Kyle Moores, 19, of Manassas, Va., says he knew he needed help when his abuse of the pain reliever OxyContin (oxycodone) left him drowning in debt and unable to hold a job. "It put me basically in a zombie mode for a year and a half," says Moores, who crushed and snorted the drug. "I finally realized I was losing my life."
Moores was successfully treated at an addiction facility in Richmond, Va. He spoke about his journey to recovery in January at a media event to kick off a joint public education program on the dangers of prescription drug abuse.
The program, sponsored by the Food and Drug Administration and the Substance Abuse and Mental Health Services Administration (SAMHSA) includes posters, public service announcements, and brochures featuring the slogans "The Buzz Takes Your Breath Away ... Permanently" and "It's To Die For." The messages target people ages 14 to 25, but they are relevant to anyone who abuses prescription drugs.
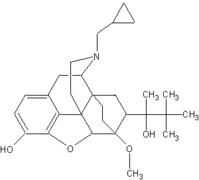
John Jenkins, M.D., director of the FDA's Office of New Drugs, says the FDA is especially concerned about the misuse of single ingredient, controlled-release formulations of opiates, such as OxyContin. "Abuse and misuse of these products is particularly dangerous because they contain higher doses of the drug and are designed to release the drug slowly over a 12- or 24-hour, or longer, period of time for sustained relief of pain," Jenkins says. "Damaging the controlled-release mechanism for these products, such as crushing an OxyContin tablet, can result in immediate release of the high dose of drug, which can be fatal."
In 2001, almost 3 million youths ages 12 to 17 and almost 7 million young adults between 18 and 25 reported using prescription medications nonmedically at least once in their lifetimes, according to the National Household Survey on Drug Abuse conducted by SAMHSA.
Data provided by SAMHSA's Drug Abuse Warning Network indicates that visits to hospital emergency departments related to narcotic prescription pain relievers increased significantly from 1994 to 2001. The highest increases were seen with oxycodone, methadone, morphine, and hydrocodone. Narcotic pain relievers, also known as opiates, are the most commonly abused prescription drugs.
The FDA is working with manufacturers of controlled-release opiates to implement risk-management plans aimed at minimizing abuse while still keeping the products available for people with a legitimate medical need. "In many cases, prescription opiate pain relievers are the most effective treatments available to help patients control their pain and lead productive lives," Jenkins says. But they also have potentially serious side effects, the most serious of which is the risk of respiratory failure.
"While addiction occurs after repeated use, death can occur after a single dose," Jenkins says. "So the first time that someone decides to abuse or misuse a prescription opiate pain reliever may be their last decision."
H. Westley Clark, M.D., J.D., director of SAMHSA's Center for Substance Abuse Treatment, wants people who are abusing prescription drugs to know that effective addiction treatment is available. Clark says that primary care physicians play a critical role in screening, assessing, and referring people with potential substance abuse problems.
According to Clark, "The recent approval by the FDA of buprenorphine to treat prescription drug abuse, and the office-based use of other addiction medications likely to be approved in the years ahead, makes the role of primary care physicians more vital than ever." In October 2002, the FDA approved Subutex (buprenorphine) and Suboxone (buprenorphine and naloxone)--the first narcotic drugs available to treat opiate dependence that can be prescribed in an office setting.
To contact SAMHSA's substance abuse treatment 24-hour helpline, call 1-800-662-HELP (1-800-662-4357), or visit www.findtreatment.samhsa.gov.
COPYRIGHT 2003 U.S. Government Printing Office
COPYRIGHT 2004 Gale Group