Objective: To assess the effects of a norepinephrine-induced vasoconstriction on renal function in septic and nonseptic patients.
Design: Open-label prospective study.
Setting: Medical-surgical ICU in an urban teaching hospital.
Patients: Fourteen patients with septic shock and 12 uninfected patients with head trauma (Glasgow coma score, < 8).
Interventions: Patients received norepinephrine infusion to increase systemic vascular resistance index (SVRI), and to raise mean arterial BP (MAP) to > 70 mm Hg in the septic group and cerebral perfusion pressure (CPP) to > 70 mm Hg in the head trauma group.
Measurements and main results: MAP and SVRI increased in both groups (p < 0J)01), and CPP significantly increased in the head trauma group (p < 0.001). The cardiac index was not mudified in either group. Norepinephrine infusion reestablished urine flow in 12 of the 14 septic patients (p < 0.001), with a decrease in serum creatinine levels (p < 0.001) and an increase in creatinine clearance rate (p < 0.001) after 24 h. Urine parameters were not affected in the head trauma group.
Conclusion: Within the limitation of the present study, norepinephrine administration induces a marked vasoconstriction in septic and nonseptic patients. Norepinephrine has positive effects on renal function in septic patients but has no significant effect on the same urinary parameters when administered to uninfected patients with normal renal function.
Key words: kidney; norepinephrine; renal blood flow; septic; shock
Abbreviations: ARF = acute renal failure; Ccreat = creatinine clearance; CPP = cerebral perfusion pressure; ICP = intracranial pressure; MAP = mean arterial pressure; PAOP = pulmonary artery occlusion pressure; RBF = renal blood flow: RVR = renal vasular resistance Screat = serum creatinine; SVBI--systemic vascular resistance index: Ucreat = urine creatinine; UF = urine flow
**********
Septic shock patients experience a hemodynamic syndrome that is characterized by systemic hypotension despite the administration of aggressive fluid resuscitation) In order to counteract the generalized vasodilatation of vascular beds, potent systemic vasopressor agents such as norepinephrine can be used to restore an acceptable MAP. (2-6) Secondary ])rain injuries occurring after severe head trauma have been shown to be deleterious, (7,8) One of the main goals of therapy is to maintain cerebral perfusion pressure (CPP) at > 70 mm Hg. (9,10) Consequently, the use of vasoactive drags such as norepinephrine is recommended. (8,11) Surprisingly, the visceral effects of catecholamines administered after severe head trauma have been poorly studied.
In this clinical setting, which is at variance with sepsis and septic shock, there is no vasodilation of the vascular bed and there is a potentially higher risk of adversely affecting the renal vascular bed than in septic patients. We hypothesized that norepinephrine would act differently under septic and nonseptic conditions, as has been shown in normal and endotoxemic dogs. (12) The aim of this study was to assess the effects on renal function of norepinephrine administered to increase mean arterial pressure (MAP) and systemic vascular resistance index (SVBI) in septic shock patients, and CPP in head trauma patients.
MATERIALS AND METHODS
Tile present study was approved by the Hospital Ethics Committee of our institution, and informed consent was obtained from next-of-kin.
Patient Eligibility
During a 16-month period, 14 consecutive patients (10 men and four women; mean [[+ or -] SD] age, 51 -+ 12 years) with septic shock were prospectively studied, These patients were consecutively admitted to the 16-bed general ICU of Nord Hospital, Marseilles University Hospital System, No patients were excluded from the study. Following the American College of Chest Physicians/Society for Critical Care Medicine Consensus Conference on sepsis and organ failure, (1) septic shock was defined as sepsis-induced hypotension persisting despite adequate fluid resuscitation, with the presence of hypoperfusion abnormalities or organ dysfunction (ie, oliguria of < 30 mL/h, lactic acidosis, and alteration in mental status evaluated without sedative drugs). Sepsis was defined by two or more of the following conditions: temperature, > 38[degrees]C or < 36[degrees]C; heart rate, > 90 heats/rain; respiratory rate, > 20 breaths/min or the need for mechanical ventilation; and WBC count, > 12,000 cells/[micro]L or < 4,000 cells/[micro]L. The causes of septic shock were bacterial pneumonia (10 patients) and peritonitis (4 patients).
During the same time period, 12 patients with severe head trauma (Glasgow coma scale, < 8) were evaluated (nine men and three women; mean age, 32 [+ or -] 9 years). These patients had no traumatic lesions other than head trauma and were considered to be free of any infection by the medical staff. They also had to be free of salt-wasting syndrome.
General Supportive Measures
All patients with septic shock received broad spectrum antibiotic coverage, usually a [5-1aetam and an aminoglycoside. Vancomycin was added when the presence of methicillin-resistant staphylococci was suspected. Patients did not receive steroids. Respiratory" support was required in all septic shock patients because of severe hypoxemia. Acute pneumonia was found in 10 patients, and ARDS was found in the remaining patients. Tidal volume, respiratory rate, and fraction of inspired oxygen were adjusted with the objective of keeping Pa[O.sub.2] at > 70 mm Hg.
Before inclusion, all patients with head trauma were managed according to our ICU guidelines for severe head trauma patients. (8) They were sedated with a combination of midazolam (0.03 to 0.06 mg/kg/h) and sufentanil (0.2 to 0.4 [micro]g/kg/h), and received mechanical ventilation to maintain [Paco.sub.2] between 35 and 38 mm Hg and arterial oxygen saturation at > 95%. Intracranial pressure (ICP) was measured using an intraparenchymal electromagnetic transducer-tipped catheter (Codman; Raynham, MA) attached to the bedside monitor and calibrated to zero in air prior to insertion through the bolt. CPP was calculated as MAP--ICP. Episodes of intracranial hypertension were treated when they lasted for more than 5 rain and in the absence of noxious stimulation. The increase in ICP (to > 25 mm Hg), or the decrease in CPP (to < 79 into Hg) were managed with the following stepwise approach: (1) hemodynamic stabilization; (2) elevation of the head to a maximum of 30[degrees]; (3) sedation with analgesic medication (ie, sufentanil and midazolam); (4) artificial ventilation with controlled hyperventilation (Pace2, 32 to 35 mm Hg); (5) osmotherapy with mannitol (0.25 to 1 g/kg administered IV) or 23.4% saline solution (30 mL administered W over 20 min); and (6) administration of barbiturate (ie, thiopental) or propofol until the patient underwent burst suppression EEG. Transcranial Doppler ultrasonography for the evaluation of middle cerebral artery flow velocities was performed in patients with ICP increases to determine their management.
Hemodynamic Management
All septic shock and head trauma patients were monitored as follows: hemodynamic and oxygen-derived data were obtained from an arterial catheter (Arrow International; Reading, PA), an oxtimetric pulmonary artery catheter (Swan-Ganz catheter, 7.5 F; Baxter Edwards Critical; Irvine, CA), making it possible to continuously record cardiac output and to measure the usual hemodynamic variables (ie, mean pulmonary arterial pressure, right arterial pressure, and pulmonary artery occlusion pressure [PAOP]), and a pulse oximeter (Oxinet N-7500; Nellcor; Hayward, CA). Heart rate and intravascular pressures were recorded continuously (Merlin; Hewlett-Packard; Palo Alto, CA). SVRI was calculated as the MAP minus right atrial pressure, divided by cardiac index, and multiplied by 80.
Initially, septic shock patients with low preload, estimated from PAOP, were given fluid resuscitation with colloid (hydroxyethyl starch, in 6% solution of nomad saline solution) and crystalloid (lactated Ringer solution) with the aim of obtaining a PAOP between 12 and 15 mm Hg. After fluid challenge, all patients remained in shock with oliguria and a MAP of [less than or equal to] 60 mm Hg. Then, norepinephrine therapy was started at a dose of 0.5 [micro]g/kg/min, with increments of 0.3 [micro]g/kg/min, to a maximal dose of 5.0 [micro]g/kg/min. The aim of therapy was to achieve and maintain MAP at [greater than or equal to] 70 mm Hg and venous oxygen saturation at [greater than or equal to] 70%. The norepinephrine infusion was continued until the resolution of septic shock or death occurred.
The head trauma patients were resuscitated according to our ICU guidelines (ie, until a CPP of 70 mm Hg was attained). Ira this setting, norepinephrine is given when the CPP goal is not met despite fluid resuscitation up to a PAOP of 12 mm Hg.
Assessment of Renal Function
An indwelling urinary catheter was inserted into each patient. Urine was collected in a urinometer. Urine samples for 24-h creatinine clearance (Ccreat) were collected and blood was drawn for serum creatinine (Screat) measurement at the same time (ie, at the end of the urine collection period). Urine creatinine (Ucreat) and Screat levels were measured by an antoanalyzer using the Jaffe method. Measurements of Ucreat (in milligrams per deciliter), urine flow (UF) rate (in milliliters per minute), and Screat (in milligrams per deciliter) were used to calculate the Ccreat (in milliliters per minute) by the following formula: Ccreat = (Ucreat X UF rate)/Screat. The Ccreat that had been determined the day before the ICP catheter was inserted was used as the control. In septic patients, the control value of Ccreat was estimated from the formula (described lay Cockeroft trod [Gault.sup.13]) Ccreat = ([149 mL/min - age] x weight)/ (72 X Screat) (1.5% less in women), where age is given in years and weight signifies body weight (in kilograms). All reported clearances were corrected ff)r be@ surface area by dividing the calculated body surface area by 1.7:3 [m.sup.2].
Statistical Analysis
Data are reported as the mean [+ or -] SD. A paired Student t test or analysis of variance was used where appropriate. A p level of < 0.0,5 was chosen to reject the null hypothesis.
RESULTS
The mean maximum dose of norepinephrine used was 1.3 [+ or -] 0.3 [micro]g/kg/min in septic shock patients and 0.3 [+ or -] 0.1 [micro]g/kg/min in head trauma patients. Seven septic shock patients and 11 head trauma patients were discharged from the hospital. Changes in hemodynamic variables are presented in Table 1. A significant increase in MAP and SVRI was observed in the septic shock and the head trauma groups. CPP rose significantly in the head trauma group. SVRI was significantly increased in both groups (Table 1).
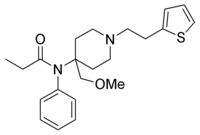
In the septic shock group, the restoration of normal tissue perfusion pressure was followed by a dramatic improvement in UF (Table 2). In 10 of these patients, UF increased by > 50 mL/h in the first hour after the normalization of MAP. UF was reestablished in the third hour in two other patients. Oliguria persisted in two septic shock patients despite subsequent treatment with low-dose dopamine and furosemide. The reestablishment of UF was maintained over time (Table 2) and was accompanied by a significant decrease in Screat (p < 0.001) and a significant increase in Ccreat (p < 0.001) [Fig 1]. In the head trauma group, the infusion of norepinephrine did not affect UF over the study period (Table 2). No significant changes in Screat and Ccreat were observed after a 24-h period of norepinephrine infusion compared with the baseline data (Fig 1).
[FIGURE 1 OMITTED]
DISCUSSION
Norepinephrine induces vasoconstriction visibly in many vascular beds (eg, the skin), and could therefore alter visceral blood flow and, more especially, renal blood flow (RBF), impairing organ function. Given the high risk of acute renal failure (ARF) in septic shock patients, many physicians are reluctant to use norepinephrine because of the risk of precipitating AI1F due to decreased RBF. In experimental models, norepinephrine has been demonstrated to cause ischemia-induced ARF in rats.14 However, it is not clear whether the same scenario of vasopressorinduced visceral hypoperfusion actually occurs in sepsis, which is characterized by marked vasodilation related to muscle [alpha]-adrenergie receptor hyporesponsiveness or massive nitric oxide production. (15, 16)
The main findings of the present study support the hypothesis that norepinephrine-induced vasoconstriction, when norepinephrine is administered in relevant dosages that significantly increase MAP and SVRI, affects renal function differentially under septic and nonseptic conditions. When normal hemodynamic status exists (ie, normal MAP, cardiac index, SVRI, and PAOP), norepinephrine administered to raise MAP by 20% does not affect UF or glomerular filtration. In contrast, when severe vasodilation (ie, low SVRI and high cardiac index) affects systemic circulation, the infusion of norepinephrine, which is required to restore tissue perfusion pressure, is accompanied by a restoration of UF, a decrease in Screat, and an increase in Ccreat in septic patients. The beneficial effect of norepinephfine in septic patients is in agreement with the conclusions of several clinical reports. (17-23) The doses of norepinephrine used in the present study were different in the two investigated groups. The doses used in the head trauma group were similar to those recommended in the literature for such patients. (8-11) Higher doses were required in the septic shock patients, a situation that is related to the downregulation of [alpha]-adrenergie receptors observed in such patients. Vascular hyporeactivity has been well-documented in such patients because of the presence of high circulating levels of vasodilator mediators such as nitric oxide. (15,16) Such a discrepancy between the norepinephrine doses required in septic and nonseptic patients to achieve a significant effect on MAP was therefore expected. We do not think that this difference in doses affected the results of the present study since a marked effect on MAP and SVRI was observed in both groups. All patients experienced a significant vasoconstriction of their vascular bed.
When improperly used, norepinephrine can induce ABF following intense renal vasoconstriction. (14) However, this finding has only been noted after the infusion of the drug directly into the renal artery (and not via the systemic route) at clinically relevant doses. (14-17, 24) In addition, the closes used in animal models of norepinephrine-induced At/F are well beyond those used in clinical practice.
Conversely, our findings are in agreement with those of Anderson et al, (25) who infused conscious dogs with doses of norepinephrine of 0.2 to 0.4 [micro]g/kg/min and found that RBF increased and renal vascular resistances (RVRs) decreased. (25) Such renal vasodilatation was not affected by pretreatment with indomethaein, propranolol, or angiotensin-converting enzyme inhibitors. However, efferent autonomic sympathetic nerve blockade with pentolinium abrogated norepinephrine-induced renal vasodilatation. The investigators concluded that most of this effect could be attributed to the increase in systemic BP, which, in turn, decreases renal sympathetic tone. This conclusion is in agreement with that in a study by Zhang et al, (26) which showed that norepinephrine did not induce a decrease in RBF in endotoxemic dogs. In an elegant physiologic study conducted in dogs, Bellomo et a1 (12) demonstrated that under endotoxemic conditions, norepinephrine infusion in creased RBF and renal perfusion pressure. By using a crossover design, they were also able to demonstrate that when normal circulatory status exists in otherwise unstressed circulation, the drug failed to increase RBF, despite increasing MAP. The interpretation of' the authors was that the renal vasculature is hyporesponsive under endotoxemic conditions. The addition of norepinephrine further decreases renal vascular ohmic resistance and also decreases renal vascular critical closing pressure, and these combined effects increase RBF to a constant perfusion pressure. (12)
Schaer et al (27) also reported the renal effects of norepinephrine in dogs. They found that although RVR, appeared to increase, RBF progressively rose with increasing doses of norepinephrine up to 1.6 [micro]g/kg/min. One limitation of their study was that baseline MAP was 151 mm Hg and that the infusion of the drug increased MAP to 200 nun Hg. Thus, the clinical relevance of these data is minimal, but the important message is that, as long as the cardiac index is maintained, increasing MAP with norepinephrine is not deleterious to renal function. To conclude with the experimental literature, under endotoxemic conditions, the infusion of norepinephrine to increase MAP would appear to be beneficial to renal function and is ,'elated to the favorable effects on RVR, RBF, and renal perfusion pressure.
There are no studies available that were designed to measure RBF or RVR. However, many studies (17-23) have supported the notion that norepinephrine infusion improves UF and Ccreat in septic shock patients. In patients with hypotension and hypovolemia (eg, during hemorrhagic shock), norepinephrine and other vasoconstrictor agents have severe detrimental effects on renal hemodynamics. Despite the constant improvement in BP, RBF did not increase, while RVR continued to rise in an animal model in dogs. (28) Renal ischemia worsens, which has been demonstrated by data showing a marked decrease in renal tissue oxygen tension. (28) However, there is little information in the literature on the renal effects of norepinephrine in head trauma patients. Despite this lack of information, the infusion of catecholamines has been recommended in guidelines (8-10) for maintaining adequate CPP in head trauma patients. Our results highlight the notion that the infusion of norepinephriue in order to increase MAP in head trauma patients without sepsis has no detrimental impact on renal function, and one can speculate that this is because norepinephrine was infused after fluid resuscitation was performed. This point is of crucial importance since hypovolemia plays a central role in the development of ARF during hypovolemic shock as well as during sepsis, thus the restoration and maintenance of normovolemia before and during the administration of norepinephrine should always be the first-line therapy.
The situation is different in patients with hyperdynamic septic shock. It is speculated that the main reason for the decrease in UF is lowered renal glomerular perfusion pressure. Since norepinephrine has a greater effect on efferent arteriolar resistance and increases the filtration fraction, the normalization of RVRs could effectively reestablish UF. The importance of this during norepinephrine infusion was shown by Schaer et al. (27) Thus, during norepinephriue therapy, cardiac index should be normal or elevated to maintain normal RBF. In septic shock patients, norepinephrine treatment is aimed at restoring vascular resistances to the normal range. It is probably wise to keep SVRI slightly below normal with norepinephrine to prevent excessive vasoconstriction in some vascular beds. This could be deleterious to the heart, and excessive vasoconstriction ,nay stress the myocardium. If the left ventricle can increase its contractile force only to a limited degree, then stroke volume cat, decrease along with cardiac output and oxygen delivery. This can also be deleterious to the kidney, and excessive vasoconstriction could worsen renal ischemia. In case there is concert, about the risk associated with the insertion and use of a pulmonary artery catheter, (29) norepinephrine should be titrated against MAP to target a MAP between 65 and 70 mm Hg, and perhaps higher in elderly patients or patients with known or suspected arterial atheromatosis.
In the present study, we hypothesized that norepinephrine infusion would act differently in septic and nonseptic patients. Indeed, it, our septic patients we were able to reproduce the favorable effects of a norepinephrine-induced increase in MAP (ie, increased UF and decreased Ccreat). These effects are probably supported by concomitant increases in RBF and the glomerular filtration rate. Such effects were not observed in the control situation (ie, patients without basal alterations of their hemodynamic status). However, the infusion of norepinephrine did not have a detrimental effect on renal function in head trauma patients without sepsis within the limitations of the present study. One limitation of the present study is that we studied only a relatively small number of patients. We focused on the evolution of hemodynamic parameters and measures of organ function and obtained clear and reliable data, but further studies are needed to confirm our findings.
One point that should be discussed is the use of aminoglycosides in the empirical antibiotic treatment of our septic shock patients. Indeed, these drugs may impair renal function, especially in patients with low intravascular volume. One the other hand, aminoglycosides are of great interest for empirical treatment in the ICU. They are fast and reliable bactericidal agents, and aminoglycoside resistance is low in the ICU. In view of these advantages, potential toxicity can be minimized, and for that reason strict monitoring of serum concentrations (peak and through levels) should be performed. In our institution as well as others, such controls and the use of once-daily regimens can keep renal toxicity as low as [less than or equal to] 5%,30 and renal function always recovers. (31)
One last point that should be discussed is that in our guidelines for the resuscitation of patients who have experienced severe head trauma, a CPP of [greater than or equal to] 70 mm Hg was targeted. Recent data have suggested that there is probably an age-related continuum for the optimal treatment threshold and that values of 60 to 70 mm HE, rather than [greater than or equal to] 70 mm HE, should be considered. Thus, lower doses of vasopressors, including norepinephrine could he used in the future. (32) Moreover, in the present study four patients received hypertonic fluids for the treatment of raised ICP (mannitol, two patients; hypertonic saline solution, two patients). No effects on renal function were observed.
In conclusion, within the limitation of the present study' and in contrast to what has been observed in patients with no alteration of their circulatory state, norepinephrine-induced vasoconstriction is accompanied by beneficial effects on renal function. Following the restoration of MAP, UF is restored and Ccreat is improved.
REFERENCES
(1) Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis aim organ failure and guidelines for the use of innovative therapies in sepsis: the ACCP/SCCM Consensus Conference Committee; American College of Chest Physicians/Society of Critical Care Medicine, Chest 1992; 101:1644-1655
(2) Schreuder WO, Schneider AJ, Groeneveld ABJ, et al. Effect of dopamine vs norephinephrine or dopamine for the treatment of hyperdynamic septic shock? Chest 1989; 95:1282-1288
(3) Martin C, Papazian L, Perrin G, et al. Norepinephrine or dopamine for the treatment of hyperdynamic septic shock Chest 1993; 103:1826-1831
(4) Dasta JF. Norepinephrine in septic shuck: renewed interest in an old drug. DICP 1990; 24:153-156
(5) Martin C, Viviand X, Leone M, et M. Effects of norepinephrine on the outcome of septic shock. Crit Care Med 2000; 28:2758-2765
(6) Mayer J, Skelton J, Mills 1,. Norepinephrine: effect in normal subject; use in treatment of shock unresponsive to other measures. Ann J Med 1953; 15:330-343
(7) Chesnut RM. Secondary brain insults after head injury: clinical perspectives. New Horiz 1996; 3:366-375
(8) Bullock RN, Chesnut RM, Clifton G, et ah Guidelines for the management of severe head injury. Eur J Emerg Med 1996; 2:109-127
(9) Rosner MJ, Rosner SD, Johnson AH, Cerebral perfusion pressure: management protocol and clinical results. J Neurosurg 1995; 83:949-962
(10) Myburgh JA, Lewis SB. Goal directed therapy in neuro-trauma. In: Vincent JL, ed. Yearbook of intensive care and emergency medicine, Berlin, Germany: Springer Verlag, 1996; 716-730
(11) Ract C, Vigu6 B. Comparison of the cerebral effects of dopamine and norepinephrine in severely head-injured patients. Intensive Care Med 200i; 27:101-106
(12) Bellomo R, Kellum JA, Winiewski SR, et al, Effects of norepinephrine on the renal vasculature in normal and endotoxemic dogs, Am J Respir Crit Care Med 1999; 159: 1186-1192
(13) Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976; 16:31-37
(14) Cronin RA, Erickson M, De Torrente A, et al. Norepinephrine induced acute renal failure: a reversible ischemic model of acute renal failure. Kidney Int 1978; 14:187-190
(15) Schott CA, Gray GA, Stoclet JC. Dependance of endotoxin-induced vascular hyporeactivity on extracelhdar L-arginine. Br J Pharmacol 1993:108:38-43
(16) Lilbourn RO, Gross SS, Jubran A, et al N-methyl-L-arginine inhibits tumor necrosis factor induced hypotension: implications tbr the involvement of nitric oxide. Proc Natl Acad Sci U S A 1990; 87:3629-3632
(17) Bellomo R, Di Giantomaso D. Noradrenaline and the kidney: friends or foes? Crit Care 2001:5:294-298
(18) Desjars P, Pinaud M, Potel G, et al. A reappraisal of norepinephrine therapy in human septic shock. Crit Care Med 1987; 15:134-137
(19) Meadows D, Edwards JD, wilkins RG, etal, Reversal of intractable septic shock with norepinephrine therapy. Crit Care Med 1988; 16:663-666
(20) Martin C, Eon B, Saux P, et al. Renal effects of norepinephrine used to treat septic shock patients, Crit Care Med 1990; 18:282-285
(21) Desjars P, Pinaud M, Bugnon D, et al. Norepinephrine therapy has no deleterious renal effects in human septic shock. Crit Care Med 1990:18:1048-1049
(22) Rudis MI, Basha MA, Zarowitz BJ. Is it time to reposition vasopressors and inotropes in sepsis? Crit Care Med 1996; 24:525-537
(23) Redl-Wenzel EM, Armbruster C, Edelmann G, el al. The effects of norepinephrine on hemodynamics and renal function in severe septic shock states. Intensive Care Med 1993: 19:151-154
(24) Cronin RE, De Torrente A, Miller PD. et al. Pathogenic mechanisms in nearly norepinephine induced acute renal failure: functional and histological correlates of protection. Kidney Int 1978; 14:115-125
(25) Anderson WP, Korner PI, Selig SE. Mechanisms involved in the renal responses to intravenous and renal artery infusions of noradrenaline in conscious dogs. J Physiol 1981; 321:21-30
(26) Zhang H, Smail N, Cabral A, et al. Effects of norepinephrine on regional blood flow and oxygen extraction capabilities during endotoxemic shock. Am J Respir Crit Care Med 1997; 155:1965-1971
(27) Schaer EL, Fink MP, Parino JE. Norepinephrine alone versus norepinephrine plus low dose dopamine: enhanced renal blood flow with combination pressor therapy. Crit Care Med 1985; 13:492-496
(28) Mills LC, Moyer JH, Handley CA. Effects of various sympathomimetic drugs on renal hemodynamics in normotensive and hypotensive dogs. Am J Physiol 19611; 198:1279-1285
(29) Practice guidelines for pulmonary artery catheterization. Anesthesiology, 2003; 99:988-1014
(30) Bartal C, Danon A, Schlaeffer F, et al, Pharmacokinetic dosing of aminoglycosides: a controlled trial. Ann J Med 2003; 114:194-198
(31) Buijk SE, Mouton JW, Gyosens IC, et al. Experience with a once-daily dosing program of aminoglycosides in critically ill patients. Intensive Care Med 2002; 28:936-942
(32) Cerebral perfusion pressure. Crit Care Med 2003; 31:S447-S449
* From the Department of Anesthesiology and Intensive Care Medicine and Trauma Center, Marseilles University Hospital System, Marseilles School of Medicine, Marseilles, France.
Manuscript received July 31, 2003; revision accepted February 11, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Claude Martin, MD, FCCP, Departement d'Anesthesie et de Reanimation, CHU Nord, 13915 Marseille cedex 20, France; e-mail: claude.martin@ap-hm.fr
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group