Suboxone
Buprenorphine, also colloquially referred to as bupe, is an opioid drug with partial agonist and antagonist actions. Buprenorphine hydrochloride was first marketed in the 1980s by Reckitt & Colman (now Reckitt Benckiser) as an analgesic, yet is now primarily used for the treatment of opioid addiction. It is a Schedule III drug under the Convention on Psychotropic Substances. more...
Commercial preparations
Britsh firm Reckitt & Colman (now Reckitt Benckiser) first marketed buprenorphine under the trade names Temgesic (sublingual/parenteral preparations, no active additives) and Buprenex (parenteral, no active additives). Two more recent formulations from Reckitt Benckiser have been approved for opioid addiction treatment in the U.S.: Subutex (lemon-lime flavored sublingual, no active additives; in 2mg and 8mg dosages) and Suboxone (orange-tang flavored sublingual, one part naloxone for every four parts buprenorphine; hexagon shaped tablet in 2mg and 8mg dosages). Suboxone contains the opioid antagonist naloxone to deter illicit intravenous preparation of the tablet, this is intended to attenuate the effects of buprenorphine on opioid-naive users should this formulation be injected - however no human studies have been done demonstrating the efficacy of this approach with buprenorphine. It must also be noted that buprenorphine in and of itself will induce a precipitated withdrawal syndrome if ingested by an acutely opioid dependant/intoxicated individual.
Buprenorphine is also delivered transdermally in 25, 50 and 75 mcg/hour. The trade name in the UK is Transtec, and manufactured by Napp. A new 5, 10 and 20 mcg/hour patch marketed as Bu'7rans (Bu-trans), where the 7 indicates its once weekly dosage for pain in osteoarthritis.
Pharmacology and pharmacokinetics
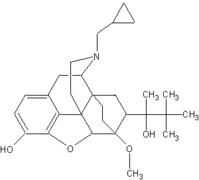
Buprenorphine is a thebaine derivative, and its analgesic effect is due to partial agonist activity at μ-opioid receptors. Buprenorphine is also a κ-opioid receptor antagonist. The partial agonist activity means that opioid receptor antagonists (e.g., an antidote such as naloxone) only partially reverse the effects of buprenorphine.
Buprenorphine hydrochloride is administered by intramuscular injection, intravenous infusion, via a transdermal patch, or as a sublingual tablet. It is not administered orally, due to very high first-pass metabolism. Buprenorphine is metabolised by the liver, via the CYP3A4 isozyme of the cytochrome p450 enzyme system, into norbuprenorphine (by N-dealkylation) and other metabolites. The metabolites are further conjugated with glucuronic acid and eliminated mainly through excretion into the bile. The elimination half-life of buprenorphine is 20.4–72.9 hours (mean 34.6).
Clinical use
Buprenorphine is indicated for the treatment of moderate to severe pain, peri-operative analgesia, and opioid dependence. It has a longer duration of action than morphine, and sublingual tablets offer an analgesic effect for 6 to 8 hours. (Joint Formulary Committee, 2004) Australian guidelines recommend against the use of buprenorphine as an analgesic because: its effect is not reversed by naloxone, it may precipitate withdrawal symptoms in people dependent on other opioids, and it may cause dependence itself and has potential for misuse. (Rossi, 2005) When used for opioid dependence, buprenorphine remains effective in the body for up to 48 hours, curbing withdrawal symptoms and counteracting other opioids that may be administered to the patient (licitly or illicitly).
Read more at Wikipedia.org