Study objectives: The aim of this study was to elucidate the clinical characteristics and treatment responses of tuberculosis developing in patients receiving anticancer chemotherapy. Design: Retrospective case-control study.
Setting: The Seoul National University Hospital, a tertiary referral hospital in South Korea. Patients: From January 1, 2000, to July 31, 2004, patients with tuberculosis detected during the course of anticancer chemotherapy were enrolled as cases. Age- and sex-matched tuberculosis patients without any malignant disease were selected as control subjects.
Measurements and results: Twenty-four patients and 48 control subjects were enrolled. Their mean [+ or -] SD age was 56.3 [+ or -] 14.3 years, and the male-to-female ratio was 3:1. The most common malignancy was gastric cancer (43%). Lymphoma (17%), lung cancer (8%), and head and neck cancer (8%) were also common. In both groups, the lung was the most common site of tuberculosis involvement (87.8% and 79.2%, retrospectively). The presence of scar tissue suggesting old tuberculosis on radiography was more common in patients with tuberculosis receiving anticancer chemotherapy (66.7% vs 43.8%, p = 0.07). No difference in radiographic severity was observed between groups. A regimen based on first-line antituberculosis drugs was started in all subjects. Frequency of completion of the expected antituberculosis chemotherapy was lower in patients with tuberculosis developing with anticancer chemotherapy (58.3% vs 79.2%, p = 0.02), but it was not different after excluding the loss due to progression of underlying malignancies. Bacteriologic/radiographic responses to treatment and toxicity of antituberculosis medication sufficient to change or stop treatment were not different in both groups. Conclusions: With regard to radiographic and clinical responses to antituberculosis treatment, tuberculosis developing during anticancer chemotherapy is not clinically different from tuberculosis developing in ordinary situations. Findings in this study suggest that anticancer chemotherapy is not an obstacle in treating tuberculosis.
Key words: cancer; chemotherapy; tuberculosis
**********
The World Health Organization estimates that one third of the population of the world has Mycobacterium tuberculosis infection. Eight million new cases of active tuberculosis are diagnosed annually, and 2 million people die of tuberculosis each year, (1) and tuberculosis is the foremost cause of death from a single infectious agent among adults, (2)
However, not all patients with M tuberculosis infection will acquire clinical tuberculosis. (3) Well-known risk factors for tuberculosis include advanced HIV infection, chronic renal failure, poorly controlled diabetes, infliximab therapy, old healed tuberculosis, silicosis, being underweight, and gastrectomy. (4-13) In addition, some malignant diseases such as malignant lymphoma, lung cancer, head and neck cancer, leukemia, and stomach cancer have been reported to be associated with the development of tuberculosis. (14-17)
Although the risk for tuberculosis increases in patients with malignant disease, the clinical response of tuberculosis to antituberculosis treatment in patients receiving anticancer chemotherapy has not been known well, except for a few case series (18-21) involving a small number of patients showing inconsistent results. The aim of this study was to elucidate the clinical characteristics and treatment responses of tuberculosis in patients receiving anticancer chemotherapy.
METHODS AND MATERIALS
Study Setting and Subjects
Patients with tuberculosis detected during anticancer chemotherapy or < 1 month after completion of anticancer chemotherapy, from January 1, 2000, to July 31, 2004, at Seoul National University Hospital, a tertiary referral hospital in South Korea, were enrolled as a case group. We excluded multidrug-resistant tuberculosis in the analysis to avoid bias caused by the cases. Two times the number of age- and sex-matched control subjects were randomly selected from among the tuberculosis patients without any malignant disease from 880 tuberculosis patients who had tuberculosis diagnosed and were treated during the same period at Seoul National University Hospital. In both groups, patients with any of the risk factors for reactivation of tuberculosis such as HIV infection, silicosis, diabetes mellitus, chronic renal diseases, or immunosuppressive treatment except corticosteroids included in the anticancer chemotherapeutic regimen were excluded. The diagnosis of tuberculosis was made on the basis of bacteriologic, pathologic, or clinical findings. We retrospectively reviewed the clinical records, the results of bacteriologic examination, and radiographs of the enrolled patients.
Statistical Analysis
Data were analyzed by comparing patients with tuberculosis detected during anticancer chemotherapy with tuberculosis patients without any evidence of malignancy. Statistical analysis was performed using statistical software (SPSS for Windows, version 11.0; SPSS; Chicago, IL). The [chi square] test or Fisher Exact Test (if the expected number was less than five in at least one cell) for comparison of categorical variables and t test for comparison of continuous variables were applied. The statistical significance was determined at p < 0.05.
RESULTS
Characteristics of the Study Population
Twenty-eight patients with tuberculosis detected during anticancer chemotherapy or < 1 month after completion of anticancer chemotherapy were enrolled. Among them, three patients were excluded from the analysis because they had diabetes mellitus. In addition, one patient with multidrug-resistant M tuberculosis was also excluded. Forty-eight age- and sex-matched tuberculosis patients without malignant disease or any other risk factors for development of tuberculosis were enrolled as a control group.
The mean [+ or -] SD ages of patients with tuberculosis receiving anticancer chemotherapy and patients without malignant disease were 56.3 [+ or -] 14.1 years and 56.3 [+ or -] 14.5 years, respectively. The male-to-female ratio was 3:1 in both groups. The baseline characteristics were similar in both groups except for lower leukocyte counts in tuberculosis patients receiving anticancer chemotherapy than in control patients (5,792 [+ or -] 2,085/[micro]L vs 7,801 [+ or -] 3,647/[micro]L, p = 0.02; Table 1). Advanced gastric cancer was the most common malignancy (10 patients, 41.7%), and lymphoma (4 patients, 16.7%), lung cancer (2 patients, 8.3%), head and neck cancer (2 patients, 8.3%), breast cancer (2 patients, 8.3%), and leukemia (2 patients, 8.3%) followed in order. Anticancer chemotherapy was prescribed as a curative modality in seven patients (29.2%), an adjuvant modality in seven patients (29.2%), a palliative modality in six patients (25%), or a neoadjuvant modality in four patients (16.7%). According to the World Health Organization definition for the response evaluation of cancer treatment, (22) the status of the underlying 22 solid tumors containing lymphoma at the time of diagnosis of tuberculosis was as follows: no evidence of disease in six patients (27.3%), progressive disease in six patients (27.3%), stationary disease in five patients (22.7%), and partial remission in five patients (22.7%).
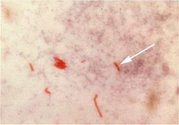
Clinical and Radiographic Characteristics of Tuberculosis Detected During Anticancer Chemotherapy
Pulmonary tuberculosis was the most common type of tuberculosis in the patient group and the control group (87.5% and 79.2%, respectively). The proportion of tuberculosis with a cavitary lesion (28.6% vs 13.6%, p = 0.28) or disease involving more than two lobes (42.9% vs 34.2%, p = 0.51) was not different in both groups. Scarring observed on chest radiographs suggesting old healed tuberculosis before the development of clinical tuberculosis was more common in patients receiving anticancer chemotherapy in trend (67% vs 44%, p = 0.07; Table 2).
Clinical Course and Response to Antituberculosis Treatment
Antituberculosis chemotherapy was started with a rifampicin-based regimen in all patients, and the mean duration of treatment was 10.1 [+ or -] 2.3 months in patients receiving anticancer chemotherapy and 9.5 [+ or -] 2.7 months in patients without malignant disease (Table 3). The treatment was performed based on daily self-administered therapy. Although the overall proportion of patients who completed the antituberculosis therapy was lower in patients receiving anticancer chemotherapy (p = 0.02), the lost proportion (including those who died or for whom contact was lost during follow-up) was larger in patients receiving anticancer chemotherapy (41.7% vs 20.8%, p = 0.02). All five deaths of patients receiving anticancer chemotherapy resulted from progression of the underlying malignancies, not from the aggravation of tuberculosis. M tuberculosis culture results were converted to negative in all patients with available follow-up cultures. The time to bacteriologic conversion and radiographic responses to antituberculosis treatment as well as the frequency of severe side effects from antituberculosis drugs were not different in both groups (Table 3).
DISCUSSION
Malignant disease and anticancer chemotherapy are risk factors for the development of tuberculosis or poor prognosis in tuberculosis patients. (16,18,23) Impairment of host defense mechanisms, poor nutrition, and debility have been proposed as attributing factors for the higher incidence of tuberculosis in patients with some malignant diseases. (18) The trend that the presence of healed scar suggesting previous tuberculosis on chest radiography is more common in tuberculosis patients receiving anticancer chemotherapy, and new lesions were extended from there or contained healed scar in our study (p = 0.07), which suggests tuberculosis development by reactivation may reinforce the concept of anticancer chemotherapy as a risk factor for the development of tuberculosis. However, we could not confirm any differences in clinical manifestation and treatment response between tuberculosis patients with or without anticancer chemotherapy, despite previous case series (18,19,23,24) suggesting that some cases of tuberculosis manifest as more severe forms associated with higher fatality in cancer patients.
This lack of difference in clinical characteristics in our study could be explained in several ways. First, all patients enrolled in this study were receiving cyclic anticancer chemotherapy. The immune suppression caused by cyclic anticancer chemotherapy might not be as severe as the suppression induced by long-term continuous use of anticancer agents or long-term steroid treatment. (25,26) Second, considering that the risk of infection could be directly related to the severity and duration of neutropenia, (27) the fact that most patients (22 patients, 91.7%) with malignant disease in this study had solid tumors causing relatively modest immune suppression rather than hematologic malignancies (28) could be another reason for good responses to antituberculosis treatment. Third, because malnutrition plays a crucial role in the development of tuberculosis in cancer-free patients and cancer patients, (10-11, 18) the absence of nutritional deficiency, judged by the levels of cholesterol and protein and body mass index in tuberculosis patients receiving anticancer chemotherapy, could explain the lack of difference in clinical characteristics between the two groups in our study.
For the treatment of tuberculosis developing in an immunocompromised host, individualized therapeutic decisions are recommended after considering the severity of tuberculosis and the response to treatment, (29) or prolonged antituberculosis treatment has been performed in some centers. (30) However, in our study, there was no difference in the culture conversion rate and radiographic responses with antituberculosis treatment, although the time to culture conversion was longer in tuberculosis patients receiving anticancer chemotherapy (p = 0.09). When considering that anticancer chemotherapy is not a situation in which immunosuppressive agents are administered continuously for long periods, that treatment response to antituberculosis medication has been reported to be fairly good even in patients with AIDS, (29,31,32) and that our study showed good responses to antituberculosis treatment in patients receiving anticancer chemotherapy, the adequate duration of antituberculosis treatment could be the same as that in tuberculosis patients without cancer.
CONCLUSION
With regard to radiographic and clinical response to treatment, tuberculosis developing during anticancer chemotherapy is not different from tuberculosis developing under ordinary situations. Our findings suggest that anticancer chemotherapy is not an obstacle to treating tuberculosis.
Manuscript received January 24, 2005; revision accepted April 20, 2005.
REFERENCES
(1) Dye C, Scheele S, Dolin P, et al. Consensus statement: global burden of tuberculosis; estimated incidence, prevalence, and mortality by country; WHO Global Surveillance and Monitoring Project. JAMA 1999; 282:677-686
(2) Dolin PJ, Raviglione MC, Kochi A. Global tuberculosis incidence and mortality during 1990-2000. Bull World Health Organ 1994; 72:213-220
(3) Murray CJ, Styblo K, Rouillon A. Tuberculosis in developing countries: burden, intervention and cost. Bull Int Union Tuberc Lung Dis 1990; 65:6-24
(4) Pablos-Mendez A, Blustein J, Knirsch CA. The role of diabetes mellitus in the higher prevalence of tuberculosis among Hispanics. Am J Public Health 1997; 87:574-579
(5) Keane J, Gershon S, Wise RP, et al. Tuberculosis associated with infliximab, a tumor necrosis factor a-neutralizing agent. N Engl J Med 2001; 345:1098-1104
(6) Ferebee SH. Controlled chemoprophylaxis trials in tuberculosis: a general review. Bibl Tuberc 1970; 26:28-106
(7) Ferebee SH, Mount FW, Murray FJ, et al. A controlled trial of isoniazid prophylaxis in mental institutions. Am Rev Respir Dis 1963; 88:161-175
(8) Cowie RL. The epidemiology of tuberculosis in gold miners with silicosis. Am J Respir Crit Care Med 1994; 150:1460-1462
(9) Kleinschmidt I, Churchyard G. Variation in incidences of tuberculosis, in subgroups of South African gold miners. Occup Environ Med 1997; 54:636-641
(10) Palmer CE, Jablon S, Edwards PQ. Tuberculosis morbidity of young men in relation to tuberculin sensitivity and body build. Am Rev Tuberc 1957; 76:517-539
(11) Edwards LB, Livesay VT, Acquaviva FA, et al. Height, weight, tuberculous infection, and tuberculous disease. Arch Environ Health 1971; 22:106-112
(12) Thorn PA, Brookes VS, Waterhouse JA. Peptic ulcer, partial gastrectomy, and pulmonary tuberculosis. BMJ 1956; 4967: 603-608
(13) Steiger Z, Nickel WO, Shannon GJ, et al. Pulmonary tuberculosis after gastric resection. Am J Surg 1976; 131:668-671
(14) De La Rosa GR, Jacobson KL, Rolston KV, et al. Mycobacterium tuberculosis at a comprehensive cancer centre: active disease in patients with underlying malignancy during 1990-2000. Clin Microbiol Infect 2004; 10:749-752
(15) Kaplan MH, Armstrong D, Rosen P. Tuberculosis complicating neoplastic disease: a review of 201 cases. Cancer 1974; 133:850-858
(16) Ibrahim EM, Uwaydah A, al-Mulhim FA, et al. Tuberculosis in patients with malignant disease. Indian J Cancer 1989; 26:53-57
(17) Karnak D, Kayacan O, Beder S. Reactivation of pulmonary tuberculosis in malignancy. Tumori 2002; 88:251-254
(18) Tubura E. Pulmonary tuberculosis in the compromised host: report of the 30th B series of controlled trials of chemotherapy; Cooperative Study Unit of Chemotherapy of Tuberculosis of the National Sanatoria in Japan. Kekkaku 1991; 66:95-99
(19) Liu SF, Liu JW, Lin MC. Characteristics of patients suffering from tuberculous pleuritis with pleural effusion culture positive and negative for Mycobacterium tuberculosis, and risk factors for fatality. Int J Tuberc Lung Dis 2005; 9:111-115
(20) Tamura A, Hebisawa A, Tanaka G, et al. Active pulmonary tuberculosis in patients with lung cancer. Kekkaku 1999; 74:797-802
(21) Komatsu H, Nagai H, Satou K, et al. Association of active pulmonary tuberculosis and malignant diseases: a clinical study. Kekkaku 1995; 70:281-284
(22) Miller AB, Hoogstraten B, Staquet M, et al. Reporting results of cancer treatment. Cancer 1981; 47:207-214
(23) Dewan PK, Arguin PM, Kiryangova H, et al. Risk factors for death during tuberculosis treatment in Orel, Russia. Int J Tuberc Lung Dis 2004; 8:598-602
(24) Millar JW, Horne NW. Tuberculosis in immunosuppressed patients. Lancet 1979; 1:1176-1178
(25) Garay GE, Pavlovsky S, Sasiain MC, et al. Immunocompetence and prognosis in children with acute lymphoblastic leukemia: combination of two different maintenance therapies. Med Pediatr Oncol 1976; 2:403-415
(26) Gea-Banacloche JC, Opal SM, Jorgensen J, et al. Sepsis associated with immunosuppressive medications: an evidence based review. Crit Care Med 2004; 32(suppl):S578-S590
(27) Bodey GP, Buckley M, Sathe YS, et al. Quantitative relationship between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med 1966; 64:328-340
(28) De Pauw BE, Verweij PE. Infection in patients with hematologic malignancies. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia PA: Elsevier 2005; 3432-3441
(29) Blumberg HM, Burman WJ, Chaisson RE, et al. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med 2003; 167:603-662
(30) Park YS, Choi JY, Cho CH, et al. Clinical outcomes of tuberculosis in renal transplant recipients. Yonsei Med J 2004; 45:865-872
(31) Perriens JH, St. Louis ME, Mukadi YB, et al. Pulmonary tuberculosis in HIV-infected patients in Zaire: a controlled trial of treatment for either 6 or 12 months. N Engl J Med 1995; 332:779-784
(32) El-Sadr WM, Perlman DC, Matts JP, et al. Evaluation of an intensive intermittent-induction regimen and duration of short-course treatment for human immunodeficiency virus-related pulmonary tuberculosis. Terry Beirn Community Programs for Clinical Research on AIDS (CPCRA) and the AIDS Clinical Trials Group (ACTG). Clin Infect Dis 1998; 26:1148-1158
Deog Kyeom Kim, MD; Sei Won Lee, MD; Chul-Gyu Yoo, MD; Young Whan Kim, MD; Sung Koo Hart, MD; Young-Soo Shim, MD; and Jae-Joon Yim, MD
* From the Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine and Lung Institute of Medical Research Center, Seoul National University College of Medicine, Seoul, Republic of Korea.
Correspondence to: Jae-Joon Yim, MD, Department of Internal Medicine, Seoul National University College of Medicine, 28 Yongon-Dong, Chongno-Gn, Seoul, 110-744, Republic of Korea; e-mail: yimjj@snu.ac.kr
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group