* Dutasteride. The U.S. Food and Drug Administration (FDA) approved dutasteride (Avodart) for the treatment of symptomatic benign prostatic hyperplasia (BPH) in men with an enlarged prostate to improve urinary symptoms, reduce risk of acute urinary retention, and reduce the need for BPH-related surgery.
According to the manufacturer, dutasteride inhibits type 1 and type 2 enzymes responsible for the conversion of testosterone to dihydrotestosterone, the primary cause of prostate growth. Side effects may include impotence, decreased libido, breast tenderness, gynecomastia, and ejaculation disorders.
Women and children should not use dutasteride. Women who are pregnant or may become pregnant should not handle dutasteride because of the risk of absorbing dutasteride and the subsequent potential risk to a male fetus. Men treated with dutasteride should not donate blood until at least six months after their final dose to prevent giving the drug to a pregnant woman through a blood transfusion. Dutasteride is contraindicated in men with an allergic reaction to the drug or its ingredients.
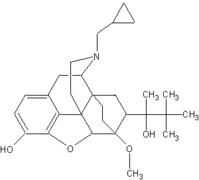
* Buprenorphine. Buprenorphine hydrochloride (Subutex) and the combination buprenorphine hydrochloride and naloxone hydrochloride (Suboxone) have been approved for the treatment of opiate dependence. The agents treat opiate addiction by preventing symptoms of withdrawal from heroin and other opiates.
Buprenorphine only is intended for use at the beginning of treatment for drug abuse. Buprenorphine combined with the opiate antagonist naloxone is intended to be the formulation used in maintenance treatment of opiate addiction. Naloxone is added to buprenorphine to guard against intravenous abuse of buprenorphine by persons physically dependent on opiates.
The U.S. Drug Enforcement Administration (DEA) placed buprenorphine in Schedule III under the Controlled Substances Act. Buprenorphine is considered to have less risk for causing psychologic and physical dependence than the drugs in Schedule II (such as morphine, oxycodone, fentanyl, or methadone).
Buprenorphine can be prescribed in an office setting under the Drug Addiction Treatment Act (DATA) of 2000. Until recently, opiate dependence treatments in Schedule II, like methadone, could be dispensed in a very limited number of clinics that specialized in addiction treatment. As a consequence, there have not been enough addiction treatment centers to accommodate all patients desiring therapy. Under this new law, medications for the treatment of opiate dependence that are subject to less restrictive controls than those of Schedule II can be prescribed in a physician's office by specially trained physicians. This change is expected to provide patients greater access to needed treatment.
Side effects most commonly seen with the use of both drugs include cold or influenza-like symptoms, headaches, sweating, sleeping difficulties, nausea, and mood swings. Clinical data indicate that the risk of serious diminished breathing may be less with buprenorphine than other opioids when used in high doses or in overdose situations.
Buprenorphine has been associated with deaths related to diminished breathing, especially when used in combination with alcohol or other central nervous system depressant drugs, according to reports from France, where it has been available for several years.
A risk-management program has been designed to deter abuse and diversion from legitimate use by training physicians regarding proper use of these drugs, close monitoring of drug distribution channels, and child-resistant packaging.
DATA provisions include limits on the number of patients individual physicians are allowed to treat and special DEA registration for the use of this drug, thus providing additional safeguards as buprenorphine enters the office-based treatment setting.
The risk-management program also provides for active and passive surveillance to identify if and when the drugs are being abused. The surveillance will include interviews with substance abusers, monitoring local drug markets, data collection, and the monitoring of adverse event reports. Reports of the results of these surveillance efforts will enable the FDA to identify untoward effects from the availability of buprenorphine and, if indicated, to take appropriate actions to protect the public health.
COPYRIGHT 2002 American Academy of Family Physicians
COPYRIGHT 2002 Gale Group