbing, consistent with an apocrine adenoma. After reviewing other reported apocrine adenomas in the literature, we determined that our case was the smallest detected apocrine adenoma to be reported to date.
Pure apocrine adenomas of the breast are extremely rare but have been reported previously in 5 cases, 1 case involving a boy, 3 involving women, and 1 girl. A 14-year-old boy was reported to have an apocrine adenoma of undisclosed size associated with gynecomastia. Two women were reported to have apocrine adenomas of the breast, with gross measurements ranging from 7 mm to 1.7 cm. The tumor in a third case involving a woman was described only as "small." The tumor size in a 14-year-old girl was not given.
We describe a rare case of a 3-mm apocrine adenoma of the breast in a 45-year-old man who presented with a tender lump in his left breast of 6 months' duration. To our knowledge, this is the smallest adenoma reported to date.
REPORT OF A CASE
A 45-year-old man without significant past medical history noticed a tender lump in his left breast that had been present for 6 months. The mass remained unchanged during this time; however, at the end of the 6 months, the lump seemed to be increasing in size. The patient had a family history of breast cancer in which a maternal aunt was diagnosed with the disease at the age of 40 years. He had a social history significant for smoking and alcohol use. A physical examination revealed an obese man (body mass index of 28) with gynecomastia, left greater than right. A pea-sized, mobile mass was palpable in the upper outer quadrant of the left breast. No nipple discharge was present. His prolactin level at the time was 4.29 ng/mL (normal range, 1.61-18.77 ng/ mL), and his testosterone level was 481.5 ng/dL (normal range, 245-1836 ng/dL). Liver function test results were within normal limits, and no other stigmata of alcoholic liver disease were present.
A mammogram of the left breast revealed a small nodular density in the left retroareolar region measuring 3 x 3 mm (Figure 1). No calcifications suggestive of malignancy were identified. The right breast was unremarkable. An ultrasound later confirmed a small hypoechoic nodule measured at 6.2 x 4.4 mm. The mass was then excised under local anesthesia without complications and was sent for pathologic examination.
PATHOLOGIC FINDINGS
A fragmented aggregate of yellow adipose tissue measuring 3.5 cm was received for examination. No grossly identifiable lesion was seen. The entire specimen was submitted for microscopic examination. Microscopic examination revealed a well-circumscribed group of glands measuring 3.0 mm (Figure 2), a few of which were minimally cystically dilated. The cells had abundant granular, eosinophilic cytoplasm and apical luminal blebbing ("snouts"). Nuclei were round and uniform. No atypia, mitotic activity, or evidence of invasion were present (Figure 3). These findings are consistent with an apocrine adenoma. The remaining tissue submitted was fibroadipose tissue only. The apparent gynecomastia was not confirmed histologically.
COMMENT
The focus of apocrine-type proliferation present in our case fits the criteria for pure breast adenomas outlined by Hertel et al in 1976.1 The criteria require the lesion to be homogenous throughout; to be sharply demarcated from the surrounding breast tissue; to have only epithelial proliferative elements; and to have a minimal, supportive stromal component.
A few similar cases of apocrine adenomas have been reported in the literature (Table). Costa2 described this lesion in a 14-year-old girl in 1974. She had a breast nodule present for several months that suddenly doubled in size within 1 week. The actual size was not given. The gross and microscopic appearance were said to be consistent with an apocrine adenoma, and it was the first described case of its kind in the literature.
Tesluk et al3 described a 24-year-old woman with a painful, palpable, 1-cm-diameter mass in her left breast for 4 months that was growing slightly. The mass was excised, and pathologic examination revealed a 0.7-cm, well-circumscribed, tan nodule with histologic features consistent with an apocrine adenoma. The lesion did not invade the stroma. Adjacent breast tissue revealed only a hyperplastic lobule; no foci of apocrine metaplasia were found.
De Potter et al4 reported the case of a 14-year-old boy with a firm, enlarging nodule in his left breast that had been present for several weeks. His prolactin level at the time was 16.5 ng/mL (normal range,
Baddoura and Judd5 described a 19-year-old woman with a palpable, mobile, tender, slowly enlarging, left inner quadrant breast mass that had been present for 4 months. The patient occasionally experienced a white nipple discharge, and the mass seemed to increase and decrease in size with each menstrual cycle. She was noted to be taking oral contraceptive pills. Examination revealed a well-circumscribed nodule made up of multilocular cystic spaces containing numerous papillary fronds projecting into the lumina. Microscopically, the histology was consistent with that of an apocrine adenoma. There was no evidence of fibrocystic change or apocrine metaplasia in adjacent, normal breast tissue.
Finally, Lui et al6 recently published a report of a 72-year-old woman with a history of left mastectomy for invasive ductal carcinoma who presented with an impalpable, ill-defined calcific density in the upper outer quadrant of her right breast on mammogram. A stereotactic, large-core needle biopsy was performed to obtain tissue for pathologic diagnosis. A well-circumscribed lesion with the characteristics of an apocrine adenoma was identified microscopically within the tissue. The stroma was noted to be sparse in the tissue examined.
All of the previously reported cases, as well as our case, share the diagnostic features of an apocrine adenoma as defined by Hertel et al,1 including isolated breast lesions consisting of benign, proliferating apocrine epithelial elements with minimal stroma. Our case, however, represents a variation, since the adenoma appeared in a man with gynecomastia. It is also the smallest (3 mm) apocrine adenoma reported to date.
Apocrine metaplastic changes have been associated with gynecomastia. Gynecomastia is characterized by ductal epithelial proliferation, which is then susceptible to undergoing apocrine metaplasia. However, a pure proliferation of apocrine epithelium is rare, even in the most common of proliferative breast lesions in women. It is understandably even more remarkable to find a pure apocrine adenoma in a male.
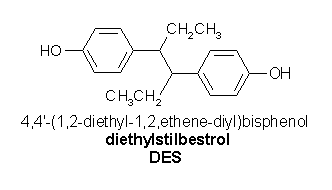
Female hormones lead to gynecomastia, as demonstrated in patients with alcoholic liver disease and those who have been treated with drugs such as stilbestrol. Dilley et al7 suggested that androgens might then play a role in the development of apocrine metaplasia in the hormonally stimulated breast tissue.
References
1. Hertel BF, Zaloudek C, Kempson R. Breast adenomas. Cancer. 1976;37: 2891-2905.
2. Costa A. Una variente non conosciuta di adenoma upro della ghiandola mammaria: l'adenoma pura a cellule apocrine. Arch De Vecchi Anat Patol. 1974; 60:393-401. Cited in Tesluk et al.3
3. Tesluk H, Amott T, Goodnight JE. Apocrine adenoma of the breast. Arch Pathol Lab Mod. 1986;110:351-352.
4. De Potter CR, Cuvelier CA, Roels HJ. Apocrine adenoma presenting as gynaecomastia in a 14-year-old boy. Histopathology. 1988;13:697-699.
5. Baddoura FK, Judd RL. Apocrine adenoma of the breast: report of a case with investigation of lectin binding patterns in apocrine breast lesions. Mod Pathol. 1990;3:373-376.
6. Lui M, Dahlstrom JE, Bell S, James DT. Apocrine adenoma of the breast: diagnosis on large core needle biopsy. Pathology. 2001;33:149-152.
7. Dilley WG, Leight GS Jr, Silva JS, Ammirata S, Haagensen DE, Wells SA. Androgen stimulation of gross cystic disease fluid protein and carcinoembryonic antigen in patients with metastatic breast carcinoma. J Natl Cancer Inst 1983;70: 69-74.
Melissa A. Pasquale-Styles, MD; Clara Milikowski, MD
Accepted for publication June 19, 2003.
From the Departments of Pathology, Jackson Memorial Hospital, Miami, Fla (Dr Pasquale-Styles), and Veterans Affairs Medical Center, Miami, Fla (Dr Milikowski).
Reprints: Clara Milikowski, MD, Miami Veterans Affairs Medical Center, 1201 NW 16th St, Room A-309, Miami, FL 33125 (e-mail: Clara.Milikowski@med.va.gov).
Copyright College of American Pathologists Nov 2003
Provided by ProQuest Information and Learning Company. All rights Reserved